Abstract
Posterior shoulder instability refers to the symptoms and signs resulting from excessive posterior translation of the humerus. Magnetic resonance (MR) imaging is the radiological modality of choice in the diagnostic assessment of posterior instability. Computed tomography (CT) is useful in the evaluation of osseous abnormalities associated with posterior instability. A detailed description of the posterior osseous and labroligamentous abnormalities has evolved recently, and many variant lesions of the posteroinferior labrum and/or capsular structures have been described. As the recommended surgical management of lesions associated with posterior instability is a lesion-specific approach, awareness of the specific lesions that have been described in association with posterior instability helps in pre-surgical planning. The purpose of this article is to review the classification of, and injury mechanisms leading to, posterior shoulder instability and to describe imaging findings associated with posterior instability, with emphasis on MR imaging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical findings
Posterior shoulder instability (PSI) constitutes approximately 5% of all cases of shoulder instability [1]. A higher proportion of approximately 10% can be seen in certain select groups with increased physical activity [2]. The common causes of PSI include traumatic posterior dislocations, a redundant posterior capsule, posterior labroligamentous tears and osteochondral lesions. Recurrent atraumatic posterior subluxation is the most common form of PSI and is being increasingly identified. PSI is usually associated with other directions of instability and is often triggered by minimal trauma [3]. Athletes with overhead arm activity, such as weightlifters, baseball pitchers, racket sport athletes, footballers, and swimmers, are at risk for developing posterior instability [4]. Subluxation is more common than dislocation with athletic injuries [5]. In this group of patients, there is chronic attenuation of the posterior capsule allowing repeated subluxations. Traumatic PSI is the result of a posteriorly directed blow to an adducted, internally rotated, and forward-flexed shoulder [4].
The patient with PSI complains of localized pain and/or clicking in the posterior aspect of the shoulder more often than actual instability symptoms [6–8]. The symptoms are usually brought on by repeated use. Shoulder fatigue with activity is a frequent symptom. Determining the exact activity that brings on the symptoms is important for correct clinical diagnosis. Often, a history of pain or a sense of instability is elicited when the arm is held in the position of forward flexion, adduction, and internal rotation. This can be confused with subacromial impingement. Clinical signs of PSI include the posterior apprehension sign, pain with posterior stress, and a characteristic “jerk” test with the arm at 90° of forward elevation and internal rotation.
Classification
Many systems exist for classifying PSI [7–9]. One system classifies it according to frequency, degree, direction, and cause [7, 8].
Frequency of posterior instability can be a single traumatic event or, more frequently, a recurrent symptom, as in the athletic population.
Degree of instability ranges from subluxation to dislocation. Athletes commonly present with recurrent posterior subluxation.
Direction is unidirectional (pure posterior), bidirectional (posteroinferior), or multidirectional (posterior, inferior, and anterior).
Cause is divided into two types, either traumatic or atraumatic. The traumatic type is subdivided into macrotrauma (a single traumatic event) or microtrauma (recurrent minor trauma). Both subdivisions may have either voluntary or involuntary subluxations.
Stabilizers of the posterior aspect of the glenohumeral joint
Excessive posterior humeral translation is limited by the bony posterior glenoid rim and the posterior soft tissue structures, including the posterior labrum, posterior capsular structures, including the posterior axillary pouch and posterior band of inferior glenohumeral ligament (PIGHL), periosteum, and the rotator cuff muscles. The capsule envelops the joint and changes in orientation and length during shoulder rotation. The posterior rotator cuff, particularly the teres minor muscle and tendon, reinforces the labrum and capsule and provides dynamic stabilization for the posterior joint. The subscapularis is the most important resistor of posterior subluxation of the humerus [10]. The rotator interval capsule also helps resist posteroinferior humeral translation [11]. Instability of the joint posteroinferiorly has been demonstrated after experimental sectioning of the rotator interval capsule in cadavers [11].
Abnormalities to any of the above-mentioned structures are associated with PSI, and these abnormalities can be demonstrated on imaging. Magnetic resonance (MR) imaging may also be useful in identifying patients who might benefit from an open surgical procedure rather than an arthroscopic one. Because contemporary surgical techniques endeavor anatomical reconstruction, the significance of precisely defining the abnormal lesion preoperatively cannot be overemphasized [6, 12]. A detailed description of the posterior osseous and labroligamentous abnormalities has evolved, and variant lesions of the posteroinferior labrum and capsular structures have been described.
Glenoid side abnormalities
Labral and articular cartilage lesions
Reverse Bankart lesion
It is also called the posterior Bankart lesion. The reverse Bankart lesion and its variant labral detachments are usually seen in patients with PSI who have prior history of a significant traumatic episode causing posterior dislocation [13]. Similar to its anterior counterpart, the posteroinferior labrum is detached from the glenoid with a tear of the scapular periosteum (Fig. 1) [4, 14, 15]. There are no significant erosions of the adjacent glenoid articular cartilage [15]. MR arthrogram demonstrates detachment of the posteroinferior labrum form the glenoid, along with a tear of the scapular periosteum such that gadolinium sometimes outlines the medial aspect of the posterior glenoid neck (Fig. 2).
Reverse Bankart lesion in a 22-year-old man with PSI. Axial proton density (PD)-weighted (time to repeat/time to echo 3,000/30 ms) fat-saturated MR arthrographic image demonstrates the labral detachment (white arrow) and the detachment tear of the scapular periosteum (white arrowheads). Note the gadolinium outlining the posterior glenoid neck (black arrow) due to the periosteal breach
Posterior labrocapsular periosteal sleeve avulsion lesion
The crucial finding that defines the posterior labrocapsular periosteal sleeve avulsion (POLPSA) lesion is a periosteal sleeve created by the avulsion of the posterior scapular periosteum at its junction with the capsule and labrum (Fig. 3) [16, 17]. This is differentiated from a reverse Bankart lesion, in which there is disrupted posterior capsule and scapular periosteum in association with the labral detachment. The surgical technique differs, since the periosteal sleeve must be reduced in order to reattach the labrum. The presence of fibrous tissue in the periosteal sleeve precludes its communication with gadolinium within the joint on MR arthrography (Fig. 4).
POLPSA lesion in a 21-year-old man who had undergone two episodes of traumatic posterior dislocations. Axial T1-weighted (517/14 ms) fat-saturated MR arthrographic image demonstrates the posteroinferior labral avulsion (white arrow) and the adjacent scapular periosteal sleeve (black arrow). There is also a divot in the anteromedial humeral head (black arrowheads), in keeping with a small reverse Hill–Sachs lesion
Kim’s lesion
This is a deep/intrasubstance detachment of the posteroinferior labrum from the posterior glenoid rim, with a separate marginal crack on the surface. Kim et al. [18–20] described four types of posteroinferior labral tears in association with PSI on arthroscopy:
-
Type I
Incomplete detachment without displacement of the posteroinferior labrum.
-
Type II
Also called the Kim’s lesion (Figs. 5 and 6), it is associated with a marginal crack. The marginal crack is a superficial tear between the posteroinferior labrum and the articular cartilage. The clinical significance of the Kim’s lesion is the need to convert this apparently concealed lesion to a complete tear before repairing it. Failure to recognize this lesion may result in persistent posterior instability. On MR arthrogram, the Kim’s lesion demonstrated a combination of incomplete labral avulsion, loss of labral height, and seemingly intact chondrolabral junction (Fig. 6) [18].
-
Type III
Associated with a chondrolabral erosion.
-
Type IV
Flap tear of the posteroinferior labrum.
a-b Kim’s lesion in a 23-year-old man with PSI. Axial proton density (PD)-weighted MR image with the arm in flexion, adduction and internal rotation (a) and double oblique axial T1-weighted fat-saturated MR image (b) demonstrate incomplete deep avulsion or cystic lesion (white arrow) at the posteroinferior labrum at the 8 o’clock position and partial filling-in with gadolinium (black arrow) with seemingly intact chondrolabral junction
The Kim’s triad consists of marginal crack or chondral erosion, chondrolabral retroversion, and incomplete and concealed avulsion of the posteroinferior labrum (Figs. 7 and 8) [19]. It is not clear if the chondrolabral retroversion is of developmental origin or is secondary to recurrent subluxation of the humeral head [18]. The posteroinferiorly directed forces exerted on the posteroinferior labrum initiate labral tears from the deep portion (Fig. 6). The tear may not extend to involve the superficial portion of the chondrolabral junction initially and, hence, could be missed arthroscopically if the deep portion is not probed. MR imaging helps the detection of these deep portion tears of the labrum. Subsequently, recurrent posterior subluxation of the humerus on the concealed avulsion of the glenoid labrum creates a marginal crack in the chondrolabral junction (Figs. 5 and 8).
A 29-year-old man with PSI. He presented with posterior shoulder pain and had a history of sports trauma. Axial proton density (PD)-weighted (3,050/38 ms) MR image demonstrates two features of the Kim’s triad, including chondral erosion (white arrow) and adjacent incomplete labral detachment (black arrowhead). Also, note the presence of edema at the inferior infraspinatus (black arrows), in keeping with a strain injury
Kim’s lesion in a 46-year-old man with PSI. Axial proton density (PD)-weighted (3,450/38 ms) MR image demonstrates the triad of marginal crack, incomplete labral detachment and labral retroversion (white arrows) at the posteroinferior glenoid. There is also posterior translation of the center of the humeral head (white star), with respect to the glenoid, of approximately 12 mm
Posterior glenolabral articular disruption lesion
A glenolabral articular disruption (GLAD) lesion typically occurs along the anteroinferior aspect of the glenoid. Similar lesions involving the posteroinferior glenoid (Fig. 9) have been described recently, which can be associated with posterior instability [21–23]. MR imaging shows focal defects of the articular cartilage between the 7 o’clock and 9 o’clock positions of the glenoid (Figs. 10), associated with subtle tear of the labrum. It is speculated that this lesion could be due to impaction on the posteroinferior glenoid by an internally rotated humerus [21]. Patients with articular cartilage defects in the setting of PSI tend do less well postoperatively and would need appropriate preoperative counseling [23].
a, b Posterior GLAD lesion in a 34-year-old man with PSI. He presented with posterior shoulder pain and fatigue of the shoulder with activity. Axial proton density (PD)-weighted (3,000/30 ms) and coronal PD-weighted (3,100/36 ms) MR arthrographic images demonstrate chondral defect (black arrow) with associated subchondral marrow edema (white arrow) and adjacent subtle labral tear (black arrowhead)
Extensive posterior labral tears
Extensive labral tears that involve the posterior labrum, such as the superior labrum anterior to posterior (SLAP) types VIII and IX, 270°–360° labral tears of the shoulder, can be associated with instability (Figs. 11 and 12) [24–26]. Posterior labral tears extending > 15 mm in length are significantly associated with PSI [27]. Defining the extent of the extensive labral tears accurately can help in pre-surgical planning, so as to avoid incomplete labral repair.
a, b SLAP type VIII in a 45-year-old man with PSI. Double oblique axial T1-weighted (450/11 ms) fat-saturated MR arthrographic images at the level of the superior glenoid (a) and inferior glenoid (b) show the labral detachment (white arrow) involving the superior labrum and extending to involve the posteroinferior labrum. Also, note osteophytic spurs in the inferior humeral head (white arrowheads), in keeping with secondary degenerative change
Non-classifiable posteroinferior labral tears
Similar to what has been observed in anteroinferior labral tears in patients with anterior instability [28], some posteroinferior labral tears associated with PSI may not be classifiable to any of the types mentioned above. These tears demonstrate irregular morphology, including thickening/blunting and/or fibrillations on MR imaging, without a definite glenolabral detachment.
Capsular lesions and abnormalities
Reverse glenoid avulsion of the glenohumeral ligament lesion
Reverse glenoid avulsion of the glenohumeral ligament (GAGL) lesion is the posterior equivalent of the anterior counterpart, with a ligamentous avulsion (Fig. 13) as opposed to a labroligamentous avulsion [29]. There is capsular and synovial stripping from the posteroinferior labrum [4, 15]. MR arthrography demonstrates glenoid side tears of the posterior capsule/PIGHL (Figs. 14 and 15) from the posteroinferior labrum, with intact chondrolabral junction.
Reverse GAGL lesion in a 24-year-old-woman with PSI. Double oblique axial T1-weighted (733/12 ms) fat-saturated MR arthrographic image demonstrates that the PIGHL (white arrowheads) has avulsed from the otherwise intact labrum (white arrow) and carries with it the stripped scapular periosteum (black arrows)
Bennett lesion
The Bennett lesion is commonly an asymptomatic finding in throwing athletes such as baseball pitchers [30]. It is characterized by a crescent-shaped extra-articular focus of mineralization at the posteroinferior aspect of the glenoid (Fig. 16). The mineralization is in close proximity to the PIGHL, and the lesion is thought to arise due to traction on the PIGHL produced by posterior subluxation during the cocking or follow-through phase [31, 32]. Bennett lesions are frequently associated with tears of the posterior labrum in symptomatic shoulders. The Bennett lesion may not be readily apparent on MR imaging, and the diagnosis is usually made on CT scans (Fig. 17). A recent study has shown that shoulders with asymptomatic Bennett lesions demonstrate posterior joint tightness and internal rotation deficit [33]. Also in the same study, the presence of posterior joint laxity and absence of internal rotation deficit were found to be useful clinical features to suggest a painful Bennett lesion, suggesting that excessive motion of the humeral head due to posterior laxity at the follow-through phase of the throwing action could contribute to the pain [33].
Abnormalities of glenoid morphology
Posterior glenoid rim deficiency
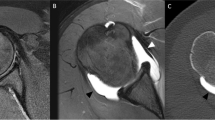
Weishaupt et al. [34] demonstrated that patients with recurrent atraumatic posterior shoulder instability had an osseous deficiency of the posteroinferior glenoid rim. From a morphologic viewpoint, they found two shapes of the posteroinferior glenoid, the lazy J and the delta, to be more common in shoulders with PSI than in control subjects with stable shoulders or anterior instability (Fig. 18). The craniocaudal extent of the osseous deficiency measured > 12 mm in patients with recurrent atraumatic posterior subluxation. CT is more useful than MR imaging in defining such osseous deficiencies of the glenoid (Figs. 19 and 28a) [35]. It is debatable whether the deficient posterior glenoid rim is a congenital abnormality or a consequence of recurrent PSI.
a–c Diagrams showing the different morphologic types of posterior glenoid rims (modified from reference [34]). a demonstrates the pointed form (without glenoid rim deficiency), b demonstrates the rounded glenoid rim deficiency (“lazy J” form), and c demonstrates the triangular bony deficiency (“delta” form)
Hypoplasia of the glenoid neck of the scapula
Glenoid hypoplasia of the neck of the scapula is a developmental anomaly associated with shoulder pain and multidirectional/posterior instability [36]. It consists of incomplete ossification of the lower two-thirds of the bony glenoid and scapular neck, with smooth articular surface of the glenoid, and abnormal hypertrophied posterior labrum. Glenoid hypoplasia is commonly bilateral and symmetric [36]. MR imaging demonstrates abnormal tissue of heterogeneous signal intensity, consistent with a combination of fibrocartilage and fat, compensating for the osseous hypoplasia (Fig. 20) [37]. Patients with glenoid hypoplasia have increased incidence of posterior labral tears [38]. Whilst some authors differentiate limited dysplasia of the posterior glenoid rim from fully developed glenoid dysplasia [34], others suggest the likelihood of a spectrum of posteroinferior glenoid osseous deficiencies, ranging from mild posterior glenoid rim deficiency to a hypoplastic glenoid neck [38].
a, b Glenoid neck hypoplasia in a 50-year-old man. Sagittal T1-weighted (700/11 ms) (a) and axial proton density (PD)-weighted (3,667/37 ms) fat-saturated (b) MR images demonstrate bony hypoplasia of posterior glenoid and scapular neck (white arrowheads). There is hypertrophy of the posterior labrum (black arrow), with labral detachment (black arrowhead). At the site of hypoplasia, there is abnormal tissue (white arrows), consistent with a combination of fibrous tissue, cartilage and fat
Glenoid retroversion
Increased retroversion of the glenoid in the mid- and inferior aspects, leading to some loss of containment of the humeral head, has been noted to be an invariable finding in shoulders with atraumatic PSI [34, 39]. It is uncertain if the retroversion of the labrum in patients with PSI is a cause or an effect of the instability, although the latter theory is favored by some authors [39]. The axial fluid-sensitive sequence images obtained at the mid- and inferior glenoid levels are used for measurement of the glenoid version (Fig. 21) [39]. Correction of the labral retroversion by capsulolabroplasty can restore the humeral head containment [19].
Diagram (modified from reference [39]) shows a method for measuring the glenoid version of both the chondrolabral and osseous portions. The black line (3) is a reference line representing the plane of the chondrolabral portion of the glenoid; the blue line (1) is a reference line representing the plane of the body of the scapula, and the red line (4) is a reference line representing the plane of the osseous glenoid. The angle between the black line (3) and the interrupted blue line (2) (line 2 is drawn perpendicular to line 1) represents the version of the chondrolabral portion of the glenoid. The angle between lines 2 and 4 measures the version of the osseous glenoid
Reverse osseous Bankart lesion
This is seen with traumatic posterior dislocations and can range from avulsion-type rim fractures of the posteroinferior glenoid to large comminuted fractures that may malunite (Figs. 22 and 23). Reverse osseous Bankart lesions may suggest the need for an open surgical approach [4, 7]. CT is useful in accurately quantifying the glenoid bone loss (Fig. 22) [40].
a, b Reverse bony Bankart lesion in a 30-year-old-man with recurrent posterior dislocations. Axial (a) and sagittal (b) CT images in bone window settings demonstrate flattening of the posteroinferior glenoid (black arrows). Note the presence of osseous debris in the posteroinferior aspect of the joint (black arrowheads)
a, b Reverse bony Bankart lesion in a 25-year-old-man. Axial proton density (PD)-weighted (3,000/29 ms) fat-saturated (a) MR image and sagittal CT image (b) in bone window settings demonstrate an avulsion osteochondral fracture (white arrows) of the posteroinferior glenoid at the site of attachment of the PIGHL
Humeral side abnormalities
Reverse Hill–Sachs lesion
The reverse Hill-Sachs lesion (also sometimes called the trough lesion or McLaughlin’s fracture) is a consequence of traumatic PSI and results from an impression fracture (Fig. 4) involving 10–30% of the articular surface of the anterior humeral head [41]. This lesion is seen in only 10% to 15% of cases of acute unidirectional posterior dislocation of the shoulder and is associated with higher grades of PSI [14, 20, 41]. The anterior humeral defect can catch on the posterior surface of the joint during internal rotation, resulting in posterior subluxation of the humeral head, thus causing gradual wear of the humeral head and tear of the posterior labrum (Fig. 24) [17].
Reverse humeral avulsion of the glenohumeral ligament and floating PIGHL lesions
The reverse humeral avulsion of the glenohumeral ligament (RHAGL) lesion is also called the posterior band inferior glenohumeral ligament avulsion from the humerus (PHAGL) lesion [42–47]. The PIGHL is an inconsistently present band of the inferior glenohumeral ligament complex and is the thinnest part of the ligament [48]. It is an important soft tissue restraint to posterior subluxation of the humeral head. Tear of the PIGHL could be associated with posterior or multidirectional instability. The RHAGL lesion is identified by a discontinuity of the PIGHL from the humerus (Fig. 25). The retracted part of the PIGHL may be identified in the posterior recess of the joint (Fig. 26). Lack of awareness of this lesion can frequently lead to non-detection pre-surgically on MR arthrogram [43, 45]. Another importance of the RHAGL lesion is that it can be missed on arthroscopy if anterior ports are not used for visualization of the posterior capsular structures [49]. The presence of concurrent RHAGL lesion and a Bankart/variant posterior labral tear (Figs. 27 and 28) is termed a floating posterior inferior glenohumeral ligament (FPIGHL) lesion [50]. It is not uncommon to see associated posterior labral tears in the presence of a RHAGL lesion [43, 45, 51].
a, b A RHAGL lesion in a 28-year-old man (elite athlete; professional football player) with PSI. Coronal proton density (PD)-weighted (2,950/25 ms) fat-saturated (a) and sagittal T1-weighted (633/10 ms) fat-saturated (b) MR arthrographic images demonstrate the humeral-sided tear and retraction of the PIGHL (black arrows). There is inferomedial extravasation of gadolinium (white arrows) associated with this RHAGL lesion, causing an irregular outline of the inferior recess
a, b Floating PIGHL lesion in a 24-year-old man with PSI, who presented with a history of recurrent posterior dislocations. Axial proton density (PD)-weighted (3,000/45 ms) fat-saturated (a) MR arthrographic image demonstrates the RHAGL lesion with retraction of the PIGHL (white arrows) from the expected humeral attachment site (white arrowheads). There is a posterior labral detachment (black arrow) and a triangular deficiency of the posteroinferior glenoid (“delta” form) (black arrowheads). The arthroscopic image (b) shows the RHAGL lesion with exposure of the teres minor (bottom right of the image)
Other miscellaneous findings in PSI
Posterior capsular laxity
A patulous posterior capsule is the most common primary pathologic abnormality in PSI [6, 52]. Laxity and some redundancy of the posterior capsule without (Fig. 29) or with (Fig. 30) tears of the labroligamentous structures can be seen in cases of recurrent posterior subluxation, leading to posterior instability [1, 4, 6, 52]. Although there is still a lack of objectivity in defining a patulous posterior recess on MR imaging, a recent article has proposed some methods to calculate the capsular cross-sectional areas on MR arthrographic images, which were found to be significantly increased in patients with PSI in comparison with control patients with stable shoulders [53].
a, b An 18-year-old woman with PSI. She had a history of bilateral recurrent posterior shoulder subluxations and a clinical diagnosis of benign joint hypermobility syndrome (Beighton score 5/9). Axial proton density (PD)-weighted fat-saturated (a) and sagittal T1-weighted fat-saturated (b) MR arthrographic images of the right shoulder demonstrate a patulous posterior recess of the joint (white arrows), in keeping with posterior capsular laxity. No labroligamentous lesions were present
a, b A 35-year-old man with posteroinferior instability. Sagittal T1-weighted (650/10 ms) fat-saturated (a) and coronal T1-weighted (517/11 ms) fat-saturated (b) MR arthrographic images of the left shoulder demonstrate a patulous posteroinferior recess (black arrows) relative to other recesses, which were tight. There is also posteroinferior labral detachment (white arrow)
Injuries to the rotator cuff and muscles
Tears of the posterior cuff, especially the teres minor and inferior infraspinatus, can frequently accompany posterior capsular tears [46, 54]. These injuries are manifested either as edema on the fluid-sensitive sequence (Fig. 7) or as gadolinium-filled gaps on the MR arthrogram (Fig. 31). Subscapularis tears could be seen in recurrent traumatic dislocations (Fig. 31). This may have clinical implications, because strengthening of the subscapularis can add to posterior glenohumeral stability [10]. Injuries to the rotator interval may also be seen in the setting of recurrent posterior dislocations on MR arthrogram (Fig. 31). Closure of the rotator interval is sometimes performed in the setting of posteroinferior instability [18, 19].
A 21-year-old man (same patient as in Fig. 4) who had undergone two episodes of traumatic posterior dislocations. Sagittal T1-weighted (550/10 ms) fat-saturated MR arthrographic image demonstrates the tear of the teres minor, with gadolinium filling in the gap (white arrows). There is also a tear and some redundancy of the posterior capsular recess (black arrow), a tear of the subscapularis (white arrowhead), and a patulous rotator interval (black arrowhead)
Posterior humeral translation
Tung and Hou [27] demonstrated that, in patients with clinical PSI, there may be associated excessive posterior humeral translation that is demonstrable on MR imaging (Fig. 32). The center of the humeral head is translated 4 mm more posteriorly, on average, in patients with posterior labral tears than in those without tears and 2.5 mm or more in patients with PSI than in those without PSI (Fig. 8).
Diagram (modified from reference [27]) shows a method for calculating the position of the humeral head in relation to the glenoid. Arrows point to a line connecting the anterior and posterior edges of the glenoid. The center of the humeral head is represented by X. The dotted line is a tangential line through the anterior surface of the scapula, bisecting the line pointed to by the arrows. In PSI, the X is significantly posterior to the dotted line extended into the humeral head
Treatment
A non-operative approach is usually recommended as the initial treatment option for symptomatic PSI [5, 6]. This includes some modification of shoulder activity, scapular stabilization, and physiotherapy to strengthen the posterior cuff muscles and the deltoid. Operative treatment of PSI is usually only considered in those who remain significantly symptomatic and disabled after failing to respond to an adequate and prolonged trial of non-surgical treatment [4]. Operative stabilizations have been proven to be more successful if aimed at the precise anatomic lesions present [7, 12]. The classification of PSI based on direction is crucial in surgical decision-making [6]. For example, if there is pure PSI, an operative technique correcting the redundant posterior capsule would be necessary. In situations of posteroinferior instability with intact anterior component and rotator interval, a posteroinferior capsular shift may be appropriate. In patients with multidirectional instability, the operative approach is determined by the primary location of the symptoms (Fig. 33). When there is primary anterior and posterior instability, rarely a combined anterior and posterior capsular shift procedure may need to be performed.
a–c A 26-year-old man with primary anterior and secondary posterior instability. Axial proton density (PD)-weighted fat-saturated (a) and coronal PD-weighted fat-saturated (b, c) MR arthrographic images demonstrate the RHAGL lesion with retraction of the posterior capsule (black arrows), patulous posterior recess (white arrows), anterior labroligamentous periosteal sleeve avulsion (ALSPA) lesion (white arrowheads) and an intra-articular loose body (black arrowheads)
Conclusion
PSI, although more uncommon than anterior instability, contributes to significant patient morbidity and is more prone to failure of both surgical and non-surgical treatment. Recognition of the cause, degree and direction are essential for proper treatment planning and to prevent recurrent instability. Recognition of lesions contributing to and associated with PSI can be identified in detail with MR imaging, particularly MR arthrography, and, thus, aid in the diagnosis and treatment of the same.
References
Robinson CM, Aderinto J. Recurrent posterior shoulder instability. J Bone Joint Surg Am 2005; 87: 883–892.
Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med 2007; 35: 1168–1173.
Bottoni CR, Franks BR, Moore JH, DeBerardino TM, Taylor DC, Arciero RA. Operative stabilization of posterior shoulder instability. Am J Sports Med 2005; 33: 996–1002.
Antoniou J, Harryman DT 2nd. Posterior instability. Orthop Clin North Am 2001; 32: 463–473.
Tibone JE, Bradley JP. The treatment of posterior subluxation in athletes. Clin Orthop Relat Res 1993; 291: 124–137.
Lamar DS, Williams GR, Iannotti JP, Ramsey ML. Posterior instability of the glenohumeral joint: diagnosis and management. Univ Pa Orthop J 2001; 14: 5–14.
Vidal LB, Bradley JP. Management of posterior shoulder instability in the athlete. Curr Opin Orthop 2006; 17: 164–171.
Fronek J, Warren RF, Bowen M. Posterior subluxation of the glenohumeral joint. J Bone Joint Surg Am 1989; 71: 205–216.
Lewis A, Kitamura T, Bayley I. The classification of shoulder instability: new light through old windows! Curr Orthop 2004; 18: 97–108.
Blasier RB, Soslowsky LJ, Malicky DM, Palmer ML. Posterior glenohumeral subluxation: active and passive stabilization in a biomechanical model. J Bone Joint Surg Am 1997; 79: 433–440.
Harryman DT 2nd, Sidles JA, Harris SL, Matsen FA 3rd. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am 1992; 74: 53–66.
Papendick LW, Savoie FH 3rd. Anatomy-specific repair techniques for posterior shoulder instability. J South Orthop Assoc 1995; 4: 169–176.
Amrami KK, Savcenko V, Dahm DL, Sundaram M. Radiologic case study. Reverse Bankart lesion with posterior labral tear. Orthopedics 2002; 25: 720, 779–780.
Williams RJ 3rd, Strickland S, Cohen M, Altchek DW, Warren RF. Arthroscopic repair for traumatic posterior shoulder instability. Am J Sports Med 2003; 31: 203–209.
Antoniou J, Duckworth DT, Harryman DT 2nd. Capsulolabral augmentation for the management of posteroinferior instability of the shoulder. J Bone Joint Surg Am 2000; 82: 1220–1230.
Yu JS, Ashman CJ, Jones G. The POLPSA lesion: MR imaging findings with arthroscopic correlation in patients with posterior instability. Skeletal Radiol 2002; 31: 396–399.
Simons P, Joekes E, Nelissen RG, Bloem JL. Posterior labrocapsular periosteal sleeve avulsion complicating locked posterior shoulder dislocation. Skeletal Radiol 1998; 27: 588–590.
Kim SH, Ha KI, Yoo JC, Noh KC. Kim’s lesion: an incomplete and concealed avulsion of the posteroinferior labrum in posterior or multidirectional posteroinferior instability of the shoulder. Arthroscopy 2004; 20: 712–720.
Kim SH, Kim HK, Sun JI, Park JS, Oh I. Arthroscopic capsulolabroplasty for posteroinferior multidirectional instability of the shoulder. Am J Sports Med 2004; 32: 594–607.
Kim SH, Ha KI, Park JH, et al. Arthroscopic posterior labral repair and capsular shift for traumatic unidirectional recurrent posterior subluxation of the shoulder. J Bone Joint Surg Am 2003; 85: 1479–1487.
Anderson M, Barr M, Gaskin C, Alford B. Posterior GLAD lesions of the shoulder (scientific presentation). Radiological Society of North America, 2005.
Resnick D, Kang HS, Pretterklieber ML. Shoulder. In: Internal derangement of joints, 2nd ed, vol 1. Philadelphia: Saunders; 2007: 713–1122.
Wolf BR, Strickland S, Williams RJ, Allen AA, Altchek DW, Warren RF. Open posterior stabilization for recurrent posterior glenohumeral instability. J Shoulder Elbow Surg 2005; 14: 157–164.
Mohana-Borges AV, Chung CB, Resnick D. Superior labral anteroposterior tear: classification and diagnosis on MRI and MR arthrography. AJR Am J Roentgenol 2003; 181: 1449–1462.
Lindauer KR, Major NM, Rougier-Chapman DP, Helms CA. MR imaging appearance of 180–360 degrees labral tears of the shoulder. Skeletal Radiol 2005; 34: 74–79.
Barber A, Field LD, Ryu R. Biceps tendon and superior labrum injuries: decision-making. J Bone Joint Surg Am 2007; 89: 1844–1855.
Tung GA, Hou DD. MR arthrography of the posterior labrocapsular complex: relationship with glenohumeral joint alignment and clinical posterior instability. AJR Am J Roentgenol 2003; 180: 369–375.
Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K. Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology 2005; 237: 578–583.
Stoller DW, Wolf EM, Li AE, Nottage WM, Tirman PJ. The shoulder. In: Stoller DW, ed. Magnetic resonance imaging in orthopedics and sports medicine, vol 2. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2007. p. 1131–1461.
Wright RW, Paletta GA Jr. Prevalence of the Bennett lesion of the shoulder in major league pitchers. Am J Sports Med 2004; 32: 121–124.
Ferrari JD, Ferrari DA, Coumas J, Pappas AM. Posterior ossification of the shoulder: the Bennett lesion. Etiology, diagnosis, and treatment. Am J Sports Med 1994; 22: 171–175.
De Maeseneer M, Jaovisidha S, Jacobson JA, et al. The Bennett lesion of the shoulder. J Comput Assist Tomogr 1998; 22: 31–34.
Nakagawa S, Yoneda M, Hayashida K, Mizuno N, Yamada S. Posterior shoulder pain in throwing athletes with a Bennett lesion: factors that influence throwing pain. J Shoulder Elbow Surg 2006; 15: 72–77.
Weishaupt D, Zanetti M, Nyffeler RW, Gerber C, Hodler J. Posterior glenoid rim deficiency in recurrent (atraumatic) posterior shoulder instability. Skeletal Radiol 2000; 29: 204–210.
Mulligan ME, Pontius CS. Posterior-inferior glenoid rim shapes by MR imaging. Surg Radiol Anat 2005; 27: 336–339.
Theodorou SJ, Theodorou DJ, Resnick D. Hypoplasia of the glenoid neck of the scapula: imaging findings and report of 16 patients. J Comput Assist Tomogr 2006; 30: 535–542.
Munshi M, Davidson JM. Unilateral glenoid hypoplasia: unusual findings on MR arthrography. AJR Am J Roentgenol 2000; 175: 646–658.
Harper KW, Helms CA, Haystead CM, Higgins LD. Glenoid dysplasia: incidence and association with posterior labral tears as evaluated on MRI. AJR Am J Roentgenol 2005; 184: 984–988.
Kim SH, Noh KC, Park JS, Ryu BD, Oh I. Loss of chondrolabral containment of the glenohumeral joint in atraumatic posteroinferior multidirectional instability. J Bone Joint Surg Am 2005; 87: 92–98.
Griffith JF, Yung PS, Antonio GE, Tsang PH, Ahuja AT, Chan KM. CT compared with arthroscopy in quantifying glenoid bone loss. AJR Am J Roentgenol 2007; 189: 1490–1493.
Krackhardt T, Schewe B, Albrecht D, Weise K. Arthroscopic fixation of the subscapularis tendon in the reverse Hill-Sachs lesion for traumatic unidirectional posterior dislocation of the shoulder. Arthroscopy 2006; 22: 227.e1–227.e6.
Abrams JS. Arthroscopic repair of posterior instability and reverse humeral glenohumeral ligament avulsion lesions. Orthop Clin North Am 2003; 34: 475–483.
Castagna A, Snyder SJ, Conti M, et al. Posterior humeral avulsion of the glenohumeral ligament: a clinical review of 9 cases. Arthroscopy 2007; 23: 809–815.
Chung CB, Sorenson S, Dwek JR, Resnick D. Humeral avulsion of the posterior band of the inferior glenohumeral ligament: MR arthrography and clinical correlation in 17 patients. AJR Am J Roentgenol 2004; 183: 355–359.
Safran O, Defranco MJ, Hatem S, Iannotti JP. Posterior humeral avulsion of the glenohumeral ligament as a cause of posterior shoulder instability. A case report. J Bone Joint Surg Am 2004; 86: 2732–2736.
Chhabra A, Diduch DR, Anderson M. Arthroscopic repair of a posterior humeral avulsion of the inferior glenohumeral ligament (HAGL) lesion. Arthroscopy 2004; 20 Suppl 2: 73–76.
Brown T, Barton RS, Savoie FH 3rd. Reverse humeral avulsion glenohumeral ligament and infraspinatus rupture with arthroscopic repair: a case report. Am J Sports Med 2007; 35: 2135–2139.
Ticker JB, Flatow EL, Pawluk RJ, et al. The inferior glenohumeral ligament: a correlative investigation. J Shoulder Elbow Surg 2006; 15: 665–674.
Laurencin CT, Paletta GA, Potter H, Wickiewicz TL. Disruption of the posterior-lateral shoulder capsule. J Shoulder Elbow Surg 1995; 4: 391–394.
Bui-Mansfield LT, Banks KP, Taylor DC. Humeral avulsion of the glenohumeral ligaments: the HAGL lesion. Am J Sports Med 2007; 35: 1960–1966.
Hill JD, Lovejoy JF Jr, Kelly RA. Combined posterior Bankart lesion and posterior humeral avulsion of the glenohumeral ligaments associated with recurrent posterior shoulder instability. Arthroscopy 2007; 23: 327.e1–327.e3.
Bigliani LU, Pollock RG, McIlveen SJ, Endrizzi DP, Flatow EL. Shift of the posteroinferior aspect of the capsule for recurrent posterior glenohumeral instability. J Bone Joint Surg Am 1995; 77: 1011–1020.
Dewing CB, McCormick F, Bell SJ, et al. An analysis of capsular area in patients with anterior, posterior, and multidirectional shoulder instability. Am J Sports Med 2008; 36: 515–522.
Hottya GA, Tirman PF, Bost FW, et al. Tear of the posterior shoulder stabilizers after posterior dislocation: MR imaging and MR arthrographic findings with arthroscopic correlation. AJR Am J Roentgenol 1998; 171: 763–768.
Acknowledgments
We extend special thanks to Glen Oomen for preparation of the illustrations. We wish to thank Joanna Andrews and David Wormald for the small financial contribution from the Dept. of Diagnostic Imaging, St. Joseph’s Healthcare towards preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harish, S., Nagar, A., Moro, J. et al. Imaging findings in posterior instability of the shoulder. Skeletal Radiol 37, 693–707 (2008). https://doi.org/10.1007/s00256-008-0487-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-008-0487-7