Abstract
Objective
To delineate the spectrum of knee injuries associated with sprains and tears of the distal iliotibial band (ITB).
Materials and methods
A retrospective review of 200 random MRI scans undertaken for acute knee trauma was performed. Scans were excluded if there was a history of injury over 4 weeks from the time of the scan, septic arthritis, inflammatory arthropathy, previous knee surgery, or significant artefact. In each scan, the ITB was scored as normal, minor sprain (grade 1), severe sprain (grade 2), and torn (grade 3). The menisci, ligaments, and tendons of each knee were also assessed.
Results
The mean age was 27.4 years (range, 9–69 years) and 71.5 % (n = 143) of the patients were male. The ITB was injured in 115 cases (57.5 %). The next most common soft tissue structure injured was the anterior cruciate ligament (ACL) in 53.5 % of cases (n = 107). Grade 1 ITB injury was seen in 90 of these 115 cases (45 %), grade 2 injury in 20 cases, and grade 3 injury in only five cases. There is a significant association between ITB injury and ACL rupture (p < 0.05), as well as acute patellar dislocation (p < 0.05). There were ten cases of significant posterolateral corner injury, and all were associated with ITB injury, including four ITB tears. Only two cases of isolated ITB injury were seen (1 %).
Conclusions
ITB injury is common in acute knee trauma and is associated with significant internal derangement of the knee, especially cruciate ligament rupture, posterolateral corner injury, and patellar dislocation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Complex knee injuries are frequently seen in clinical practice [1] and MRI is the gold standard for non-invasive assessment of the knee [2]. A recent epidemiological study in the United States showed an incidence of 2.29 knee injuries per 1,000 individuals [3]. The anatomy and biomechanics of the knee are complex [4]. Certain traumatic forces are associated with particular patterns of injury. For instance, flexion valgus with hyperextension is typically associated with anterior cruciate ligament (ACL), medial collateral ligament (MCL), and meniscal injury as well as bone bruising in the lateral femoral condyle [5]. Undiagnosed knee injuries can be debilitating. Prompt and accurate diagnosis is critical.
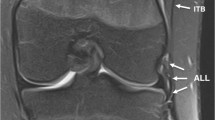
The anatomy of the lateral and posterolateral aspects of the knee are complex and there is marked variability in the nomenclature used to describe their component structures [6]. There is an increasing radiological awareness of the importance of recognizing posterolateral corner injury in acute knee trauma in preventing long-term instability and early osteoarthritis [7]. However, little is documented on abnormalities of the iliotibial band (ITB) as a discrete entity in knee trauma MRI. The iliotibial band or tract is part of the lateral soft tissue structures of the knee joint. The soft tissues of the lateral knee can be considered to form three layers, with the ITB along with the biceps femoris tendon forming the superficial layer, the patellar retinaculum forming the intermediate layer, and the lateral collateral ligament and joint capsule the deep layer [8]. The ITB is a distal continuation of the deep fascia of the thigh (fascia lata), receiving insertions from the gluteus maximus and tensor fascia lata (TFL) muscles, passing over the anterolateral aspect of the thigh and inserting onto Gerdy’s tubercle onto the anterolateral aspect of the proximal tibia (Fig. 1) [9]. The ITB contributes to lateral stability at the knee joint [10].
The normal ITB. Axial T1-weighted MR image of the left upper thigh (a) and coronal PDFS MR image of the left knee (b). The ITB (black arrow) is attached to the TFL muscle anteriorly and gluteus maximus (GM) posteriorly. In the knee, the ITB (white arrow) inserts onto Gerdy’s tubercle (asterisk) on the anterolateral tibia
Isolated ITB abnormalities include ITB friction syndrome [11] and external snapping hip [12], which are not associated with acute injury. However, there is limited information regarding injury of the ITB in acute knee trauma as a discrete structure. The authors performed a systematic retrospective analysis of MRI scans performed after acute knee trauma in order to establish the spectrum of injuries associated with ITB sprains and tears. Given the anterolateral location of the ITB in the knee, we hypothesize that there is an association between ITB injury and posterolateral corner (PLC) and cruciate ligament disruption.
Methods
This was a retrospective observational cross-sectional study. A search was performed on all knee MRI scans in our institution for acute knee trauma between August 2011 and August 2013 using our departmental radiology information database (RIS). Scans were randomly selected from the search results and an initial review was performed. Patients with a clinical history of acute knee trauma within 4 weeks of the scan date were included in the study. Scans were excluded when there was a previous history of knee surgery, septic arthritis, inflammatory arthropathy, or significant motion artefact. Basic demographic data on each patient were obtained. A total of 200 eligible scans were submitted for further analysis.
The scans were analyzed by consensus by two musculoskeletal radiologists of 8 (RM) and 2 (PY) years of experience, respectively. Scans were performed on either a 1.5-Tesla (Signa HDxt 1.5 T, GE Healthcare) or 3-Tesla (Discovery MR750w 3.0 T, GE Healthcare) whole-body scanner with dedicated circumferential knee coils. Our departmental knee MRI protocol consists of coronal, sagittal, and axial FSPD sequences, with a T2* sagittal sequence in patients under 35 years of age, and a T1 sagittal sequence in patients over 35 years of age.
In each scan, the ITB was scored as normal (grade 0; Fig. 3a), minor sprain (grade 1), severe sprain (grade 2) and torn (grade 3). Table 1 and Figs. 2 and 3 describe and illustrate the definitions for each grade in more detail. Following this assessment of the ITB, a systematic review of the medial (medial collateral ligament, posteromedial corner) and lateral soft tissue structures (lateral collateral ligament, biceps femoris tendon, popliteus tendon, popliteofibular ligament), anterior cruciate ligament, posterior cruciate ligament, medial and lateral meniscus was performed, with each structure graded as 0 (intact) or 1 (torn). No distinction was made between partial/low-grade and complete/high-grade injury. In addition, other notable findings such as bone bruising, fracture, and extensor mechanism abnormalities were specified.
Fisher’s exact tests were performed to establish if there was a significant association between ITB injury and ACL injury (p < 0.05). The posterolateral corner was considered significantly injured if two or more of the following structures were torn: popliteus tendon, popliteofibular ligament, LCL, and biceps femoris tendon [13].
Results
A total of 200 knees fulfilled the inclusion criteria of acute knee trauma less than 4 weeks prior to the scan and were analyzed in this study. The mean age was 27.4 years (range, 9–69 years) and 143 patients were male and 57 were female.
The proportions of internal knee injuries are now described and summarized in Table 2. The most common single pathological finding in our traumatic knee injury series was bone edema, seen in 154 of our 200 patients (77 %), and this was the solitary finding in seven cases (3.5 %). Excluding the ITB, the most frequent soft tissue injuries were ACL rupture (107), MCL rupture (95), and meniscal tears (50 involving the medial meniscus and 37 the lateral meniscus). The combination of ACL and MCL tear was seen in 66 cases: in 35 of these cases there was also a tear of one or both of the menisci. Transient lateral patellar dislocation was the primary mechanism of injury in 31 cases (15.5 %). The PCL was torn in 16 cases (8 %) and there was a significant posterolateral corner injury in ten cases (5 %). In 13 cases (6.5 %), no traumatic injury was identified.
The ITB was injured in 115 cases (57.5 %) and normal in 85 cases (42.5 %). ITB injury was defined as either a sprained (grades 1 and 2) or torn ITB (grade 3). Grade 1 injury was seen in 90 cases (45 %), grade 2 injury in 20 (10 %), and grade 3 injury in only 5 (2.5 %).
The findings in the 115 cases of ITB injury were as follows. In 65 %, there was an ACL tear (75/115) and in 20 % transient patellar dislocation (23/115). There was one case of combined ACL tear and patellar dislocation, so 84 % of cases with ITB sprain showed either ACL tear or transient patellar dislocation. Conversely, where there was an ACL tear, the ITB was injured in 75/107 (70 %) and where there was patellar dislocation the ITB was injured in 23/31 (74 %). All of the ten cases with significant posterolateral corner injury had coexistent cruciate ligament injury (both ligaments torn in five cases, the ACL in four, and the PCL in one) and all were associated with ITB injury including four cases of complete ITB rupture.
The LCL was torn in ten cases. In nine of these cases, there was also significant posterolateral corner injury. In all of these cases, one or both cruciate ligaments were torn and ITB injury consistently demonstrated (grade 1/2 in six cases and grade 3 in four cases). The biceps femoris was torn in only four cases, all of which were in the context of significant posterolateral corner injury. Again, ITB injury was seen in all four cases (grade 1/2 in two cases and grade 3 in two cases).
There were only 14 (12 %) cases where there was ITB sprain without cruciate ligament tear, patellar dislocation, or posterolateral corner injury, and in only two (2 %) cases was ITB sprain an isolated finding. In only three of 17 cases where the MCL was the only ligamentous structure injured was an ITB injury apparent (17 %).
An ITB tear (grade 3 injury) was seen in only 2.5 % of cases in our series of 200 knee trauma MRI scans. Of these five cases of ITB tear, in four there were injuries to both cruciate and collateral ligaments as well as significant PLC injuries. In the other case, the only other finding was a complete ACL tear.
A Fisher’s exact test was performed (Tables 3 and 4) and there was a significant relationship between ITB injury and ACL rupture (p = 0.0002). There was also a significant relationship between ITB injury and patellar dislocation (p = 0.0485).
Discussion
The ITB is a large, flat, fibrous band that runs over the lateral aspect of the hip, thigh, and knee, connecting the ilium with the proximal tibia (Fig. 1). Its attachment to the Gerdy tubercle [14] on the anterolateral tibia is well recognized, although the anatomy is more complex than is often appreciated, with multiple attachments to the linea aspera, lateral epicondyle, patellar retinaculum, and joint capsule [15]. The ITB stabilizes the anterolateral knee, resisting varus stress and rotation [14]. Compared to the menisci, cruciate, and collateral ligaments, it is infrequently mentioned in the context of acute knee trauma. Nevertheless, an ITB avulsion fracture from its attachment to the Gerdy tubercle is occasionally seen in conjunction with lateral ligamentous injuries [16]. The ITB is now believed to play a role in the pathophysiology of the Segond fracture of the lateral tibial condyle together with the lateral capsule (meniscotibial ligament) [17]. Some clinical studies have indicated a synergistic interaction between ITB disruption and ACL tears in anterolateral rotational instability [18].
However, the concept of discrete ITB injury on MRI, in particular a “sprain”, defined by adjacent edema with structural integrity on MRI, has not been widely addressed, nor the possible associations with other knee injuries. With its lack of ionizing radiation and excellent multiplanar soft tissue resolution, MRI is well established as the first-line technique for evaluating traumatic internal derangement of the knee [19]. We therefore analyzed high-quality MR studies from a database of acute knee trauma cases, with particular reference to the status of the ITB. We demonstrated that ITB injury is relatively common in knee trauma. A significant association between ITB injury and ACL tears on MRI, as well as ITB injury and transient lateral patellar dislocation, was found (Fig. 4), with 84 % of patients with an ITB injury showing either of these two acute injuries. There would also appear to be an association with significant posterolateral corner injury, with ITB injury a consistent finding in all ten cases in our study. Isolated ITB injury and ITB tears were extremely uncommon. Tears were usually seen in the context of multi-ligament, high-energy trauma, involving all the cruciate and collateral ligaments in four out of five cases (Fig. 5). It is therefore reasonable to conclude that ITB injury predicts significant internal derangement after trauma. The epidemiology of our knee trauma cases is similar to other published studies, reflecting the prevalence of common injury mechanisms and resultant patterns of internal derangement [5].
Our study has a number of limitations. The diagnosis of ITB injury is presumptive and purely based upon radiological findings, without clinicopathological correlation. In particular, the peritendinous edema seen in grade 1 injuries may or may not reflect ITB injury and could reflect injury to adjacent structures. The first structure analyzed in our systematic review of each scan was the ITB, which does not reflect the typical approach to analysis of a knee MRI study, where the menisci and cruciates are often initially scrutinized [20]. Both this and the retrospective nature of the study introduce observer bias. We have limited information regarding the mechanism of injury in each patient and there is variability of the duration of time of between the injury and scan, although to minimize this confounding variable, only scans where the injury occurred less than 4 weeks before were included. It is possible that athletic patients who sustain knee injuries are at increased risk of ITB friction syndrome and that some cases of apparent ITB sprain actually represent ITB friction syndrome, although our criteria for sprain was signal abnormalities both superficial and deep to the ITB, whereas edema is usually seen only deep to the ITB in friction syndrome.
To summarize, ITB injuries in acute knee trauma are common but rare in isolation. This correlates with the paucity of descriptions of acute ITB injury in the literature. Pure varus stress is required for an isolated ITB disruption and this is a rare mechanism of injury, as varus stress usually combines with flexion and internal rotation at the knee joint [5]. The clinical significance of ITB injury is unclear, especially in the presence of more established stabilizing and supportive structures such as cruciate ligaments, menisci, and posterolateral corner. The underlying mechanisms of injury are also unclear. In patellar dislocation, direct impact and contusion from abnormal lateral motion of patella would seem a reasonable explanation. Nevertheless, our study demonstrates that in acute knee trauma imaging, injury to the ITB is usually an indicator of significant internal derangement, with a strong association with ACL rupture, significant posterolateral corner injury, and acute patellar dislocation. It would seem reasonable to conclude that the ITB acts synergistically with the ACL and lateral/posterolateral ligamentous structures in knee stability. A routine review of the ITB as a discrete entity may be a useful approach in acute knee imaging.
References
Bollen S. Epidemiology of knee injuries: diagnosis and triage. Br J Sports Med. 2000;34(3):227–8.
McNally EG. Magnetic resonance imaging of the knee. BMJ. 2002;325(7356):115–6.
Gage BE, McIlvain NM, Collins CL, Fields SK, Comstock RD. Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad Emerg Med Off J Soc Acad Emerg Med. 2012;19(4):378–85.
Flandry F, Hommel G. Normal anatomy and biomechanics of the knee. Sports Med Arthrosc Rev. 2011;19(2):82–92.
Hayes CW, Brigido MK, Jamadar DA, Propeck T. Mechanism-based pattern approach to classification of complex injuries of the knee depicted at MR imaging. Radiograph Rev Publ Radiol Soc N Am, Inc. 2000;20 Spec No: S121–34.
Haims AH, Medvecky MJ, Pavlovich Jr R, Katz LD. MR imaging of the anatomy of and injuries to the lateral and posterolateral aspects of the knee. AJR Am J Roentgenol. 2003;180(3):647–53.
Pacholke DA, Helms CA. MRI of the posterolateral corner injury: a concise review. J Magn Reson Imaging: JMRI. 2007;26(2):250–5.
Seebacher JR, Inglis AE, Marshall JL, Warren RF. The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am Vol. 1982;64(4):536–41.
Beals TC. So who was Gerdy… and how did he get his own tubercle? Am J Orthop (Belle Mead NJ). 1996;25(11):750–2.
Kaplan EB. The iliotibial tract; clinical and morphological significance. J Bone Joint Surg Am Vol. 1958;40–A(4):817–32.
Muhle C, Ahn JM, Yeh L, Bergman GA, Boutin RD, Schweitzer M, et al. Iliotibial band friction syndrome: MR imaging findings in 16 patients and MR arthrographic study of six cadaveric knees. Radiology. 1999;212(1):103–10.
Pelsser V, Cardinal E, Hobden R, Aubin B, Lafortune M. Extraarticular snapping hip: sonographic findings. AJR Am J Roentgenol. 2001;176(1):67–73.
Vinson EN, Major NM, Helms CA. The posterolateral corner of the knee. AJR Am J Roentgenol. 2008;190(2):449–58.
Fairclough J, Hayashi K, Toumi H, Lyons K, Bydder G, Phillips N, et al. The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. J Anat. 2006;208(3):309–16.
Vieira EL, Vieira EA, da Silva RT, Berlfein PA, Abdalla RJ, Cohen M. An anatomic study of the iliotibial tract. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2007;23(3):269–74.
Recondo JA, Salvador E, Villanua JA, Barrera MC, Gervas C, Alustiza JM. Lateral stabilizing structures of the knee: functional anatomy and injuries assessed with MR imaging. Radiograph Rev Publ Radiol Soc N Am, Inc. 2000;20 Spec No: S91–S102.
Davis DS, Post WR. Segond fracture: lateral capsular ligament avulsion. J Orthop Sports Phys Ther. 1997;25(2):103–6.
Terry GC, Norwood LA, Hughston JC, Caldwell KM. How iliotibial tract injuries of the knee combine with acute anterior cruciate ligament tears to influence abnormal anterior tibial displacement. Am J Sports Med. 1993;21(1):55–60.
Mackenzie R, Dixon AK, Keene GS, Hollingworth W, Lomas DJ, Villar RN. Magnetic resonance imaging of the knee: assessment of effectiveness. Clin Radiol. 1996;51(4):245–50.
Sanders TG, Miller MD. A systematic approach to magnetic resonance imaging interpretation of sports medicine injuries of the knee. Am J Sports Med. 2005;33(1):131–48.
Conflict of interest
The authors report no conflicts of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mansour, R., Yoong, P., McKean, D. et al. The iliotibial band in acute knee trauma: patterns of injury on MR imaging. Skeletal Radiol 43, 1369–1375 (2014). https://doi.org/10.1007/s00256-014-1918-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-014-1918-2