Abstract
Objective
Morphological correlation between the acetabulum and femur at the hip joint is still controversial. We tested the hypothesis that femoral anteversion correlates with acetabular version and coverage in patients with developmental dysplasia of the hip (DDH).
Materials and methods
Using pelvic computed tomography (CT) images of 79 hips in 49 Asian women with DDH and 49 normal hips, we measured femoral anteversion, the axial and vertical acetabular version and the acetabular sector angle (ASA) to demarcate femoral head coverage. Depending on the location of the acetabular bone defect, dysplastic hips were divided into three subgroups: the anterior, global and posterior deficiency groups. We performed a comparative analysis between dysplastic and normal hips using the Wilcoxon rank sum test, and a relative analysis between femoral anteversion and acetabular measurements in dysplastic hips using Pearson’s correlation coefficient.
Results
The amount of femoral anteversion in dysplastic hips was greater and more variable than in normal hips (p < 0.0001, p = 0.0277 respectively). Femoral anteversion in dysplastic hips correlated significantly with acetabular anteversion in the groups with anterior and global deficiency subgroups (p < 0.05, r = 0.2990, p < 0.05, r = 0.451 respectively), but not with the posterior deficiency subgroup. Femoral anteversion also correlated with vertical acetabular version. When acetabular coverage was examined, significant correlations were noted between femoral anteversion and anterior and superior coverage, but not with posterior coverage. These correlations were not observed in normal hips.
Conclusions
Our results showed significantly greater and more variable femoral anteversion in DDH, and a significant correlation between femoral anteversion and acetabular version and coverage in DDH with anterior and global acetabular bone deficiency.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH) has various morphological abnormalities. The acetabulum in the dysplastic hip has been reported to show a shallow articulating cavity, an excessively oblique acetabular roof, and decreased acetabular coverage of the femoral head [1]. The femur also shows increased femoral anteversion and neck-shaft angle along with a shortened femoral neck [2]. These abnormalities may cause abnormal joint stresses, leading to subsequent degeneration of the labrum and articular cartilage, and thus secondary osteoarthritis develops at an early age [3–6].
When planning periacetabular osteotomies [7, 8] for patients with dysplastic hips, it is important to assess the morphology of hip joint three-dimensionally and to customize the correction in accordance with this individual variation in acetabular and femoral morphologies [9–12]. Previous studies suggested that suboptimal correction of abnormal acetabular version and coverage can result in an inferior clinical result from the osteotomy [13–15].
Morphological features in dysplastic hips have been reported in detail, with acetabular and femoral findings having also been separately described. Only a few reports have evaluated the relationship between the femur and acetabulum [1, 16–18]. Anda et al. reported that femoral morphology was not found to correlate with acetabular morphology in both normal and dysplastic hips [16, 18]. In contrast, Jacobsen et al showed in their three dimensional CT study a significant correlation between femoral anteversion and anterior acetabular coverage in the dysplastic hip [1]. Therefore, the true relationship remains controversial.
The recent development and prevalence of computer imaging software has enhanced the description of three-dimensional (3D) morphology of the hip. Studies using CT data revealed a substantial amount of individual variation in acetabular version, the location of the bone defect, and degree of acetabular dysplasia [19, 20]. A review of the literature revealed that acetabular dysplasia could be classified as anterior, posterior, and global deficiency groups based on the location of the acetabular bone defect [16, 19–22]. We previously reported that these subgroups of acetabular dysplasia were significantly associated with acetabular version as well as rotational alignment of the entire pelvis [23]. These findings led us to examine the correlation between femoral and acetabular version in each subgroup of dysplastic hips.
We hypothesized that the femoral and the acetabular abnormalities may have the wide distribution in dysplastic hips and that the femoral anteversion may have different correlations with the acetabular morphology among the subgroups of dysplastic hips. In this study, we examined the distribution of hip deformities in dysplastic hips compared with normal hips, and the correlation of femoral anteversion with acetabular version and coverage in subgroups of dysplastic hips.
Materials and methods
Patients
This retrospective study was approved by our institutional review board. We reviewed standard anteroposterior (AP) radiographs of the pelvis [24, 25] and pelvic CT scans of 143 hips in 84 patients with DDH, obtained during preoperative examinations for corrective osteotomies between July 2004 and June 2010. DDH was defined as a lateral center-edge angle of Wiberg [26] that was less than 20°, based on measurements using AP radiographs of the pelvis. Thirty hips with Tönnis grade 2 or advanced [27] and visible osteophyte formation on radiographic examination were excluded from the study because their measurements could not be verified as accurate. We also excluded 6 patients (12 hips) with prior surgery and 7 (12 hips) with severe deformities of the femoral head. To eliminate the effect of morphological differences between gender [28], we included only female subjects in this study (10 hips in 7 male patients were excluded). On the basis of these criteria, 79 hips in 49 female patients were included in this study. Thirty patients had bilateral involvement, and 19 patients had unilateral involvement. The average age upon initial examination was 39.6 years (range, 17−60 years). All hips were classified as type 1 according to the classification system of Crowe et al. based on the migration magnitude of the femoral head relative to the interteardrop line [29]. This classification of the degree of vertical subluxation of the hip is a measure of severity of disease: Type I—vertical subluxation measured from the inferior margin of the tear to the head–neck junction is <50% of the diameter of the femoral head or <10% of the height of the pelvis; Type II—50 to 75% subluxation; Type III—75 to 100% subluxation; and Type IV—more than 100% subluxation. Regarding the past treatment of the hip, 5 patients (5 hips) had a history of non-operative treatment for DDH.
The control group included 49 normal hips in 44 patients with osteoarthritis of the knee. These patients had no history of disease or articular symptoms in the hip joints as indicated by a medical records search and radiographic examination. All subjects were women with an average age of 75.1 years (range, 52−83 years). Although these two groups were similar in terms of body mass index and laterality of the hips evaluated, the average age of the control group was older than that of the DDH group. We confirmed that control subjects had no degenerative changes in hip joints or other hip abnormalities [30, 31]. We examined all AP pelvic radiographs and pelvic CT images obtained during planning for total knee arthroplasty using a CT-based navigation system [32].
Computed tomography evaluations
Pelvic computed tomography (CT) was performed following methods previously described [23, 33]. Briefly, images were obtained at 2-mm intervals from the anterior superior iliac spines to the inferior rim of the pelvis in combination with a 200-mm section of the midpoint of the knee joint with a slice thickness of 2 mm. Control group CTs were obtained with the patients in a supine position. Data were obtained from a 100-mm section of the femoral head, a 200-mm section of the midpoint of the knee joint, and a 100-mm section of the distal part of tibia, with a slice thickness of 2 mm, in preparation for a CT-based navigation system of the total knee arthroplasty. Multiplanar reconstruction processing was performed on these resulting images using analysis software (3D template; Japan Medical Materials, Osaka, Japan). As standardizing the position of the pelvis at the time of imaging is important, we defined an anterior pelvic plane [30, 34] involving the anterior superior iliac spines and the public tubercles, as a reference plane (coronal section). After correcting according to this reference, we then performed the following measurements.
Measurements
All measurements using CT images were performed by one observer (M.A.) and were repeated in a blinded manner during the course of two sessions at least one month apart. Two observers (M.A. and T.S.) independently made CT measurements on the scans of 30 randomly selected hips. The intraobserver and interobserver reliabilities were evaluated with the use of the intraclass correlation coefficient.
Femoral anteversion
Anteversion of the femoral neck was assessed three-dimensionally using techniques described by Sugano et al. [35]. Briefly, the femoral neck axis is measured from a best-fit line on a single cut high in the femoral neck just distal to the head. The distal femoral condylar axis is measured from a transepicondylar axis, which can also be discernible in damaged knees like control subjects in this study [36]. The relative alignment of these two axes describes femoral anteversion (Fig. 1a).
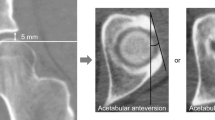
a The femoral anteversion angle was defined as the angle between the femoral neck axis and the transepicondylar axis. b The acetabular anteversion angle was determined in the axial plane passing through the femoral head center as the angle formed by the intersection of a line connecting the anterior and posterior edges of the acetabulum and a sagittal line. c The Sharp angle was determined in the coronal plane passing through the femoral head center as the angle formed by a line connecting the superior and inferior edges of the acetabulum and a horizontal line
Acetabular version
We defined the acetabular opening direction as the acetabular anteversion angle in the axial plane. The acetabular lateral opening direction was defined as the vertical acetabular version (Sharp angle) in the coronal plane. Both versions were measured at the level of center of the femoral head (Fig. 1b, c).
Acetabular coverage
To determine acetabular coverage of the femoral head (Fig. 2), we measured the acetabular sector angle (ASA) based on a modified version of the method described by Anda et al. [16]. We determined the anterior and posterior ASAs in the axial plane passing through the center of the femoral head, as well as the superior ASA in the coronal plane. The values of the anterior and posterior ASA were used to classify the dysplastic hips into three groups depending on the location of the acetabular bone defect according to the method of Ito et al. [19] with modification: the anterior deficiency group (anterior ASA < 50° and posterior ASA > 90°), the global deficiency group (anterior ASA < 50° and posterior ASA < 90°) and, the posterior deficiency group (anterior ASA > 50° and posterior ASA < 90°). Using these criteria, 44 hips (55.7%) were diagnosed as having an anterior deficiency, 26 hips (32.6%) as having a global deficiency, and 9 hips (11.4%) as having a posterior deficiency.
Statistical analysis
A statistical analysis was performed using JMP 6.0.3 (SAS Institute, Tokyo, Japan). Wilcoxon rank sum tests were used to compare the radiographic parameters between dysplastic and normal hips in each subgroup. The Levene test was used to assess the equality of variances in dysplastic and normal hips. The F-value signifies the deviation ratio between dysplastic and normal hips. The Dunnett tests were used to compare the radiographic parameters between the control group and all subgroups. Pearson’s correlation coefficient was used to evaluate the relationships between the parameters of the femur and the acetabulum. For all statistical analyses, p values less than 0.05 were considered significant.
Results
Comparison of the parameters between dysplastic and normal hips is shown in Table 1.
The average femoral anteversion was 22.2 ± 10.8° in dysplastic hips and 14.3 ± 6.8° in normal hips, indicating a significantly larger degree of femoral anteversion in dysplastic hips (p < 0.0001). Femoral anteversion in dysplastic hips varied widely from −13.2 to 58.2° with significantly wider distribution of values than in normal hips (p = 0.0024) (Fig. 3a). When the dysplastic hips were divided into subgroups, the degree of femoral anteversion in the anterior and global deficiency subgroups was also significantly larger than in the control groups (p = 0.0040, p < 0.0001 respectively). However, we noted that the posterior deficiency subgroup was comparable to normal hips in the amount of femoral anteversion (Table 1, Fig. 4). Although the acetabular anteversion of dysplastic hips was significantly larger than that of normal hips (p = 0.0060), the difference was only 3° (Fig. 3b). In detail, acetabular anteversion in the anterior deficiency subgroup was significantly larger; however, acetabular anteversion in the posterior deficiency subgroup was significantly smaller compared with normal hips (p < 0.0001, p = 0.0005 respectively). The Sharp angles in dysplastic and normal hips were similarly distributed; however, significantly larger Sharp angles were noted in the dysplastic hips (Fig. 3c). Acetabular coverage was significantly smaller in dysplastic hips in all three portions (Fig. 3d–f).
Correlations between the femur and acetabulum in dysplastic hips with regard to various parameters are shown in Table 2.
There was no significant correlation between femoral anteversion and acetabular anteversion in dysplastic hips when they were lumped. However, when dysplastic hips were divided into subgroups, the anterior and global deficiency subgroups showed a significantly positive correlation between femoral anteversion and acetabular anteversion (p <0 .05, r = 0.2990, p < 0.05, r = 0.451 respectively; Fig. 5b, c). There was a significantly positive correlation between femoral anteversion and the Sharp angle (p = 0.0312, r = 0.25962) in dysplastic hips (Fig. 5d).
Correlation between the femoral anteversion and acetabular measurements. A scatter-plot chart showing the relationship between femoral anteversion (FeAv) and acetabular measurements and their linear regression. a–c) The relationship between FeAv and acetabular anteversion (AcAv) in a the control group, b the anterior deficiency subgroup, and c in the global deficiency subgroup. d The relationship between FeAv and Sharp Angle in DDH. e–g The relationships between FeAv and the ASA: e anterior, f superior and g posterior in DDH. *Statistical significance
Femoral anteversion correlated significantly with acetabular coverage of the femoral head in the anterior and superior portions (p = 0.0156, r = −0.29005, p = 0.0157, r = −029005 respectively; Fig. 5e–g). In normal hips, no significant correlations were observed between femoral anteversion and acetabular anteversion, Sharp angles, or acetabular coverage in any directions (Fig. 5a).
Intra-observer and inter-observer reliabilities, evaluated with the use of the intra-class correlation coefficient (ICC), were excellent, ranging from 0.98 to 0.99 and 0.88 to 0.96 respectively.
Discussion
In this study of 69 dysplastic hips and 49 normal hips, we confirmed morphological differences between dysplastic and normal hips and found significant correlations between femoral anteversion and acetabular version in the anterior and global deficiency subgroups. We also demonstrated a significant correlation of femoral anteversion to coverage in the anterior and superior portions.
As previously reported, the degree of femoral anteversion in dysplastic hips is significantly larger than in normal hips [18, 37–39]. Interestingly, when we compared the distribution of femoral anteversion between dysplastic and normal hips, dysplastic hips showed significantly wider distribution of femoral anteversion ranging from −13 to 58°. Sankar et al. [40] reported significant variability in femoral anteversion of the dysplastic hip in children. In their study on 37 consecutive hips, the mean femoral anteversion was 50.3° with a standard deviation of 17.9, varying from 0° to 95.7°. Therefore, this variability of femoral anteversion is thought to exist from the early stages of life. Additionally, femoral anteversion in the posterior deficiency subgroup was comparable to that of controls. This increased variability might lead to the controversy in relating femoral anteversion to other anatomical measurements.
In contrast to femoral anteversion, the distribution of acetabular anteversion in dysplastic hips was small and similarly distributed to that of normal hips. Although the degree of acetabular anteversion in DDH was significantly larger than that of normal hips, the difference was only 3° on average. The significance in the case of acetabular version might be “statistical significance” but not “clinical significance.” This finding was supported by other reports. Anda et al. [16] reported that acetabular anteversion was almost equal in dysplastic and normal hips, and that hip dysplasia is not associated with any consistent change in acetabular version. In their study including 21 adult patients, the mean acetabular anteversions were 22.1 ± 5.9° in dysplastic hips and 21.6 ± 5.1° in normal hips. However, when dysplastic hips were divided according to the location of the acetabular bone defect, significant differences in acetabular version were noted among the subgroups. Acetabular version in the anterior deficiency subgroup was significantly larger than in the other groups. Conversely, acetabular version in the posterior deficiency subgroup was significantly smaller than in the normal and global deficiency subgroups. Anda et al. [16] also suggested that there was a trend toward decreased acetabular anteversion in shallow hips with poor posterior support.
Normal hips did not show any correlation between femoral anteversion and acetabular version and coverage in this study and in the report by Anda et al. [16] in their 3D analysis. In pathological hips, Bargar et al. [18] also reported no correlation between femoral and acetabular anteversion in their cohort with 46 patients undergoing total hip arthroplasty without dysplastic hips in their 3D analysis. Our study also showed that femoral anteversion did not correlate significantly with acetabular anteversion in dysplastic hips when they were lumped. However, when they were divided, depending on the location of the acetabular bone defect in this study, femoral anteversion in the anterior and global deficiency subgroups correlated significantly with acetabular anteversion. Femoral anteversion also correlated significantly with acetabular coverage in the anterior and superior portions. These findings suggested a possible developmental interaction between the femur and acetabulum. Our results showed that the hip with larger degrees of femoral anteversion had increased acetabular version, suggesting a biomechanical vicious cycle resulting in the pathology of dysplastic hips with anterior and global acetabular deficiency.
In contrast, no correlation in either version or coverage was observed in hips with a posterior bone deficiency. We previously reported the earlier onset of pain in patients with posterior acetabular deficiency, suggesting the pathological significance of this group [33]. Our results and previous reports suggested the existence of several subtypes of dysplastic hips with different pathologies [23, 41]. Regarding the correlation with femoral anteversion in the posterior deficiency subgroup, relatively better anterior acetabular coverage in this subgroup compared with other subgroups may have fewer effects on the development of the femur. This requires further research and clarification.
It is important to customize correction of the acetabular fragment in accordance with individual variability of the hip when planning pelvic osteotomies for patients with DDH [12, 13, 15, 42]. Anterior rotation of the acetabular fragment is one of the conventional maneuvers performed during periacetabular osteotomies to correct anterior acetabular deficiency. In cases with excessive femoral anteversion, derotational femoral osteotomy is combined to improve the coverage and congruity of the hip joint [43]. In cases of posterior deficiency, anterior rotation of the acetabulum can aggravate posterior acetabular insufficiency in turn [13, 44]. Our observations confirmed that anterior rotation of the acetabular fragment is an anatomically reasonable maneuver for patients in anterior and global deficiency subgroups to cover the anteverted femoral head. However, the maneuver can be problematic in those with posterior acetbular deficiency and should therefore be avoided in this subgroup.
There were several limitations to this study. First, the normal subjects in this study were older than the DDH subjects; however, their hips were asymptomatic with no deformities. Their hips had no morphological abnormalities leading to osteoarthritis; therefore, investigating morphologies in this elderly population was valuable in understanding the normal hip joint in its true sense. We also corrected for pelvic tilt as the pelvis tends to tilt backward because of lumbar kyphosis in elderly patients. Second, because of the retrospective database and image review, correlation with clinical findings was limited. Nevertheless, it is important to understand 3D information and the relationship between femoral and acetabular morphologies for surgeons. Our stated purpose was to investigate the morphological correlation between femoral anteversion and acetabular morphologies as a first step in determining the potential need for augmentation procedures. Third, the study cohort was limited to Asian women with Crowe Type 1 hips, which may limit the generalizability of our findings to other populations. However, as DDH occurs frequently in Japan, we believe this does not change our overall findings of correlations between femoral and acetabular morphologies. Fourth, as the number of patients with DDH was limited, each subgroup had a relatively small number of hips. Although there were significant correlations between femoral anteversion and acetabular version in patients with anterior and global deficiency, analysis with a larger number of patients would increase the statistical power of the study.
In conclusion, our data reveal a significant correlation between femoral anteversion and acetabular version in Asian women with anterior and superior deficiency subgroups of DDH, but not in the posterior deficiency subgroup. We also found that femoral anteversion varied widely in dysplastic hips compared with normal hips.
References
Jacobsen S, Romer L, Soballe K. Degeneration in dysplastic hips. A computer tomography study. Skeletal Radiol 2005; 34:778–84.
Noble PC, Kamaric E, Sugano N, Matsubara M, Harada Y, Ohzono K, Paravic V. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res. 2003;417:27–40.
Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;7:985–9.
Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;3:423–9.
Nakamura S, Ninomiya S, Nakamura T. Primary osteoarthritis of the hip joint in Japan. Clin Orthop Relat Res. 1989;241:190–6.
Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58(2):176–83.
Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36.
Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984;66(3):430–6.
Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the "cross-over-sign". J Orthop Res. 2007;25:758–65.
Kiyama T, Naito M, Shiramizu K, Shinoda T. Postoperative acetabular retroversion causes posterior osteoarthritis of the hip. Int Orthop. 2009;33(3):625–31.
Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88(9):1920–6.
Peters CL, Erickson JA, Anderson L, Anderson AA, Weiss J. Hip-preserving surgery: understanding complex pathomorphology. J Bone Joint Surg Am. 2009;91 Suppl 6:42–58.
Johnston CE, Wenger DR, Roberts JM, Burke SW, Roach JW. Acetabular coverage: three-dimensional anatomy and radiographic evaluation. J Pediatr Orthop. 1986;6(5):548–58.
Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–9.
Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466(7):1633–44.
Anda S, Terjesen T, Kvistad KA, Svenningsen S. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr. 1991;1:115–20.
Reikeras O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta Orthop Scand. 1983;54(1):18–23.
Bargar WL, Jamali AA, Nejad AH. Femoral anteversion in THA and its lack of correlation with native acetabular anteversion. Clin Orthop Relat Res. 2010;468(2):527–32.
Ito H, Matsuno T, Hirayama T, Tanino H, Yamanaka Y, Minami A. Three-dimensional computed tomography analysis of non-osteoarthritic adult acetabular dysplasia. Skeletal Radiol. 2009;2:131–9.
Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;261:214–23.
Haddad FS, Garbuz DS, Duncan CP, Janzen DL, Munk PL. CT evaluation of periacetabular osteotomies. J Bone Joint Surg Br. 2000;82(4):526–31.
Nakamura S, Yorikawa J, Otsuka K, Takeshita K, Harasawa A, Matsushita T. Evaluation of acetabular dysplasia using a top view of the hip on three-dimensional CT. J Orthop Sci. 2000;5(6):533–9.
Fujii M, Nakashima Y, Sato T, Akiyama M, Iwamoto Y. Pelvic deformity influences acetabular version and coverage in hip dysplasia. Clin Orthop Relat Res. 2011;469(6):1735–42.
Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90 Suppl 4:47–66.
Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: A study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–8.
Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83 Suppl 58:1–135.
Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. Berlin: Springer; 1987. p. 165–71.
Traina F, De Clerico M, Biondi F, Pilla F, Tassinari E, Toni A. Sex differences in hip morphology: is stem modularity effective for total hip replacement? J Bone Joint Surg Am. 2009:121–8.
Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61(1):15–23.
McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52(1):148–59.
Hapa O, Yuksel HY, Muratli HH, Aksahin E, Gulcek S, Celebi L, et al. Axial plane coverage and torsion measurements in primary osteoarthritis of the hip with good frontal plane coverage and spherical femoral head. Arch Orthop Trauma Surg. 2010;10:1305–10.
Mizu-Uchi H, Matsuda S, Miura H, Higaki H, Okazaki K, Iwamoto Y. Three-dimensional analysis of computed tomography-based navigation system for total knee arthroplasty: The accuracy of computed tomography-based navigation system. J Arthroplasty. 2009;7:1103–10.
Fujii M, Nakashima Y, Yamamoto T, Mawatari T, Motomura G, Matsushita A, et al. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;4:895–903.
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;2:217–20.
Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr. 1998;22(4):610–4.
Yoshino N, Takai S, Watanabe Y, Fujiwara H, Ohshima Y, Hirasawa Y. Primary total knee arthroplasty for supracondylar/condylar femoral fracture in osteoarthritic knees. J Arthroplasty. 2001;4:471–5.
Shands AR Jr, Steele MK. Torsion of the femur; a follow-up report on the use of the dunlap method for its determination. J Bone Joint Surg Am. 1958;4:803–16.
Terjesen T, Benum P, Anda S, Svenningsen S. Increased femoral anteversion and osteoarthritis of the hip joint. Acta Orthop Scand. 1982;4:571–5.
Sankar WN, Neubuerge CO, Moseley CF. Femoral anteversion in developmental dysplasia of the hip. J Pediatr Orthop. 2009;29(8):885–8.
Visser JD, Jonkers A, Hillen B. Hip joint measurements with computerized tomography. J Pediatr Orthop. 1982;2(2):143–6.
Fujii M. Effect of intra-articular lesions on the outcome of periacetabular osteotomy in patients with symptomatic hip dysplasia. J Bone Joint Surg Br. 2011;93-B:1449–56.
Klaue K, Wallin A, Ganz R. CT evaluation of coverage and congruency of the hip prior to osteotomy. Clin Orthop Relat Res. 1988;232:15–25.
Azuma H, Taneda H, Igarashi H, Fukuoka M. Preoperative and postoperative assessment of rotational acetabular osteotomy for dysplastic hips in children by three-dimensional surface reconstruction computed tomography imaging. J Pediatr Orthop. 1990;10:33–8.
Jia J, Li L, Zhang L, Zhao Q, Liu X.. Three dimensional-CT evaluation of femoral neck anteversion, acetabular anteversion and combined anteversion in unilateral DDH in an early walking age group. Int Orthop. 2012;36:119–24.
Acknowledgement
None of the authors received financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was approved by the institutional review board. Investigation performed at Department of Orthopaedic Surgery, Kyushu University
Rights and permissions
About this article
Cite this article
Akiyama, M., Nakashima, Y., Fujii, M. et al. Femoral anteversion is correlated with acetabular version and coverage in Asian women with anterior and global deficient subgroups of hip dysplasia: a CT study. Skeletal Radiol 41, 1411–1418 (2012). https://doi.org/10.1007/s00256-012-1368-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-012-1368-7