Abstract
Objective
Little is known about the natural course of pain from vertebral compression fractures (VCF). In this study we evaluated the pain course in conservatively treated patients with back pain and a VCF on the spine radiograph.
Materials and methods
Between May 2007 and November 2008, 169 patients with back pain referred by the general practitioner for spine radiographs and with a VCF were requested to participate in this follow-up study. Base line questionnaires about visual analogue scale (VAS) score, type of treatment and use of osteoporosis medication were filled in by 82 patients. Questionnaires were repeated at 6 weeks, and at 3, 6 and 12 months. Significant pain relief was defined as a decrease in VAS score of 50 % or more from baseline.
Results
At baseline, mean VAS score in 82 patients was 6.9 (SD 2.0). Significant pain relief at 12 months was reported by 44 patients (54 %) while in 38 patients (46 %) pain relief was insufficient. No predictors for pain relief could be identified. Patients with insufficient pain relief at 12 months used significantly more analgesics and in these patients physiotherapy did better than other types of therapy.
Conclusion
More than half of conservatively treated patients with back pain and VCF had sufficient pain relief at 12 months with most pain decrease in the first 3 months. However, a substantial proportion of patients still reported disabling pain. There were no predictors for the development of chronic pain. Patients with continuing pain ≥3 months after diagnosis of VCF may be candidates for vertebroplasty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vertebral compression fractures (VCFs) are an important health concern in the elderly population. VCFs are the most common fractures in patients with osteoporosis and these fractures are associated with an increased incidence of mortality, morbidity and reduced health status [1–5].
The vast majority of patients presenting with a VCF are treated by the general practitioner with conservative therapy. This may include a range of therapies, such as bed rest, analgesics, physiotherapy and sometimes bracing. However, little is known about the frequency of these therapies and its effect on pain [5].
Minimally invasive techniques, such as percutaneous vertebroplasty and kyphoplasty, may be performed in a selected group of patients [6–14]. Indications for these minimally invasive techniques partly depend on the knowledge about the natural course of a VCF. In some studies it is assumed that 10–20 % of patients with a symptomatic osteoporotic VCF will eventually develop chronic pain [15].
In patients with pain and the radiographic diagnosis of VCF, little is known about the frequency and type of conservative therapies that are instigated in general practice and its effect on pain. In this study, we followed patients with back pain referred by the general practitioner for spine radiographs and with a VCF identified on the X-ray. The primary aim of this prospective follow-up study was to determine the natural course of pain in a large cohort of symptomatic patients with a VCF. The secondary aim was to assess the type of conservative therapy prescribed by the general practitioner and its effect on the pain.
Materials and methods
This study was approved by the Institutional Review Board and written patient informed consent was obtained.
Patients
Between May 2007 and November 2008, enrolment of patients took place in three large teaching hospitals in the Netherlands. Patients referred by their general practitioner for a spine radiograph and with the diagnosis of VCF on these X-rays were asked to fill in a short questionnaire regarding the presence, severity and duration of pain. Inclusion criteria for this study were:
-
1.
VCF on spine radiograph
-
2.
Age ≥50 years
-
3.
Back pain for 6 weeks or more
-
4.
Visual analogue scale (VAS) score ≥5
-
5.
Conservative therapy
Dementia was an exclusion criterion. Eligible patients received a more comprehensive baseline questionnaire within 1 week of the spine radiograph regarding VAS score and type of conservative treatment. Patients who did not return these questionnaires were contacted by telephone to reconsider participation. If necessary, a medical student helped with filling in the forms.
Follow-up
The patients included received additional questionnaires at 6 weeks, and at 3, 6 and 12 months. These questionnaires contained a VAS score, questions on the type of treatment during the previous period and use of osteoporosis medication. The VAS score ranged from 0 (no pain) to 10 (worst pain ever). Use of pain medication was classified into an ordinal variable: (0) no pain medication, (1) paracetamol, (2) non-steroidal anti-inflammatory agents (NSAID), and (3) opiate derivatives.
Statistical analysis
Significant pain relief was defined as a decrease in VAS score of 50 % or more. Univariate logistic regression analysis was used to assess a possible relation between pain relief and the following factors: age, gender, duration of back pain at baseline and baseline VAS score. Potential predictors of the VAS score and significant pain relief were examined using a (stepwise) multiple linear regression model. Chi-squared test was used to correlate significant pain relief at 12 months with the use of pain medication. Statistics were calculated using MedCalc (Mariakerke, Belgium).
Results
One hundred sixty-nine patients filled in the short primary questionnaire. There were 34 non-responders, 32 declined participation, 17 had a VAS score <5, 3 had dementia, 1 was planned for percutaneous vertebroplasty and 1 died. Ultimately, 82 patients were included at baseline and form the basis of this study. Figure 1 shows the patient flow chart. Baseline characteristics of the patients enrolled are summarised in Table 1.
Changes in VAS scores
At baseline the mean VAS score was 6.9 (SD 2.0). Figure 2 shows the mean VAS score over time. A significant decrease in pain scores occurred, particularly in the first 3 months (p < 0.05), while thereafter the decrease in pain scores was minimal. None of the baseline factors predicted the VAS score at 12 months.
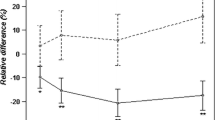
Significant pain relief
Forty-four patients (54 %) had significant pain relief at 12 months, while 38 patients (46 %) did not. Figures 3, 4, 5 show the mean VAS score over time for the two groups.
Type of treatment
Table 2 shows the type of treatment patients received from the general practitioner at baseline. Analgesics were the most frequent treatment for subacute VCFs. After 12 months, 41 % of patients still used analgesics. Of patients with insufficient pain relief at 12 months, 83 % still used pain medication. In patients with significant pain relief this was 17 %. This difference in use of pain medication between the two groups at 12 months was statistically significant (P = 0.012). At baseline 44 out of 82 (54 %) patients had osteoporosis medication. This percentage gradually increased to 38 out of 58 patients (66 %) at 12 months.
Discussion
In this study we found that the natural course of pain in conservatively treated patients with back pain and a VCF on the spine radiograph is basically bidirectional: about half of patients had insufficient pain relief at 12 months while in the other half pain decreased progressively, particularly during the first 3 months and this trend was sustained during the first year of follow-up. Analgesics medication was the most frequent treatment. Patients with insufficient pain relief used significantly more analgesics after 12 months. In patients with insufficient pain relief during follow-up, physiotherapy as the only therapy did better than other types of conservative therapy. In patients with pain relief, this was independent of the type of therapy (physiotherapy, medication or both). We were unable to detect predictors for both significant and insufficient pain relief at follow-up. Factors like age, baseline VAS score, fracture location, type and number of fractures, duration of pain at baseline and others failed to predict pain relief in stepwise logistic regression models. At baseline about half of the patients used osteoporosis medication and this increased to about two thirds of patients at 12 months. Our study has several limitations. VCF was diagnosed on a spine radiograph, but it was uncertain whether this VCF was the cause of pain and also the age of the VCF was not known. No physical examination, magnetic resonance imaging (MRI), or bone densitometry was performed. Sometimes, and especially in non-acute VCFs, it is difficult to distinguish between other causes of back pain, such as degenerative disease, spinal stenosis, facet arthropathy, sacroiliac joint dysfunction, and muscular pain. However, we primarily aimed to study the course of pain in this particular patient population in general practice. Another limitation is the lack of follow-up imaging to detect possible new VCFs.
In a previous study [15], we also found that a substantial proportion (40 %) of conservatively treated patients with acute VCFs still had disabling pain after 1 year, despite the higher class of pain medication used at various intervals. Optimal pain medication and supportive therapy were apparently not sufficient for pain relief in a large proportion of these conservatively treated patients. On the other hand, 60 % of patients had sufficient pain relief with conservative therapy, almost all within 3 months of the acute fracture. Also in this study we could not find any predictors for the development of chronic pain. In particular, baseline pain scores, number of fractures, and the degree or shape of vertebral compression had no influence on the development of chronic pain.
In the natural history of pain after an acute vertebral compression fracture, the time point of 3 months may be of clinical significance. There is no consensus in the literature about the best timing for minimally invasive techniques. According to this study combined with the results of the VERTOS II trial [15], patients with continuing pain at 3 months may be candidates for vertebroplasty.
The effectiveness of vertebroplasty is currently under debate. Most results are based on retrospective studies. Recently, 3 randomized controlled trials concerning vertebroplasty have been published with conflicting results [12–14]. Investigators in 2 trials [13, 14] concluded that there is no benefit to vertebroplasty over a sham placebo procedure involving the injection of local anaesthetic into the area adjacent to the fracture. In the study by Buchbinder et al. [14] 78 patients with 1 or 2 painful osteoporotic VCFs were randomized to receive either vertebroplasty or a sham procedure, which included infiltration of anaesthetic into the pedicular periosteum. The primary measured outcome was overall pain at 3 months. Despite significant reductions in overall pain in both groups, there was no significant advantage of vertebroplasty over the sham procedure.
In the study by Kallmes et al. [13] 131 patients with one to three painful osteoporotic VCFs were randomized to undergo either vertebroplasty or a simulated sham procedure, which included infiltration of anaesthetic into the periosteum of the posterior lamina. The primary outcomes were RMD scores and average pain intensity during the preceding 24 h at 1 month. Treatment-group crossover was permitted at 1 month. At this time, there was no significant difference between the two groups in either the RMD score or the pain rating. In the third trial, VERTOS II [12] vertebroplasty was compared with optimal conservative treatment in 202 patients with VCFs and bone oedema on MR imaging, back pain for ≤6 weeks, and a VAS score for pain of ≥5. The primary outcome was pain relief at 1 month and 1 year. The authors concluded that in a subgroup of patients with acute osteoporotic vertebral compression fractures and persistent pain, vertebroplasty is effective and safe. Pain relief after vertebroplasty is immediate, is sustained for at least a year, and is significantly greater than that achieved with conservative treatment, and at an acceptable cost.
Other than the lack of blinding in VERTOS II, the most important difference between the two sham studies and VERTOS II is patient selection. In the sham studies, both acute and chronic fractures were included, while in VERTOS II, only acute fractures were eligible. In addition, bone oedema in the affected vertebra was not a consistent inclusion criterion in the sham studies. The sham studies lacked a control group without intervention. The discordant results from the sham studies, on the one hand, and VERTOS II, on the other hand, have incited much debate. Apparently, clinicians still do not know how to best treat their patients. Medical societies understand the need for further randomised trials to support treatment decisions. Until then, on the basis of our findings, we believe it is justified to offer vertebroplasty to patients with compression fractures with insufficient pain relief after 3 months of conservative treatment.
Conclusion
More than half of conservatively treated patients with back pain and a VCF had sufficient pain relief at 12 months, particularly during the first 3 months. However, after 1 year, a substantial proportion of patients still reported disabling pain. There were no predictors for the development of chronic pain. Patients with continuing pain ≥3 months after diagnosis of the fracture may be candidates for invasive therapy such as vertebroplasty.
References
Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–7.
Black DM, Cummings SR, Karpf DB, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–41.
Nevitt MC, Ettinger B, Black DM, et al. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med. 1998;128:793–800.
Hasserius R, Karlsson MK, Jonsson B, Redlund-Johnell I, Johnell O. Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly-a 12- and 22-year follow-up of 257 patients. Calcif Tissue Int. 2005;76:235–42.
Klazen CA, Verhaar HJ, Lohle PN, et al. Clinical course of pain in acute osteoporotic vertebral compression fractures. J Vasc Interv Radiol.. 2010;21:1405–9.
Voormolen MH, Lohle PN, Lampmann LE, van den Wildenberg W, Juttmann JR, Diekerhof CH, et al. Prospective clinical follow-up after percutaneous vertebroplasty in patients with painful osteoporotic vertebral compression fractures. J Vasc Interv Radiol. 2006;17:1313–20.
Ploeg WT, Veldhuizen AG, The B, Sietsma MS. Percutaneous vertebroplasty as a treatment for osteoporotic vertebral compression fractures: a systematic review. Eur Spine J. 2006;15(12):1749–58.
Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8(9):1137–48.
Zoarski GH, Snow P, Olan WJ, Stallmeyer MJ, Dick BW, Hebel JR, et al. Percutaneous vertebroplasty for osteoporotic compression fractures: quantitative prospective evaluation of long-term outcomes. J Vasc Interv Radiol. 2002;13:139–48.
McGraw JK, Lippert JA, Minkus KD, Rami PM, Davis TM, Budzik RF. Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty: results and follow-up. J Vasc Interv Radiol. 2002;13:883–6.
Legroux-Gerot I, Lormeau C, Boutry N, Cotten A, Duquesnoy B, Cortet B. Long-term follow-up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol. 2004;23:310–7.
Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (VERTOS II): an open-label randomised trial. Lancet. 2010;376:1085–92.
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569–79.
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557–68.
Venmans A, Klazen CA, Lohle PN, et al. Natural history of pain in patients with conservatively treated osteoporotic vertebral compression fractures: results from VERTOS II. AJNR Am J Neuroradiol. 2012;33:519–22.
Acknowledgement
Conflict of interest
No conflict of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Venmans, A., Lohle, P.N.M. & van Rooij, W.J. Pain course in conservatively treated patients with back pain and a VCF on the spine radiograph (VERTOS III). Skeletal Radiol 43, 13–18 (2014). https://doi.org/10.1007/s00256-013-1729-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-013-1729-x