Abstract
Objective
To describe the MR imaging findings of acute and chronic rectus femoris origin (RFO) injuries.
Materials and methods
A retrospective review of pelvic and hip MR imaging procedures was performed over a 4-year period for detection of cases with injuries to the RFO. Subjects were classified as having either acute or chronic symptoms. MR imaging studies, radiographs, CT scans, radiology reports, medical records, and operative notes were reviewed. Imaging analysis was directed to assess injuries affecting the direct and indirect heads of the RFO. Concurrent osseous, cartilaginous and musculotendinous injuries were tabulated.
Results
The incidence of RFO injuries on MR imaging was 0.5% (17/3160). With the exception of one case of anterior inferior iliac spine apophysis avulsion and partial tear of the direct head of RFO, all subjects had indirect head of RFO injuries (acute injury 8/9, chronic injury 8/8). Partial tear of the direct head of RFO was less frequently seen (acute injury 3/9, chronic injury 2/8). Partial tears of the conjoint tendon were least frequent (acute 1/9, chronic 2/8). No full-thickness tears of the RFO were noted. Associated labral tears were seen in only one case, with no other concomitant abnormality of the articular cartilage or surrounding soft tissues. All RFO injuries were treated non-operatively.
Conclusion
Injuries of the RFO are uncommon on MR examinations of pelvis/hips and may occur in a sequence progressing from indirect head injury to involvement of direct head and conjoint tendon in more severe cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The rectus femoris muscle is a component of the quadriceps musculature in the anterior thigh. Proximally, the rectus femoris muscle has two discrete attachments described as the direct and indirect heads (Fig. 1). The direct head of the rectus femoris originates from the anterior inferior iliac spine just cranial to the hip joint. The indirect head also known as the reflected head, originates from the anterior-lateral aspect of the acetabulum and the hip joint capsule [1]. The two heads form a conjoined tendon around 2 cm distal to their origin.
Normal MR anatomy of the proximal right rectus femoris in a 51-year-old woman. a Axial fat-suppressed T2-weighted image from an MR arthrogram demonstrates the origin of the direct head (large arrow) from the anterior inferior iliac spine and of the indirect head (small arrow) from the superior ridge at the anterolateral aspect of the acetabulum. b Slightly caudally, the two heads converge to form the conjoined tendon, with the direct head fibers superficial (large arrow) and the indirect head fibers deep (small arrow). c, d Coronal T1-weighted images demonstrate the proximal indirect head (c, small arrow) and the direct head (d, large arrow) at their origins. Note the close proximity of the indirect head to the joint capsule, which is distended with intra-articular contrast medium. (IP iliopsoas muscle, R rectus femoris muscle, SA superior)
The rectus femoris is the most commonly injured muscle of the quadriceps muscle group [2]. Myotendinous strain injuries to the rectus femoris muscle are common and have been previously described [2–6]. Limited reports are available on magnetic resonance (MR) imaging of injuries affecting the direct head of RFO [1, 2, 7], and no study describes the MR imaging features of injuries affecting the indirect head of RFO. To our knowledge, the present study is the first to specifically evaluate the MR imaging appearance of injuries affecting the direct and indirect heads of RFO. In this article, we report our experience with imaging of acute and chronic RFO injuries in a retrospective analysis of MR imaging studies of pelvis and hip performed at our institution.
Materials and methods
This study was approved by the Institutional Review Board with exemption status for individual informed consent. A retrospective search was performed using Boolean operators [8] in reports generated for 3,160 consecutive cases of pelvis and hip MR imaging studies obtained at our institution from 2002 to 2005. Of these examinations, 13% were MR arthrographic studies (410/3,160). The reports were searched with a standard keyword subroutine (Folio, Camberly Systems, Cambridge, MA) for the words “rectus” and “femoris”. Imaging studies and reports, medical records and operative notes were reviewed in all cases.
Subjects were clinically classified as either having acute or chronic hip pain. Previously asymptomatic subjects who experienced sudden hip pain at a definable moment were classified as acute injuries. All other patients, including those with longstanding hip pain, were classified as chronic injuries. For subjects with acute injuries, the time interval between acute event and MR imaging was tabulated.
MR imaging of pelvis and hip was performed on 1.5-T scanners (Signa LX, GE Medical Systems, Milwaukee, WI; and Sonata, Siemens Medical Systems, Erlangen, Germany), employing routine imaging protocols that included sagittal fat-suppressed proton density [repetition time (TR) 2850 ms, time to echo (TE) 20 ms, number of excitations (NEX) 2, matrix192×390, slice thickness 4 mm, field of view (FOV) 36 cm], coronal short-tau inversion recovery (STIR) (TR 4000 ms, TE 48 ms, NEX 2, matrix 192×320, slice thickness 4 mm, FOV 36 cm), coronal T1-weighted (TR 400 ms, TE 12 ms, NEX 2, matrix 192×384, slice thickness 4 mm, FOV 36 cm), axial proton density (TR 2500 ms, TE 17 ms, NEX 2, matrix 192×512, slice thickness 3 mm, FOV 36 cm) and axial fat-suppressed T2-weighted (TR 3500 ms, TE 50 ms, NEX 2, matrix 192×320, slice thickness 3 mm, FOV 36 cm) pulse sequences. Imaging protocols for MR arthrography included coronal T1 (TR 700 ms, TE 12 ms, NEX 3, matrix 192×320, slice thickness 4 mm, FOV 16 cm), coronal and sagittal fat-saturated T1-weighted (TR 700 ms, TE 12 ms, NEX 3, matrix 192×384, slice thickness 4 mm, FOV 16 cm), axial proton density (TR 1900 ms, TE 25 ms, NEX 4, matrix 192×384, slice thickness 4 mm, FOV 16 cm) and axial fat-suppressed T2-weighted (TR 5000 ms, TE 50 ms, NEX 3, matrix 192×384, slice thickness 4 mm, FOV 16 cm) pulse sequences. MR arthrographic images were obtained after intra-articular administration of approximately 10 ml of contrast material solution. The solution was made by mixing 50 ml of normal saline with 0.4 ml of gadopentetate dimeglumine (Magnevist, Berlex, Montville, NJ). Ten milliliters of this solution was then mixed with 5 ml of 61% iopamidol (Isovue-M 300, Bracco Diagnostics, Princeton, NJ) and 5 ml of 1% lidocaine. CT scan imaging was performed of GE Lightspeed 16 slice platforms using standard departmental protocol (FOV 16 cm, slice thickness 2.5 mm, image spacing 2.5 mm, pitch 0.938, KVP 140, auto MA, bone algorithm).
MR imaging interpretation of subjects with RFO injury was performed in consensus by two experienced musculoskeletal radiologists (H.O., M.T.). The MR imaging criterion for complete tear of RFO was non-visualization of tendinous structure or presence of full-thickness discontinuity with fluid signal intensity (SI) on T2-weighted images. The criterion for partial tear detection was fluid-like hyperintense SI partially disrupting the tendon on T2-weighted images (Fig. 2). On MR arthrography, identifying intra-articular contrast material partially (partial tear) or completely (complete tear) transecting the indirect head of RFO was used as additional criterion (Fig. 3). The criterion for RFO strain was increased SI (lower than fluid SI) on T2-weighted imaging without tendon disruption. MR imaging criteria for avulsion fracture included hypointense linear abnormality on T1-weighted imaging in bone underlying RFO, and visualization of osseous fragment and donor site (Fig. 4). MR imaging criteria for chronic injury included wavy appearance and thickening of a tendon (Fig. 5). Detection of mineralization in a tendon visualized as globular hypointense area on both T1- and T2-weighted MR images was also used as criterion for chronic injury (Fig. 6). Twelve radiographs and three CT scans were available and analyzed for the presence of heterotopic ossification at the RFO.
A 35-year-old man with acute partial tears of the indirect head, direct head, and confluence of the proximal rectus femoris. a Axial fat-suppressed T2-weighted image demonstrates attenuation of the indirect head at its origin with surrounding fluid (large arrow). There is thickening and increased signal within the direct head (small arrow). b Axial fat-suppressed T2-weighted image shows thickening and increased signal at the confluence of the indirect and direct heads (arrow) with adjacent edema. c Coronal inversion recovery image at the level of the anterior inferior iliac spine shows thickening and intrinsic signal abnormality of the proximal direct head (arrow)
A 28-year-old man with acute partial-thickness tear of the indirect head of the left rectus femoris at its origin from the anterolateral aspect of the acetabulum and the superolateral joint capsule. a Axial fat-suppressed T2-weighted image from an MR arthrogram demonstrates partial disruption of the tendon with T2 hyperintensity and enlargement (arrow). b Coronal fat-suppressed T1-weighted image shows extension of intra-articular gadolinium into the partially torn indirect head (arrow)
A 14-year-old boy with acute avulsion of the apophysis of the left anterior inferior iliac spine. a Coronal T1-weighted image shows an avulsed fragment of the apophysis (arrow) with hypointense hematoma interposed between the fragment and the adjacent bone. b Axial fat-suppressed T2-weighted image demonstrates large hematoma (arrow) in the expected location of the proximal direct head of the rectus femoris
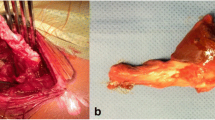
A 49-year-old man with chronic rectus femoris rupture. a Anteroposterior radiograph of the right hip demonstrates ossification throughout the length of the proximal rectus femoris tendon (arrows). b–d Axial proton density-weighted (b, c) and fat-suppressed T2-weighted (d) images show full-thickness tear of the proximal tendon with heterotopic ossification expanding the tendon sheath visualized as heterogeneous hypointense signal (arrows)
Data on population age, gender, history, injury location and grade of injury were tabulated. Injuries to the indirect and direct heads of RFO were analyzed. Injuries involving the junction of direct and indirect heads were also recorded. MR imaging data on associated injuries including bone contusions, acetabular labral tear, hip articular cartilage defect and other musculotendinous injuries were acquired.
Results
Seventeen subjects were found to have RFO injuries. The incidence of RFO injury on MR imaging in our series was 0.5% (17/3,160). The average age of the subjects was 47 years (range 14–78 years) at the time of MR imaging. Seven patients were female and 10 were male. Fifty-three percent (9/17) had an acute injury. There were eight injuries involving the right RFO and nine involving the left. No subject had documented bilateral RFO injuries. Most subjects had an injury to the indirect head of the RFO (94%, 16/17) predominantly representing partial tears (75%, 12/16). Five subjects had a partial tear of the direct head of the RFO (29%, 5/17). No full-thickness tears of the RFO were noted.
Nine subjects met our clinical criteria for acute injury (Table 1). The average age of patients with acute injury was 47 years (range 14–76 years). Six subjects were male and three were female. The average time from injury to MR imaging was 17 days (range 1–58 days). There was clinical suspicion of injury to the direct head of RFO in two cases. The finding of indirect head of RFO injury was clinically unsuspected in all cases. Eighty-nine percent of acutely injured patients (8/9) had an injury to the indirect head of the RFO. The only acutely injured patient with an intact indirect head had an avulsion of the anterior inferior iliac spine and partial tear of the direct head of RFO. Two other acutely injured patients also had partial tears of the direct head of the RFO. Two patients had mineralization of RFO seen only on radiographs. One subject had mineralization of RFO on both radiographs and CT scans. Despite presenting with acute symptoms, two subjects showed MR imaging findings suggesting chronic injury of RFO (Table 1).
Eight subjects had chronic hip pain (Table 2). The average age in this category was 53 years (range 16–78 years). Four subjects were male and four female. All patients in this category had injuries to the indirect head of the RFO. Two patients with chronic symptoms also had injuries to the direct head and conjoint tendon. Two patients had mineralization of RFO on radiographs.
Two cases of RFO injuries were diagnosed on MR hip arthrogram. In both instances, intra-articular gadolinium leakage was visualized partially extending through the indirect head of RFO, suggesting partial tear of the indirect head and associated superior capsular injury. Labral tears were noted in only one case with no other concomitant abnormality of the articular cartilage or surrounding soft tissues. All RFO injuries were treated non-operatively.
Discussion
The rectus femoris is the most frequently injured muscle of the quadriceps group. The rectus femoris is particularly susceptible to injuries because it spans two joints (hip and knee) [1], with injuries being particularly common in kicking sports such as soccer [2].
The biomechanics of kicking has been well described [9]. In the final portion of the backswing phase, the hip is hyperextended and the knee is flexed, leading to stretching of the quadriceps muscle. At the onset of the forward swing, there is massive eccentric muscular recruitment of the quadriceps and iliopsoas muscles. Forceful muscular contraction in a stretched quadriceps muscle may lead to sprain and tear, affecting most likely the rectus femoris due to its bi-articular span [4, 9]. In our study, one subject with partial tear of the indirect head of the RFO experienced sudden hip pain during a tae-kwon-do kicking exercise. A second subject with avulsion of the anterior inferior iliac spine experienced sudden pain when kicking during soccer practice.
Although injuries to the rectus femoris muscle and myotendinous junction are common, injuries to the RFO are unusual [1]. In our study, the incidence of RFO injury seen on pelvis and hip/hip arthrogram MR imaging was 0.5% (17/3160).
Injuries to the direct head of RFO are thought to be more common than injuries to the indirect head of RFO [2]. However, this is based on case reports using radiographs and CT scans to demonstrate avulsion fractures [7, 10]. Furthermore, very few reports are available on MR imaging of injuries affecting the direct head of RFO. A prior report demonstrated a case of high SI on T1-weighted imaging at the direct head of RFO, suggesting a full-thickness tear with mild retraction [1]. Another report demonstrated MR imaging features of avulsion fracture of the antero-inferior iliac spine at the direct head origin [2]. No study describes the magnetic resonance (MR) imaging features of injuries affecting the indirect head of the RFO.
Our data are in contrast with those of prior studies using radiographs and CT in which injuries to the direct head were more frequent and thought likely to occur in isolation without indirect head injury [2, 7, 10]. In cases of acute injury, the indirect head of RFO was injured in almost all subjects (8/9). The only patient with an intact indirect head of RFO was a soccer player with avulsion of the anterior inferior iliac spine apophysis and partial tear of the direct head of RFO. One patient had partial tear of both the indirect and direct heads of RFO without injury to the conjoint tendon. One patient had a partial tear of the indirect head, direct head and conjoint tendon. Although avulsion fractures may occur at the direct head origin and can be identified on radiographs or CT [7, 10], this discrepancy could be partially explained by the improved sensitivity of MR imaging of soft tissue injuries, enabling better overall assessment of the RFO. In fact, our data presented in Table 1 suggest a progression of acute injury, starting with the indirect head of RFO, progressing to the direct head and eventually affecting the conjoint tendon in more severe cases.
Of the nine patients who met our clinical criterion for acute injury, three had mineralization at the expected location of the RFO (Table 1). The discordance between the acuity of clinical symptoms and the imaging findings of chronicity in three of the patients in this group requires further elucidation. Subject 1 had mineralization at the RFO and met our MR imaging criterion for chronic injury. We suspect that this subject had prior injury to the indirect head of RFO, which may not have been injured acutely and not have been the source of acute pain. Subject 8 had mineralization at the RFO, but met the MR imaging criterion for acute tears of the indirect head, direct head and conjoint tendon. We suspect that this patient had an acute injury superimposed on a chronic injury of RFO. Lastly, subject 9 had mineralization at the RFO likely because imaging was performed 32 days after initial injury. Subject 9 met the MR imaging criteria for old injury because of the presence of low-intensity mineralization in the RFO.
In the category of subjects with chronic symptoms, all patients had injury to the indirect head of RFO (8/8). Two subjects also had injury to the direct head and conjoint tendon. Our data in the chronic injury population further supports the concept that RFO injuries occur at the indirect head first and progress to involve the direct head and eventually the conjoint tendon of the RFO in more severe cases.
No patients had avulsion fractures at the attachment site of the indirect head. The indirect head of the RFO originates both from the anterior lateral aspect of the acetabulum and the hip joint capsule. Of interest, two cases with partial tear of indirect head of RFO were seen on MR arthrography (2/17). In both cases, intra-articular gadolinium leakage was visualized partially transecting the indirect head of RFO, suggesting associated superior capsular injury. Because of its capsular attachment, it is possible that there is a high association between indirect head of RFO tears and superior capsular rupture.
RFO injuries are likely to be missed on radiographs unless there is heterotopic bone formation suggesting chronic injury, or an avulsion fracture has occurred [1]. In our study, 12 of the 17 subjects (71%) had radiographs of the hip, and 5 of these 12 (42%) showed mineralization in the expected location of the RFO consistent with chronic injury. The remaining 7 subjects (58%) showed no evidence of injury to the RFO. CT scan correlation was available in a limited subset of patients (3/17, 18%), of which only one case of chronic injury was detected. These findings underscore the importance of MR imaging in detecting RFO injuries in the acute setting.
Most patients with RFO injuries are treated conservatively. In cases of antero-inferior iliac spine apophysis avulsion, a short period of bed rest followed by a period of progressive weight bearing with crutches is recommended [11]. In some cases in which conservative treatment is not successful, operative treatment such as reattachment surgery can be performed [12]. In our study, all subjects were treated non-operatively.
One limitation of our study was the small sample size. Only 17 subjects with MR imaging of RFO injuries were available. Only 12 subjects had radiographs and 3 had CT correlation. Another limitation was the retrospective nature of this study, which could affect our reported incidence, as a few positive cases may have been undiagnosed. Furthermore, our incidence refers to detection of RFO pathology in patients undergoing MR imaging of pelvis and hip and hip arthrography, which may not reflect the true incidence of this injury in elite or competitive athletes. The activities that produced acute symptoms are tabulated in Table 1. Amongst those in the chronically symptomatic group, there were no elite/or competitive athletes. Lastly, surgical confirmation for injury of RFO, labral tear or cartilage abnormalities could not be obtained.
In conclusion, injuries affecting the RFO are uncommon in MR examinations of pelvis and hips in a general population. Our study suggests a progression of acute injury affecting the indirect head of RFO first, progressing to the direct head and eventually the conjoint tendon in more severe cases.
References
Hsu JC, Fischer DA, Wright RW. Proximal rectus femoris avulsions in national football league kickers: a report of 2 cases. Am J Sports Med 2005;33:1085–7
Bordalo-Rodrigues M, Rosenberg ZS. MR imaging of the proximal rectus femoris musculotendinous unit. Magn Reson Imaging Clin North Am 2005;13:717–25, vii
Temple HT, Kuklo TR, Sweet DE, Gibbons CL, Murphey MD. Rectus femoris muscle tear appearing as a pseudotumor. Am J Sports Med 1998;26:544–8
Hasselman CT, Best TM, Hughes Ct, Martinez S, Garrett WE, Jr. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med 1995;23:493–9
Cross TM, Gibbs N, Houang MT, Cameron M. Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. Am J Sports Med 2004;32:710–9
Rask MR, Lattig GJ. Traumatic fibrosis of the rectus femoris muscle. Report of five cases and treatment. JAMA 1972;221:268–9
Deehan DJ, Beattie TF, Knight D, Jongschaap H. Avulsion fracture of the straight and reflected heads of rectus femoris. Arch Emerg Med 1992;9:310–3
Thomas BJ, Ouellette H, Halpern EF, Rosenthal DI. Automated computer-assisted categorization of radiology reports. AJR Am J Roentgenol 2005;184:687–90
Gainor BJ, Piotrowski G, Puhl JJ, Allen WC. The kick: biomechanics and collision injury. Am J Sports Med 1978;6:185–193
Nanka O, Havranek P, Pesl T, Dutka J. Avulsion fracture of the pelvis: separation of the secondary ossification center in the superior margin of the acetabulum. Clin Anat 2003;16:458–60
Mader TJ. Avulsion of the rectus femoris tendon: an unusual type of pelvic fracture. Pediatr Emerg Care 1990;6:198–9
Straw R, Colclough K, Geutjens G. Surgical repair of a chronic rupture of the rectus femoris muscle at the proximal musculotendinous junction in a soccer player. Br J Sports Med 2003;37:182–4
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ouellette, H., Thomas, B.J., Nelson, E. et al. MR imaging of rectus femoris origin injuries. Skeletal Radiol 35, 665–672 (2006). https://doi.org/10.1007/s00256-006-0162-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-006-0162-9