Abstract
Purpose
We have noted apparent far lateral meniscal attachment of the meniscofemoral ligament (MFL) with an anterior cruciate ligament (ACL) tear. This study evaluates MFL attachment and association with posterior horn lateral meniscus (PHLM) tear.
Materials and methods
Nine months of knee arthroscopy reports were reviewed to classify the PHLM and ACL as torn or normal. After excluding those with prior knee surgery, MR images were reviewed by two radiologists to determine the number of images lateral to PCL, which showed the ligaments of Humphrey and Wrisberg visible as structures separate from the PHLM. Any patient with abnormal PHLM surface signal not continuous with the MFL was excluded. MRI findings were compared with arthroscopy using Student’s t test and Fisher’s exact test.
Results
Of the 54 participants, 5 had PHLM tears and 49 were normal. Twenty-one had ACL tears; all those with an PHLM tear had an ACL tear. The ligament of Humphrey inserted on average 0.9 consecutive images lateral to the PCL without an PHLM tear and 4.7 with an PHLM tear; the ligament of Wrisberg inserted on average 3.0 consecutive images without an PHLM tear and 4.5 with an PHLM tear (slice thickness/gap = 3 mm/0.5 mm). There was a significant association between PHLM tear and number of images (p = 0.0028), and between ACL tear and this type of PHLM tear (p = 0.0064).
Conclusion
Apparent far lateral meniscal extension of a meniscofemoral ligament (greater than or equal to four images lateral to the PCL) should be considered as a possible PHLM tear, especially in the setting of an ACL tear.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance imaging (MRI) has become widely accepted as a sensitive and specific standard in evaluation for meniscal injury, with greater than 90% accuracy for some meniscal tears [1, 2]. Both orthopedic and radiology literature have reported a significant association between lateral meniscus tears and anterior cruciate ligament (ACL) injury, and that ACL injuries are more commonly associated with lateral meniscus tears than medial meniscus tears [3].
However, it has also been noted that the sensitivity of MRI is decreased in the setting of an ACL injury, in particular the sensitivity of diagnosing posterior horn lateral meniscus tears is significantly decreased [1]. Hypothesized explanations for the relative insensitivity of MRI with these injuries include different biomechanical stresses involved in ACL injuries, anatomy of the lateral meniscus, artifact, and its close anatomical relationship with the meniscofemoral ligament (MFL) [1, 2, 4]. In fact, the MFL has been described as causing a “pseudotear” in the posterior aspect of the lateral meniscus [5].
In our clinical practice, we have noted apparent far lateral meniscal attachment of the meniscofemoral ligament in the setting of patients with ACL tears, and hypothesized this to represent a type of meniscal tear (Fig. 1). This retrospective study was performed to evaluate MFL attachment and its possible association with PHLM tears.
Illustration of disarticulated knee with femur removed looking down on menisci shows a longitudinal tear of the posterior horn of the lateral meniscus (arrow), which extends to the attachment of the meniscofemoral ligament (black arrowheads). F fibula, P posterior cruciate ligament, A anterior cruciate ligament
Materials and methods
After receiving IRB approval with informed consent waived, the medical records of 209 patients who underwent knee arthroscopy from four Orthopaedic Surgery faculties from January 2004 to September 2004 were retrospectively reviewed (excluding March 2004, which was inadvertently omitted). Of these 209 patients, 132 were found to have a prior available MRI examination of the knee.
Of the 132 patients with prior MRI, the following were required to be included in the study: the PHLM and ACL were evaluated at arthroscopy and described as normal or torn, and the patient did not have prior meniscal or ACL surgery. This resulted in 95 patients being included. Two fellowship-trained musculoskeletal radiologists (with 10 and 12 years of experience respectively) reviewed the 95 sagittal spin-echo intermediate-weighted MRI sequences (TE/TR = 14/1,000, slice thickness/gap = 3 mm/0.5 mm, 1.5 Tesla magnet, Model Signa; GE Medical Systems, Milwaukee, WI, USA).
The presence or absence of the meniscofemoral ligament (Humphrey and/or Wrisberg) was recorded for each participant, as well as the number of MR images lateral to the posterior cruciate ligament (PCL) where the MFL was identified as a structure separate from the posterior horn of the lateral meniscus. The first MR image lateral to the PCL where the PCL was not visualized was regarded as image number one, with subsequent lateral images numbered sequentially. The MFL ligaments of Humphrey and Wrisberg were identified as elongated linear low signal structures extending from the medial femoral condyle to the posterior horn of the lateral meniscus, either anterior or posterior to the PCL respectively. A value of zero was given if the MFL was observed to have attached to the lateral meniscus on the image immediately lateral to the PCL, without the presence of a high signal cleft in between the MFL and PHLM. Reviewers were blinded to the arthroscopic findings; although the ACL was not assessed at MRI, this structure was not masked at retrospective review.
Of these 95, participants were excluded if no MFL was present (2 participants), if the MR images were of suboptimal quality (3 participants), or if there was additional signal abnormality involving the superior or inferior articular surface of the PHLM not continuous with an MFL (36 participants). This latter exclusion criterion was applied so that retrospective arthroscopic results could directly correlate with the MRI findings at the PHLM and MFL. Our goal was to evaluate only those meniscal tears that involved the attachment of the MFL. After applying these exclusion criteria, the final study group consisted of 54 participants.
The number of images where either the MFL of Humphrey or Wrisberg was identified as a structure separate from the PHLM was correlated with the presence or absence of an PHLM and ACL tear at arthroscopy to determine significance using Fisher’s exact test. Other variables were compared using the Student’s t test.
Results
The 54 participants consisted of 43 men and 11 women with an average age of 39 years (range 17–71 years). The average time interval between MRI and arthroscopy was 107 days (range 3–1,106 days); the two participants with a time interval greater than 180 days did not have an PHLM tear. Of the 54 subjects, 9% (5 out of 54) had a tear of the PHLM and 91% (49 out of 54) had a normal PHLM at arthroscopy. In addition, 40% (21 out of 54) were found to have an ACL tear, 5 of whom also had an PHLM tear. Of the 60% (33 out of 54) without an ACL tear, the PHLM was normal at arthroscopy. A significant association was found between PHLM and ACL tears (p = 0.0064), as all 5 patients with an PHLM had an ACL tear. There was a significant difference in age between those with ACL injury (average 28 years) and those without (average 46 years; p < 0.0001).
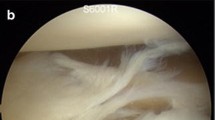
On MRI, a distinct MFL was identified as a ligament of Humphrey in 50% (27 out of 54 patients), ligament of Wrisberg in 28% (15 out of 54 patients), or both in 22% (12 out of 54 patients). In those 49 patients without an PHLM tear, the ligament of Humphrey inserted on average 0.9 consecutive images (range 0–3) lateral to the PCL. In contrast, the ligament of Humphrey inserted an average of 4.7 consecutive images (range 0–8) in patients with an PHLM tear (Fig. 2). The ligament of Wrisberg inserted on average 3.0 consecutive images (range 1–5) lateral to the PCL in patients without an PHLM tear, and 4.5 consecutive images (range 4–5) in patients with an PHLM tear (Fig. 3). There was a significant association between PHLM tears and the number of consecutive images on which the MFL is visualized lateral to the PCL (p = 0.0028).
A 37-year-old man with posterior horn lateral meniscus (PHLM) and anterior cruciate ligament (ACL) tears at arthroscopy. Sagittal spin-echo intermediate-weighted MR image (TE/TR = 14/1,000, slice thickness/gap = 3 mm/0.5 mm) six images lateral to PCL shows abnormal increased signal (arrow), which extends to the superior surface of the PHLM. Low signal area (arrowhead) was continuous with the ligament of Humphrey
A 17-year-old man with PHLM and ACL tears at arthroscopy. Sagittal spin-echo intermediate-weighted MR image (TE/TR = 14/1,000, slice thickness/gap = 3 mm/0.5 mm) five images lateral to the PCL shows abnormal vertical increased signal (arrow), which extends to the superior surface of the PHLM. Low signal area (arrowhead) was continuous with the ligament of Wrisberg. Note low signal bone marrow edema of the lateral femoral condyle and posterior tibia
When comparing the patients with and without ACL tear (Table 1), the ligament of Humphrey inserted on average 0.8 and 1.0 images lateral to the PCL respectively in the absence of an PHLM tear. The ligament of Wrisberg inserted on average 3.1 and 3.0 images respectively in those with and without ACL tears in the absence of an PHLM tear.
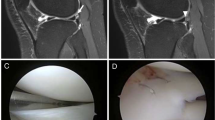
Using a threshold of four or more images lateral to the PCL where the MFL was identified as a structure distinct from the meniscus resulted in a sensitivity of 80% (4 out of 5), specificity of 82% (40 out of 49), positive predictive value of 31% (4 out of 13), and negative predictive value of 98% (40 out of 41) for the diagnosis of PHLM tear (p = 0.0097). Of the 5 patients with PHLM tear, 4 had the MFL (Wrisberg and/or Humphrey) visualized on four or more consecutive images lateral to the PCL, and 1 patient had less than four images. Of the patients without PHLM tear, 9 demonstrated the MFL inserting on four or more consecutive images (Fig. 4), and 40 with less than four images.
A 21-year-old man with an ACL tear and a normal PHLM at arthroscopy. Sagittal spin-echo intermediate-weighted MR image (TE/TR = 14/1,000, slice thickness/gap = 3 mm/0.5 mm) five images lateral to the PCL shows an abnormal vertical increased signal (arrow), which extends to the superior surface of the PHLM. Low signal area (arrowhead) was continuous with the ligament of Wrisberg
Discussion
Our results demonstrate a significant association between apparent far lateral meniscal attachment of the MFL and PHLM tear (visualized at four or more consecutive sagittal MR images lateral to the PCL with a 3-mm slice thickness and a 0.5-mm slice gap). Each patient with this type of PHLM tear also had an ACL tear. Conversely, in patients without PHLM tears, the MFL inserted on average less than four continuous images lateral to the PCL.
The MFL is a strong fibrous structure that extends inferiorly and laterally from the medial femoral condyle to insert into the PHLM. When coursing anteriorly to the PCL, it is called the ligament of Humphrey, while posterior to the PCL it is called the ligament of Wrisberg. The MFL has a reported incidence of 70–100%, with the ligament of Humphrey seen in 26–50%, an isolated ligament of Wrisberg in 35–76%, and both present in 6–17% [6]. The function of the MFL is to stabilize the PHLM [7, 8].
With regard to the MRI appearance of the MFL, Vahey et al. [5] reported in a series of 42 patients with normal arthroscopy that the MFL inserted within three consecutive images, possibly simulating a meniscal tear. However, the significance of MFL insertion beyond three consecutive images was not addressed. Our findings may be one explanation for inaccuracies in the diagnosis of an PHLM tear, particularly in the setting of ACL injury. While it is understood that the attachment of the MFL may simulate a meniscal tear, theoretically the PHLM tear that extends into the attachment between the MFL and PHLM as shown in our study may be misinterpreted as a normal variant of the MFL attachment. Our results support our hypothesis that apparent far lateral meniscal attachment (four or more images lateral to the PCL) represents a type of longitudinal meniscal tear associated with ACL injury (Fig. 1).
The association between ACL tears and PHLM is well documented in the literature, with a longitudinal tear being most common [1–3, 6]. It has been proposed that the relative increased mobility of the lateral meniscus makes it more susceptible to shear or compressive injury related to twisting injury associated with ACL tears [9]. Bone marrow edema patterns associated with ACL tears commonly involve the posterior and lateral tibia, which suggests a direct compressive force between the tibia and femur on the meniscus and may partly be the causative factor. It is also possible that the PHLM tears associated with an ACL tear in our patients are caused by anterior tibial translation at the time of the ACL injury, which may pull the meniscus forward, stripping the MFL away from the meniscus to create an PHLM tear. While previous investigations indicated that there was no association between the presence or absence of an MFL and a lateral meniscal tear [7], none our participants with both ligaments of Humphrey and Wrisberg (n = 12) had this type of MFL-stripping tear of the PHLM tear, even in the presence of an ACL tear.
Our data indicate a significant association between apparent far lateral meniscal attachment of the MFL and PHLM tear, with a threshold determined to be four or more images lateral to the PCL. However, in one patient with an PHLM tear at arthroscopy, the MFL attached immediately to the PHLM. Retrospective review of this case (not shown) revealed an abnormal superior popliteomeniscal fascicle, which is an indirect sign of an PHLM tear [4, 10]. Because only sagittal spin-echo intermediate-weighted sequences were used in this study to characterize an abnormal meniscal signal separate from the MFL, this finding was overlooked and was better appreciated on the retrospective review of the fast spin-echo intermediate-weighted fat saturation sequences. With regard to those patients without an PHLM tear, the ligament of Humphrey always inserted less than four images lateral to the PCL (Table 1). However, in the 25 patients with a ligament of Wrisberg, 96% (24 out of 25) showed attachment equal to or less than four images and 4% (1 out of 25) had an attachment that was seen on five images. It is possible that this represents a variation in the MFL attachment to the PHLM, or perhaps the PHLM was overlooked at arthroscopy or healed (the time interval in this case was 73 days; Fig. 4). The small sample size precluded evaluation of the ligaments of Humphrey and Wrisberg independent from each other.
We acknowledge several limitations to this study, which includes a small number of patients with an PHLM tear; however, this was due to our exclusion criteria, which ensured that the arthroscopic abnormality directly correlated with the findings on MRI in the region of the MFL. Another limitation is the retrospective nature of this study. Selection bias is likely introduced as patients with more significant injury or symptoms are more likely to receive medical care. Another limitation is the retrospective MRI interpretation by consensus; therefore, interobserver variability was not assessed. Lastly, four orthopaedic surgeons participated in this study, which could add variability to the diagnosis of PHLM tears.
In conclusion, apparent far lateral meniscal attachment of the MFL to the PHLM (equal to or greater than four consecutive MR images lateral to PCL) may represent a type of meniscal tear associated with ACL injury. Knowledge of this type of tear may help to improve accuracy in the diagnosis of PHLM tears.
References
De Smet AA, Graf BK. Meniscal tears missed on MR imaging. AJR Am J Roentgenol 1994;162:905–11.
Jee WH, McCauley TR, Thomas R, Kim JM. Magnetic resonance diagnosis of meniscal tears in patients with acute anterior cruciate ligament tears. J Comput Assist Tomogr 2004;28:402–6.
Nikolic DK. Lateral meniscal tears and their evolution in acute injuries of the anterior cruciate ligament of the knee. Knee Surg Sports Traumatol Arthrosc 1998;6:26–30.
De Smet AA, Asinger DA, Johnson RL. Abnormal superior popliteomeniscal fascicle and posterior pericapsular edema: indirect MR imaging signs of a lateral meniscus tear. AJR Am J Roentgenol 2001;176:63–6.
Vahey TN, Bennett HT, Arrington LE, Shelbourne KD, Ng J. MR imaging of the knee: pseudotear of the lateral meniscus caused by the meniscofemoral ligament. AJR Am J Roentgenol 1990;154:1237–9.
Poynton AR, Javadpour SM, Finegan PJ, O’Brien M. The meniscofemoral ligaments of the knee. J Bone Joint Surg Br 1997;79:327–30.
Lee BY, Jee WH, Kim JM, Kim BS, Choi KH. Incidence and significance of demonstrating the meniscofemoral ligament on MRI. Br J Radiol 2000;73:271–4.
Gupte CM, Smith A, McDermott D, Bull AMJ, Thomas RD, Amis A. Meniscofemoral ligaments revisited. J Bone Joint Surg Br 2002;84-B:846–51.
Smith JP, Barrett GR. Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. Am J Sports Med 2001;29:415–19.
Blankenbaker DG, De Smet AA, Smith JD. Usefulness of two indirect MR imaging signs to diagnose lateral meniscus tears. AJR Am J Roentgenol 2002;178:579–82.
Acknowledgement
Figure 1 illustration by Anna Browning.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, L.S., Jacobson, J.A., Jamadar, D.A. et al. Posterior horn lateral meniscal tears simulating meniscofemoral ligament attachment in the setting of ACL tear: MRI findings. Skeletal Radiol 36, 399–403 (2007). https://doi.org/10.1007/s00256-006-0257-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-006-0257-3