Abstract
Objective
The objective was to correlate radiographic findings with magnetic resonance imaging (MRI) findings in patients with suspected tibial stress injuries in order to determine the significance of radiographic signs of stress injury in these individuals.
Patients and methods
The study group consisted of 80 patients with suspected tibial stress injuries who underwent a radiographic and MR examination of the tibia. Nineteen patients had bilateral involvement. Thus, a total of 99 tibias were evaluated. All radiographs and MR examinations were retrospectively reviewed, 1 month apart, in consensus by two musculoskeletal radiologists. The radiographs were reviewed without knowledge of the site of the clinical symptoms. Fisher’s exact tests were used to determine the association between a positive radiograph and the presence of various MRI signs of a high-grade stress injury.
Results
There was a strong association between the presence of periosteal reaction on radiographs at the site of the clinical symptoms and a Fredericson grade 4 stress injury on MRI.
Conclusions
The presence of periosteal reaction on radiographs at the site of clinical symptoms is predictive of a high-grade stress injury by MRI criteria.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stress injuries represent a spectrum of osseous abnormalities that occur in response to chronic repetitive stress applied to healthy bone. Stress injuries are common in athletes and represent approximately 10% of all injuries seen in sports medicine clinics. Running is the activity most commonly associated with these injuries. The vast majority of stress injuries involve the tibia followed in order of decreasing frequency by the tarsal bones, metatarsals, femur, and fibula [1].
Radiographs are commonly used to evaluate patients with suspected tibial stress injuries. Radiographic manifestations of stress injuries include decreased cortical density, periosteal reaction, endosteal thickening, and a cortical fracture line [2–5]. However, radiographs are insensitive for detecting early tibial stress injuries and are initially negative in the vast majority of symptomatic patients [6–9]. For this reason, most patients with clinical signs and symptoms of tibial stress injuries who have normal radiographs are further evaluated with more sensitive imaging modalities.
Nuclear medicine scintigraphy and computed tomography (CT) have long been used to evaluate patients with suspected tibial stress injuries. Bone scans show increased radionuclide uptake at sites of tibial stress injuries days to weeks before radiographic abnormalities become apparent [2, 3, 6–11]. CT is superior to radiographs at detecting early periostitis and cortical abnormalities in patients with tibial stress injuries [12]. However, both imaging modalities may occasionally appear normal during the early stages of stress injury [11–14]. For this reason, magnetic resonance imaging (MRI) has become the modality of choice at most institutions for evaluating patients with suspected tibial stress injuries [15–19]. MRI is more sensitive than nuclear medicine scintigraphy and CT for detecting early stress injuries [12]. MRI can also be used to grade the severity of the stress injury and thereby assist in clinical management [20].
Despite their low sensitivity, radiographs remain the initial imaging study obtained at most institutions when evaluating patients with suspected tibial stress injuries. [2, 3, 6–10, 12]. The usefulness of radiographs in the initial evaluation of these individuals is presently unknown. It would be helpful to identify which MRI findings are present in patients with radiographic evidence of tibial stress injuries on initial imaging studies. In this way, the significance of a positive radiograph in these individuals could be determined. Thus, this study was performed to determine if there was a consistent and predictable relationship between the presence of radiographic findings of tibial stress injury and the severity of the stress injury as assessed by MRI.
Patients and methods
Study group
The study was performed in compliance with HIPAA regulations and with approval from our Institutional Review Board. A waiver of informed consent was obtained prior to performing the study.
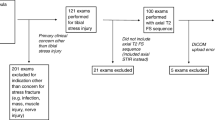
A musculoskeletal MRI database was used to identify 131 consecutive patients who were referred for an MRI examination of the lower extremity at our institution between 1 January 1998 and 1 March 2006 to rule out tibial stress injury. Eighty of these 131 patients had a radiographic examination of the tibia performed within 2 weeks of their MRI examination. The study group consisted of these 80 patients (21 males and 59 females; aged between 14 years and 44 years with an average age of 22 years) with suspected tibial stress injuries who were evaluated with radiographs and MRI. Nineteen patients complained of bilateral tibial pain and had imaging studies performed on both lower extremities. Thus, a total of 99 tibias were evaluated with radiographs and MRI.
All 80 patients in the study group were evaluated by a sports medicine specialist at our institution. All patients were athletes involved in sports activities that included long distance running, sprinting, pole vaulting, high jumping, basketball, soccer, and dancing. All patients complained of focal pain within the tibia (duration of clinical symptoms ranging between 4 days and 600 days with an average duration of 61 days), which was exacerbated by physical activity. All patients had point tenderness over the tibia on physical examination. None of the patients had a history of acute trauma to the lower extremity or had clinical manifestations to suggest the presence of infection or malignancy.
Radiographic examination
All patients in the study group underwent a radiographic examination of the tibia at the time of presentation to their physician. Twenty radiographic examinations consisted of anteroposterior and lateral views of the tibia, while the remaining 79 examinations consisted of anteroposterior, lateral, internal oblique, and external oblique views of the tibia. All radiographs were performed using a standardized technique [21]. A radio-opaque marker was not placed at the site of the patient’s maximal pain to localize symptoms during the radiographic examinations.
MRI examination
All patients in the study group underwent an MRI examination of the tibia within 2 weeks of their radiographic examination. All MRI examinations were performed on the same General Electric 1.5 Tesla field strength magnet (General Electric Medical Systems, Milwaukee, WI, USA) using a phased array extremity coil. All MRI examinations included an axial T1-weighted spin-echo sequence (TR/TE: 400–600 ms/15–30 ms) and fat-suppressed T2-weighted fast spin-echo sequence (TR/TE: 2,000–4,000 ms/60–80 ms, echo train of 8). All MRI examinations also included a T1-weighted spin-echo sequence (TR/TE: 400–600 ms/15–30 ms) and either a fat-suppressed T2-weighted fast spin-echo sequence (TR/TE: 2,000–4,000 ms/60–80 ms, echo train of 8) or short tau inversion recovery sequence (TI/TR/TE: 160 ms/3,000 ms/44 ms, echo train of 8) performed in the coronal and/or sagittal planes. All fat-suppressed T2-weighted fast-spin echo sequences were performed using a frequency selective chemical presaturation pulse (ChemSat; General Electric Medical Systems) to suppress signal from adipose tissue. All MRI examinations were performed with a field of view between 16 cm and 24 cm, a slice thickness between 3 mm and 7 mm with an interslice gap between 0.4 mm and 3 mm, a matrix of 256 × 192 or 256 × 256, and one or two excitations. During each MR I examination, a vitamin E capsule was placed at the site of the patient’s maximal pain to localize symptoms.
Review of MRI examinations
All MRI examinations were retrospectively reviewed in consensus by two fellowship-trained academic musculoskeletal radiologists who had between 4 and 7 years of clinical experience. The radiologists were unaware of the radiographic findings of each patient when retrospectively reviewing their MRI examination.
The radiologists determined the presence or absence of periosteal edema, bone marrow edema, and intracortical signal abnormality within the tibia on each MRI examination. Periosteal edema was defined as a linear area of high T2 signal intensity immediately adjacent to the outer surface of the tibial cortex. Bone marrow edema was defined as a focal or ill-defined area of low T1 signal intensity and high T2 signal intensity within the intramedullary canal of the tibia. Intracortical signal abnormality was defined as globular or linear areas of intermediate T1 signal intensity and intermediate to high T2 signal intensity within the tibial cortex. The radiologists also graded the severity of the tibial stress injuries using the Fredericson MR Classification System (Table 1) [20].
When periosteal edema was present on the tibial cortex, the radiologist assessed its severity using two separate methods. The periosteal edema was considered to be mild if it involved less than 25% of the circumference, moderate if it involved between 25% and 50% of the circumference, and severe if it involved more than 50% of the circumference of the tibial cortex on axial fat-suppressed T2-weighted fast spin-echo MR images. The maximal thickness of the periosteal edema was also measured on axial fat-suppressed T2-weighted fast spin-echo MR images perpendicular to the cortical surface of the tibia using electronic calipers on an ALI workstation (Horizon Medical Imaging Systems, Version 5; McKesson Corporation, San Francisco, CA, USA).
When bone marrow edema was present within the tibia, the radiologists assessed its severity using two separate methods. The bone marrow edema was considered to be mild if it involved less than 25% of the total cross-sectional area, moderate if it involved between 25% and 50% of the total cross-sectional area, and severe if it involved more than 50% of the total cross sectional area of the intramedullary canal of the tibia on axial fat-suppressed T2-weighted fast spin-echo MR images. The maximal longitudinal length of the bone marrow edema was also measured on sagittal or coronal fat-suppressed T2-weighted fast spin-echo or short tau inversion recovery MR images using electronic calipers on an ALI workstation (Horizon Medical Imaging Systems, Version 5; McKesson Corporation).
Review of radiographic examination
All radiographs were retrospectively reviewed in consensus by the same two fellowship-trained musculoskeletal radiologists. The radiologists were unaware of the clinical findings and MRI findings of each patient when retrospectively reviewing their radiographic examination. In order to prevent recall bias, the radiologists reviewed the radiographic examination of each patient at least 1 month after reviewing their MRI examination.
The radiologists determined the presence or absence of decreased cortical density, periosteal reaction, endosteal thickening, and a cortical fracture line within the tibia on each radiographic examination. When a radiographic abnormality was identified, the radiologists documented its location within the proximal, mid, and distal tibia and within the anterior, posterior, medial, or lateral tibia. The radiologists also documented on which view the abnormality was best visualized.
When periosteal reaction was identified on the tibial cortex, the radiologists documented whether it was smooth or irregular in contour. Irregular periosteal reaction was considered to include periosteal reaction, which was lamellated or which had an ill-defined periphery or jagged outline. The radiologists also documented whether the periosteal reaction was of equal or lower density than the adjacent cortical bone. In addition, the thickness of the periosteal reaction was measured perpendicular to the cortical surface of the tibia using electronic calipers on an ALI workstation (Horizon Medical Imaging Systems, Version 5; McKesson Corporation, San Francisco, CA).
All radiographs on which abnormalities within the tibia were identified on the initial retrospective review were reviewed in consensus a second time at a separate sitting by the same two fellowship-trained musculoskeletal radiologists. During the second review, the radiologists correlated the radiographic findings with clinical symptoms and MRI findings. Each radiographic abnormality identified on the initial review was determined to be concordant or discordant with the patient’s clinical symptoms and MRI findings. A radiographic abnormality was considered to be concordant with clinical symptoms if it was located at the same site as the patient’s maximal pain, as determined by the location of the vitamin E capsule on the MR examination. A radiographic abnormality was considered to be concordant with the MRI findings if they were located at the same site within the tibia.
Statistical analysis
The sensitivity with 95% confidence intervals of radiographs for detecting symptomatic tibial stress injuries was calculated using MRI as the gold standard. Sensitivity was defined as the proportion of individuals with MRI findings of tibial stress injury who had a concordant abnormality identified on radiographs.
T-tests were used to compare the duration of clinical symptoms in patients with and without a positive radiograph. A positive radiograph was defined as a radiograph that showed an abnormality that corresponded to the location of the patient’s clinical symptoms and MRI abnormalities. A difference in the duration of clinical symptoms in patients with and without a positive radiograph was considered to be statistically significant if the p value was less than 0.01.
Fisher’s exact tests were used to compare the proportion of patients with and without a positive radiograph who had various MRI findings indicating a severe tibial stress injury. These MRI findings included severe periosteal edema, periosteal edema more than 2 mm thick, severe bone marrow edema, bone marrow edema more than 5 cm in longitudinal length, intracortical signal abnormality, and a Fredericson grade 4 stress injury. A positive radiograph was defined as a radiograph that showed an abnormality that corresponded to the location of the patient’s clinical symptoms and MRI abnormalities. A difference in the proportion of patients with and without a positive radiograph who had the various MRI findings was considered to be statistically significant if the p value was less than 0.01. Fisher’s exact tests were also used to calculate odds ratios and 95% confidence intervals describing the relative risk of a patient with a positive radiograph having these MRI findings compared with a patient without a positive radiograph.
Results
Radiographic and MRI findings
The grades of the stress injuries of the 99 tibias evaluated in the study according to the Fredericson MR Classification System are summarized in Table 2 [20].
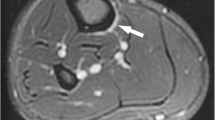
Eighty-six tibias showed abnormalities on MRI indicating a stress injury. The MRI abnormalities in all 86 tibias corresponded to the location of the patients’ clinical symptoms. None of the 86 tibias showed decreased cortical density, endosteal thickening, or a cortical fracture line on radiographs. Thirty-three of the 86 tibias showed periosteal reaction on radiographs. Thirteen of these 33 tibias showed concordant periosteal reaction that corresponded to the location of the patient’s clinical symptoms and MRI abnormalities (Fig. 1). Twenty of these 33 tibias showed a discordant periosteal reaction that did not correspond to the location of the patient’s clinical symptoms and MRI abnormalities (Fig. 2). The radiographic appearance of the concordant and discordant periosteal reaction is summarized in Table 3.
Thirty-two-year-old male marathon runner with pain and focal tenderness in the proximal tibial diaphysis. a Lateral radiograph of the tibia shows periosteal reaction (arrow) at the proximal tibial diaphysis. Corresponding b sagittal and c coronal fat-suppressed T2-weighted fast spin-echo MR images of the tibia show bone marrow edema (large arrows) and periosteal edema (small arrows) in the proximal tibial diaphysis. Note that the location of the patient’s MRI abnormalities corresponds to the location of the periosteal reaction. d Corresponding axial fat-suppressed T2-weighted fast spin-echo MR image of the tibia shows bone marrow edema (large arrow) and periosteal edema (small arrows) in the tibial diaphysis. Also note the signal abnormality (arrowhead) within the posterior tibial cortex
Twenty-two-year-old male college cross-country runner with pain in the anterior aspect of the distal tibial diaphysis. a Anteroposterior radiograph of the tibia shows periosteal reaction (arrow) at the proximal tibial diaphysis. Corresponding b sagittal and c coronal fat-suppressed T2-weighted fast spin-echo MR images of the tibia show bone marrow edema (large arrows) and periosteal edema (small arrows) in the distal tibial diaphysis. Note that the location of the patient’s clinical symptoms (arrowhead in b) and MRI abnormalities does not correspond to the location of the periosteal reaction
In the 13 tibias with concordant periosteal reaction, the periosteal reaction was located in the proximal diaphysis in 5 tibias, the mid diaphysis in 7 tibias, and the distal diaphysis in 1 tibia. The periosteal reaction was located on the anterior cortex in 1 tibia, the posterior cortex in 7 tibias, and the medial cortex in 5 tibias. The periosteal reaction was best seen on the lateral view in 9 tibias, the anteroposterior view in 2 tibias, and the oblique view in 2 tibias. Two of the 13 tibias with concordant periosteal reaction showed Fredericson grade 3 stress injuries on MRI, while the remaining 11 tibias showed Fredericson grade 4 stress injuries.
Thirteen tibias showed no abnormalities on MRI. None of the 13 tibias showed decreased cortical density, endosteal thickening, or a cortical fracture line on radiographs. Three of the 13 tibias showed discordant periosteal reaction on radiographs that did not correspond to the location of the patient’s clinical symptoms (Fig. 3). The radiographic appearance of the discordant periosteal reaction is summarized in Table 3.
Eighteen-year-old female high school cross-country runner with pain and focal tenderness in the mid tibial diaphysis. a Anteroposterior radiograph of the tibia shows periosteal reaction (arrow) at distal tibial diaphysis. Corresponding b sagittal and c coronal fat-suppressed T2-weighted fast spin-echo MR images of the tibia show no evidence of stress injury. Note that the location of the patient’s clinical symptoms (arrow in b) does not correspond to the location of the periosteal reaction
Statistical analysis
Radiographs had a sensitivity of 15% (13 out of 86 tibia; 95% confidence interval between 8% and 24%) for detecting tibial stress injury. There was no statistically significant difference (p = 0.91) in the duration of clinical symptoms in patients with and without a positive radiograph. In fact, patients with a positive radiograph had, on average, a shorter duration of clinical symptoms than patients without a positive radiograph. There was a statistically significantly higher (p < 0.01) proportion of patients with a positive radiograph than without a positive radiograph who had severe periosteal edema, periosteal edema more than 2 mm in thick, severe bone marrow edema, bone marrow edema more than 5 cm in longitudinal length, intracortical signal abnormality, and a Fredericson grade 4 stress injury. Table 4 shows the odds ratios and 95% confidence intervals describing the relative risk of a patient with a positive radiograph having various MRI findings indicating a severe tibial stress injury compared with a patient without a positive radiograph.
Discussion
Stress injuries of the tibia occur when bone does not adapt normally to repetitive stress [22]. Stress related to daily activity stimulates bone to strengthen and remodel its architecture to better withstand its mechanical environment. Normal stress stimulates osteoclastic activity that creates resorption cavities within the tibial cortex that eventually fill in with lamellar bone over the course of several months [23, 24]. Chronic repetitive stress to the tibia may result in an imbalance between osteoclastic and osteoblastic activity, which ultimately weakens bone [22]. If the repetitive stress continues, repair mechanisms may be overwhelmed and a true fracture may develop through the weakened bone [2, 22, 25]. However, most tibial stress injuries represent stress reaction and not stress fracture and show no evidence of a break in the continuity of bone on histologic analysis [26, 27]. In most cases, the chronic repetitive stress on the tibia is discontinued prior to the development of a true fracture [2, 22, 25].
Radiographs have long been used to evaluate patients with tibial stress injuries. Radiographic manifestations of tibial stress injuries include decreased cortical density, periosteal reaction, endosteal thickening, and a cortical fracture line. Decreased cortical density has been described as the earliest radiographic finding of stress injury and is thought to represent hyperemia and edema of the injured tibial cortex [4]. Periosteal or endosteal proliferation may later form at the site of repetitive stress in an attempt to buttress the weakened cortical bone. If the chronic repetitive stress continues, a true fracture through the tibial cortex may eventually occur [2].
In our study, the only radiographic finding seen in patients with tibial stress injuries was periosteal reaction. Only two previous studies have documented the radiographic findings in patients with tibial stress injuries. Giladi and associates described periosteal reaction in 11 out of 51 tibias and a cortical fracture line in 1 out of 51 tibias with stress injuries confirmed by nuclear medicine scintigraphy [6]. Fredericson and associates described areas of periosteal and endosteal new bone formation in 4 out of 12 tibias with stress injuries confirmed by MRI [20]. The fact that periosteal reaction is the most common radiographic finding of tibial stress injuries is not surprising. Decreased cortical density and endosteal thickening may be very difficult to appreciate on radiographs. Furthermore, a cortical fracture line is a late manifestation of tibial stress injuries. In most patients, the stress injuries are detected with more sensitive imaging modalities such as nuclear medicine scintigraphy or MRI before a fracture line is identified on radiographs.
Radiographs had an extremely low sensitivity for detecting tibial stress injuries in our study. Only 13 out of 86 tibias with stress injuries confirmed by MRI showed concordant periosteal reaction on radiographs. The 15% sensitivity of radiographs in our study corresponds well to previously reported sensitivity values, which have ranged between 10% and 29% for the initial radiographic examination [1, 6–9, 20]. On follow-up examinations, the sensitivity of radiographs is higher with reported values ranging between 40% and 54% [7, 9].
In our study, discordant periosteal reaction was commonly seen on radiographs in patients with suspected tibial stress injuries. Discordant periosteal reaction, which did not correspond to the location of the patient’s clinical symptoms, was present in 3 out of 13 tibias with no MRI abnormalities and in 20 out of 86 tibias with MRI findings of stress injury. The exact cause of the discordant periosteal reaction is unknown. Perhaps the periosteal reaction was secondary to prior episodes of acute or repetitive trauma to the tibia.
There was no difference in the radiographic appearance of concordant and discordant periosteal reaction in our study. The contour, density, and thickness of the periosteal reaction on radiographs were not useful for differentiating between concordant and discordant periosteal reaction. Periosteal reaction was specific for a tibial stress injury only when it occurred at the same location as the patient’s clinical symptoms. This emphasizes the need to correlate radiographic findings with clinical findings when evaluating patients with tibial stress injuries. At our institution, radio-opaque markers are now routinely used during radiographic examinations of the tibia to mark the exact location of clinical symptoms in patients with suspected stress injuries.
In our study, there was no association between the presence of concordant periosteal reaction on radiographs and the duration of clinical symptoms. Periosteal reaction forms at the site of repetitive stress in an attempt to buttress the weakened cortical bone. It would seem likely that patients with tibial stress injuries who have a longer duration of clinical symptoms would have more time for the body to respond to the weakened bone and thus would more likely have periosteal reaction on radiographs. However, the duration of clinical symptoms in patients with concordant periosteal reaction was, on average, shorter than the duration of clinical symptoms in patients without concordant periosteal reaction.
There was a strong association between the presence of concordant periosteal reaction on radiographs and the presence of various MRI findings indicative of a severe tibial stress injury. The presence of intracortical signal abnormality, which corresponds to a Fredericson grade 4 stress injury, was the MRI finding most strongly associated with the presence of concordant periosteal reaction. Patients with concordant periosteal reaction on radiographs were 26 times more likely to have signal abnormality within the tibial cortex on MRI than patients without concordant periosteal reaction.
Only one previous study has correlated radiographic findings with MRI findings in patients with suspected tibial stress injuries. Fredericson and associates described radiographic abnormalities in 4 out of 12 tibias with stress injuries confirmed by MRI. According to their MRI classification system, the radiographic abnormalities occurred in 2 tibias with grade 2 stress injuries and 2 tibias with grade 3 stress injuries [20]. In our study, radiographic abnormalities occurred in 2 tibias with Fredericson grade 3 stress injuries and 11 tibias with Fredericson grade 4 stress injuries. We cannot explain the differences in findings between the two studies. Radiographic abnormalities may occur in patients with low-grade stress injuries, as suggested by the study performed by Fredericson and associates. However, our larger cohort of patients indicates that radiographic abnormalities are much more common in patients with high-grade tibial stress injuries who have extensive periosteal and bone marrow edema and intracortical signal abnormality on MRI.
Despite their extremely low sensitivity, radiographs remain the initial imaging study obtained at most institutions when evaluating patients with suspected tibial stress injuries. Patients with concordant periosteal reaction on radiographs have a high likelihood of producing the MRI findings of a severe tibial stress injury. Thus, if periosteal reaction is identified on radiographs at the site of the patient’s clinical symptoms, it may be assumed that the patient has a high-grade stress injury and should be treated accordingly.
There are several limitations of our study. One limitation was that MRI was used as the gold standard to calculate the sensitivity of radiographs for detecting tibial stress injuries. MRI is the single best technique for evaluating patients with stress injuries [12]. However, MRI is not 100% sensitive. Previous studies have shown that CT can occasionally depict osteopenia, which is the earliest finding of a cortical stress injury, in symptomatic patients with normal MRI examinations [12]. It is quite possible that some of our patients with normal MRI examinations had tibial stress injuries. However, all patients in our study who had radiographic abnormalities, but normal MR examinations, had discordant periosteal reaction, which did not correspond to the location of their clinical symptoms. A second limitation of our study was that the retrospective review of radiographs was performed without knowledge of the exact location of the patient’s clinical symptoms. If a radio-opaque marker had been present on the radiographs to mark the location of the patient’s clinical symptoms, the radiologists may have been able to better identify subtle abnormalities within the tibia that would have increased the sensitivity of the radiographic interpretation in our study. A third limitation of our study was the relatively small number of tibias with concordant radiographic abnormalities. Only 13 of the 99 tibias in the study showed concordant periosteal reaction on radiographs. Nevertheless, the sample size was sufficient to use statistical analysis to correlate radiographic findings with MRI findings in our patients. A final limitation of our study was the presence of selection bias. Not all patients with suspected tibial stress injuries at our institution were included in the study. It is likely that some patients with clinical manifestations of tibial stress injuries who had periosteal reaction on radiographs were treated for their injuries without being further evaluated with MRI.
In conclusion, our study has shown that radiographs are rarely positive in patients with suspected tibial stress injuries. However, if a radiographic abnormality is identified at the location of a patient’s clinical symptoms, there is a high likelihood that a severe tibial stress injury is present. Thus, radiographs may be useful for predicting the severity of the stress injury and thereby assist in clinical management.
References
Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sports Med 1987; 15: 46–58.
Anderson MW, Greenspan A. Stress fractures. Radiology 1996; 199: 1–12.
Daffner RH, Martinez S, Gehweiler JA Jr., Harrelson JM. Stress fractures of the proximal tibia in runners. Radiology 1982; 142: 63–65.
Mulligan ME. The “gray cortex”: an early sign of stress fracture. Skeletal Radiol 1995; 24: 201–203.
Sofka CM. Imaging of stress fractures. Clin Sports Med 2006; 25: 53–62.
Giladi M, Nili E, Ziv Y, Danon YL, Aharonson Z. Comparison between radiography, bone scan, and ultrasound in the diagnosis of stress fractures. Mil Med 1984; 149: 459–461.
Greaney RB, Gerber FH, Laughlin RL, et al. Distribution and natural history of stress fractures in U.S. Marine recruits. Radiology 1983; 146: 339–346.
Prather JL, Nusynowitz ML, Snowdy HA, Hughes AD, McCartney WH, Bagg RJ. Scintigraphic findings in stress fractures. J Bone Joint Surg Am 1977; 59: 869–874.
Zwas ST, Elkanovitch R, Frank G. Interpretation and classification of bone scintigraphic findings in stress fractures. J Nucl Med 1987; 28: 452–457.
Amman W, Matheson GO. Radionuclide bone imaging in the detection of stress fractures. Clin J Sports Med 1991; 1: 115–122.
Kiuru MJ, Pihlajamaki HK, Ahovuo JA. Bone stress injuries. Acta Radiol 2004; 45: 317–326.
Gaeta M, Minutoli F, Scribano E, et al. CT and MR imaging findings in athletes with early tibial stress injuries: comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology 2005; 235: 553–561.
Milgrom C, Chisin R, Giladi M, et al. Negative bone scans in impending tibial stress fractures. A report of three cases. Am J Sports Med 1984; 12: 488–491.
Sterling JC, Webb RF Jr, Meyers MC, Calvo RD. False negative bone scan in a female runner. Med Sci Sports Exerc 1993; 25: 179–185.
Ahovuo JA, Kiuru MJ, Kinnunen JJ, Haapamaki V, Pihlajamaki HK. MR imaging of fatigue stress injuries to bones: intra-and interobserver agreement. Magn Reson Imaging 2002; 20: 401–406.
Aoki Y, Yasuda K, Tohyama H, Ito H, Minami A. Magnetic resonance imaging in stress fractures and shin splints. Clin Orthop Relat Res 2004; 421: 260–267.
Lee JK, Yao L. Stress fractures: MR imaging. Radiology 1988; 169: 217–220.
Stafford SA, Rosenthal DI, Gebhardt MC, Brady TJ, Scott JA. MRI in stress fracture. AJR Am J Roentgenol 1986; 147: 553–556.
Yao L, Johnson C, Gentili A, Lee JK, Seeger LL. Stress injuries of bone: analysis of MR imaging staging criteria. Acad Radiol 1998; 5: 34–40.
Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners. Correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med 1995; 23: 472–481.
Ballinger PW, Frank ED. In: Merrill’s atlas of radiographic positions and radiologic procedures, 9th edn. Philadelphia: Mosby, 1999; 285–287.
Jones BH, Harris JM, Vinh TN, Rubin C. Exercise-induced stress fractures and stress reactions of bone: epidemiology, etiology, and classification. Exerc Sport Sci Rev 1989; 17: 379–322.
Burr DB, Martin RB, Schaffler MB, Radin EL. Bone remodeling in response to in vivo fatigue microdamage. J Biomech 1985; 18: 189–200.
Churches AE, Howlett CR. Functional adaptation of bone in response to sinusoidally varying controlled compressive loading of the ovine metacarpus. Clin Orthop Relat Res 1982; 168: 265–280.
Johnson LC, Stradford HT, Geis RW, Dineen JR, Kerley E. Histiogenesis of stress fractures [abstract]. J Bone Joint Surg Am 1963; 45: 1542.
Li GP, Zhang SD, Chen G, Chen H, Wang AM. Radiographic and histologic analyses of stress fracture in rabbit tibias. Am J Sports Med 1985; 13: 285–294.
Uhthoff HK, Jaworski ZF. Periosteal stress-induced reactions resembling stress fractures. A radiologic and histologic study in dogs. Clin Orthop Relat Res 1985; 199: 284–291.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kijowski, R., Choi, J., Mukharjee, R. et al. Significance of radiographic abnormalities in patients with tibial stress injuries: correlation with magnetic resonance imaging. Skeletal Radiol 36, 633–640 (2007). https://doi.org/10.1007/s00256-006-0272-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-006-0272-4