Abstract
Objective
The purpose of this study was to highlight the critical role that MRI may play in diagnosing unsuspected lower extremity deep venous thrombosis and to stress the importance of scrutinizing MRI studies of the lower extremity showing apparently non-specific muscle edema for any evidence of intramuscular venous thrombosis.
Design and patients
The imaging studies of four patients in whom deep venous thrombosis was unsuspected on clinical grounds, and first diagnosed on the basis of MRI findings, were reviewed by two musculoskeletal radiologists in consensus. In all four patients the initial clinical suspicion was within the scope of musculoskeletal injuries (gastrocnemius strain, n=3; ruptured Baker cyst, n=1), explaining the choice of MRI over ultrasound as the first diagnostic modality.
Results
All patients showed marked reactive edema in the surrounding soft tissues or muscles. Three patients showed MR evidence of branching rim-enhancing structures within intramuscular plexuses characteristic of venous thrombosis (gastrocnemius, n=1; sural, n=2); one patient showed a distended popliteal vein. Ultrasound was able to duplicate the MRI findings in three patients: one patient showed above-the-knee extension on ultrasound; neither of the two patients with intramuscular thrombosis demonstrated on ultrasound showed extension to the deep venous trunks.
Conclusion
Intramuscular venous thrombosis can present as marked edema-like muscle changes on MRI, simulating primary musculoskeletal conditions. In the absence of clinical suspicion for deep venous thrombosis, only the identification of rim-enhancing branching intramuscular tubular structures will allow the correct diagnosis to be made.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In daily clinical practice deep venous thrombosis is diagnosed by Doppler ultrasound examination performed on patients with pulmonary embolism or a clinical history suspicious of deep venous thrombosis; in this setting a positive diagnosis is expected. However, patients may present with calf pain without clear predisposing factors for deep venous thrombosis, and the clinical suspicion may be directed to alternative diagnoses, often of musculoskeletal nature.
A low pre-test suspicion of deep venous thrombosis may lead to opting for an MR examination under the presumptive diagnosis of muscle strain. Compounding the initial misleading impression, reactive muscle edema-like changes may predominate on the MR imaging study and overshadow the presence of venous thrombosis.
We noticed this pattern in four patients who were sent for MR imaging due to a suspicion of a muscle strain or intraarticular derangement.
Subjects and methods
The medical records and imaging findings of four patients undergoing MR examinations with a presumptive diagnosis of musculoskeletal conditions in the knee or calf were reviewed. These cases were collected from two different institutions over the course of 2 years during routine clinical reading sessions. The group consisted of three men and one woman with ages ranging from 49 years to 80 years (mean age 52 years). Three of the patients presented with calf pain, which prompted the referring physician to obtain an MR examination of the painful calf; and the fourth patient complained of posterior knee pain and was sent for imaging with a clinical suspicion of Baker cyst. An Institutional Review Board waiver was obtained.
Two musculoskeletal radiologists retrospectively reviewed the MR imaging studies, reaching consensus as to the presence of rim-enhancing tubular branching structures corresponding to distended thrombosed veins. Ancillary MR criteria used to differentiate thrombosed from non-thrombosed vascular structures included the presence of distention, wall thickening, and high signal intensity on T1- and T2-weighted sequences.
Doppler ultrasound examinations were obtained in all cases within 2 days of the MR study.
MRI was performed on a 1.5 T unit (GE, Healthcare). Calf imaging protocols were used for three of the patients and included axial T1-weighted (TR range/TE range 500–750/10 ms); fat-suppressed, axial T2-weighted (TR range/TE eff. range 4,650–6,100/80–84 ms); sagittal T1-weighted (500–550/9 ms); sagittal short-tau inversion recovery (STIR) (TR/TE eff./TI, 5,650–6,250/52–66/160 ms); fat-suppressed coronal T2-weighted (3,100–5,050/70–90 ms).
All patients received intravenously administered contrast material and were scanned with post-contrast axial T1-weighted spin-echo, sagittal spin-echo T1-weighted, and coronal spin-echo T1-weighted sequences. A phased-array extremity coil was used in two patients.
Experienced ultrasound technologists performed the ultrasound studies, and static images were presented to the radiologist at the time of the interpretation. Compressibility was demonstrated on gray-scale axial scans; flow was documented with gray-scale and color-Doppler analysis; 7.5 MHz linear-array probes (Acuson 128 XP, Mountain View, Calif., USA) were used.
The fourth patient underwent MRI of the right knee, also performed on a 1.5 T magnet (Signa, General Electric Medical Systems) using a quadrature extremity coil. MRI protocol incorporated the following sequences: sagittal spin-echo intermediate-weighted (TR /TE 1,200/20 ms), fat-suppressed sagittal and axial T2-weighted (TR/TE eff., 5,500/65 ms), and coronal fast spin-echo intermediate-weighted (2,000/35 ms). Post-contrast scans included a fat-suppressed T1-weighted spin-echo sequence (550/15 ms).
Results
In all cases the presumptive clinical suspicion of muscle strain (n =3), or intraarticular derangement (n =1), were proven to be incorrect in view of the MRI results.
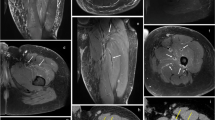
A 61-year-old man presented with a complaint of left calf pain with inability to bear weight. There was no prior significant medical history. Intramuscular medial gastrocnemius thrombosis was shown on MRI and ultrasound (Fig. 1).
A 61-year-old male patient with calf pain. There was no history of trauma. a Axial, T2-weighted, fat-suppressed scan shows diffuse edema signal in the medial gastrocnemius muscle. A central round structure corresponds to a distended clot-filled intramuscular vein (arrows). b Coronal, T2-weighted, fat-suppressed MR image shows a distended vein with increased signal intensity and wall thickening (arrows). Notice the presence of marked surrounding muscle edema. c Coronal, T1-weighted, post-contrast, MR image shows a tubular, thrombosed, venous structure with surrounding enhancement (arrows). d Gray-scale transverse ultrasound image at the level of the calf identifies a non-compressible, intramuscular, distended vein with intravascular echogenic material (asterisk)
MRI showed marked edema in the medial gastrocnemius muscle, with a central distended tubular structure showing peripheral rim enhancement (Fig. 1b,c).
On ultrasound evaluation, a diagnostic non-compressible intramuscular venous structure was demonstrated. Additionally, no residual flow could be found on color or spectral Doppler interrogation (Fig. 1d).
A 49-year-old man presented with calf pain and swelling of 2 weeks’ duration. The presumptive diagnosis was of muscle strain. However, the patient did not recall any specific traumatic accident. MRI showed a predominance of edema-like changes in the soleus muscle, overshadowing the presence of central tubular rim-enhancing intramuscular clots (Fig. 2). The results of an ultrasound performed shortly after the MRI study were reported as negative.
A 49-year-old male patient presenting with calf pain and swelling for 2 weeks and no history of trauma. a Coronal, T2-weighted, fat-suppressed image shows marked muscle edema in the soleus. b Coronal, T2-weighted, fat-suppressed image at a deeper plane shows a tubular low-intensity filling defect within a soleal intramuscular vein (arrows). c Coronal, fat-suppressed, post-contrast image shows tubular branching structures in the soleus venous plexus, with surrounding enhancement at two different levels (arrows). d,e Two axial, fat-suppressed, post-contrast images, corresponding to the segments of involvement shown on the coronal post-contrast image (c), show characteristic, branching, rim-enhancing structures (arrows)
Neither of these two patients was proven to experience proximal extension of thrombus into the main venous trunks of the calf or into the popliteal vein on follow-up examinations. There was no evidence of pulmonary embolism at presentation or follow up.
The third patient was a 46-year-old man presenting with a history reminiscent of a ruptured Baker cyst and complaining of posterior knee pain. An extensive past medical history included prostate and stomach carcinoma, as well as renal lymphoma requiring a left nephrectomy.
The MRI examination demonstrated edema in the popliteal fossa with a typical filling defect with surrounding enhancement, corresponding to the thrombosed popliteal vein (Fig. 3).
The diagnosis was further supported by positive results from an ultrasound performed 2 days later, demonstrating thrombosis extending to the superficial and common femoral veins.
The fourth patient was a 53-year-old woman presenting with pain in the right calf approximately 2 weeks after total hip replacement. She had been prophylactically treated with anticoagulants, which were found to be in the sub-therapeutic range when she presented.
The MR examination showed edema in the soleus muscle surrounding distended, branching, tubular structures (Fig. 4a). On post-contrast MR images rim enhancement around the thrombosed muscular veins was visible (Fig. 4b).
A 53-year-old female patient presenting with calf pain and swelling 2 weeks after total hip arthroplasty. a Coronal, STIR, MR image shows marked muscle edema-like changes centered on thrombosed, duplicated, sural veins (arrows). b Post-contrast, fat-suppressed, sagittal, T1-weighted, MR image shows enhancement surrounding tubular filling defects (arrows)
A Doppler ultrasound performed on the same day confirmed deep venous thrombosis in a muscular branch; the femoral and popliteal veins were patent.
Discussion
Deep venous thrombosis often forms within the venous cusps of intramuscular branches. Medially and superficially, there is a mesh of venous structures within the gastrocnemius muscle (gastrocnemius plexus); at a deeper plane the sural plexus provides venous drainage for the soleus muscle.
Muscle edema may be due to multiple etiologies, ranging from disuse atrophy; diabetic neuropathy or myopathy [1]; denervation changes [2]; inflammatory and septic myositis; traumatic strain or tears [3]; myonecrosis and rhabdomyolysis [4] to delayed-onset muscle soreness (DOMS) [5]. In the case of denervation or disuse changes, edema-like changes usually overlap with ensuing marbelization of the muscle, which typically creeps outwardly from the musculotendinous junction. Edematous changes in strains tend to have a characteristic feathery pattern resulting from the orientation of the torn muscle fibers. However, patterns of edema are, by and large, non-specific in etiology.
Deep intramuscular thrombophlebitis is not usually a major diagnostic consideration in patients presenting with a clinical history of possible muscle strain and marked muscular edema; rather, the tendency is to favor traumatic etiologies to explain the presence of edema. In these cases, identification of rim-enhancing, branching, tubular structures within the edematous muscles is pathognomonic for deep-venous thrombosis.
Contrast material administration increases the conspicuity of the findings by bringing out the outlines of the branching intramuscular structures as a consequence of the enhancement of vascular walls through vasa vasorum [6].
The clinical management of deep venous thrombosis isolated to the calf has often been debated, resulting in different imaging protocols. As an example, a CT scan from the upper calves to the diaphragm, performed simultaneously with pulmonary CT angiography to detect thrombus in the iliac-femoral vessels and/or popliteal vein, was proposed as a single-test work-up protocol, with the implicit assumption that thrombosis below the popliteal vein may be inconsequential [7, 8].
Doppler ultrasound assessment of the deep venous system below the trifurcation is not generally considered as crucial as the evaluation for patency of the popliteal vein and venous structures cranial to it. Macdonald et al. prospectively followed up with Doppler ultrasound patients with deep venous thrombosis isolated to deep intramuscular calf branches without anticoagulation therapy, and in only 16% of cases with thrombus in the soleal or gastrocnemius plexus was there extension to the adjacent tibial or peroneal veins; further, in only 3% of the cases did the thrombus extend as far up as the popliteal vein; none showed extension to the deep venous system of the thigh [9].
However, diagnosing symptomatic cases of intramuscular deep venous thrombosis is still significant, since identification of thrombophlebitis in the calf during a routine MR study should prompt one to obtain an ultrasound of the entire deep venous system of the bilateral lower extremities to exclude the presence of more extensive or proximal disease.
It is possible that, even in the absence of more proximal involvement, intramuscular calf thrombosis may be associated with pulmonary embolism [10]. Isolated soleus thrombosis has been found in patients with pulmonary embolism when the size of the clot is more than 7 mm in diameter [11].
The soleus or gastrocnemius plexus are involved in approximately 80% of cases of deep venous thrombosis of the lower extremity and, more importantly, in 25% of cases are the only sites of involvement. The soleus plexus is more often involved. In this subset of patients with isolated thrombosis to the intramuscular venous plexuses of the legs, a non-specific history of pain while walking is typical. This fact explains why deep venous thrombosis isolated to the calf may be confused for a muscular or tendinous problem [12].
Even with a directed Doppler ultrasound examination of the intramuscular branches of the calf, the sensitivity of ultrasound is diminished (approximately 88%), as compared with contrast venography (approximately 95%) [12], probably as a result of the small size of intramuscular veins, their physiologic wide range of anatomic variations, and the absence of paired, guiding, arterial structures. Of isolated calf venous thrombosis, 40% of cases will be missed [13]. Although focused ultrasound has been found useful in the detection of isolated intramuscular thrombosis, up to 21% of cases were visualized only with contrast venography [14].
By and large, Doppler ultrasound examinations focus on the main venous trunks of the lower extremity. Below the knee, the posterior tibial veins are routinely examined at the level of the ankle, and the popliteal vein is followed distally to the level of its trifurcation. The peroneal veins are not systematically included, and the anterior tibial veins are only interrogated in cases where the posterior tibial veins are not clearly patent. The intramuscular branches tend not to be included in routine imaging protocols [15].
Probably, this explains the falsely negative ultrasound results in our second patient: given the small size of the clots, it is unlikely that even a focused Doppler ultrasound of the intramuscular venous plexuses could have shown the intramuscular clots more conspicuously than the contrast-enhanced MR study.
This study is limited to four cases that were collected during the course of random case reading sessions. The suspicion of deep venous thrombosis (DVT) was based on the MRI findings. We are unaware of other cases in which a diagnosis of DVT may have been suspected on MRI during the same time period and was simply disproved on further work-up.
In conclusion, isolated intramuscular venous thrombosis should be included in the differential diagnosis of muscle edema in the calf; a clinical suspicion of strain is not unexpected and can be misleading, particularly when MRI shows predominantly edema in the calf muscles. Branching, rim-enhancing, tubular structures within the edematous muscles are diagnostic.
References
Kattapuram TM, Suri R, Rosol MS, Rosenberg AE, Kattapuram SV. Idiopathic and diabetic skeletal muscle necrosis: evaluation by magnetic resonance imaging. Skeletal Radiol 2005;34:203–209
Fleckenstein JL, Watumull D, Conner KE, et al. Denervated human skeletal muscle: MR imaging evaluation. Radiology 1993;187:213–218
May DA, Disler DG, Jones EA, Balkissoon AA, Manaster BJ. Abnormal signal intensity in skeletal muscle at MR imaging: patterns, pearls, and pitfalls. Radiographics 2000;20:S295–S315
Shintani S, Shiigai T. Repeat MRI in acute rhabdomyolysis: correlation with clinicopathological findings. J Comput Assist Tomogr 1993;17:786–791
Evans GF, Haller RG, Wyrick PS, Parkey RW, Fleckenstein JL. Submaximal delayed-onset muscle soreness: correlations between MR imaging findings and clinical measures. Radiology 1998;208:815–820
Ghaye B, Szapiro D, Willems V, Dondelinger RF. Pitfalls in CT venography of lower limbs and abdominal veins. AJR Am J Roentgenol 2002;178:1465–1471
Loud Peter A, Katz Douglas S, Klippenstein Donald L, Shah Rakesh D, Grossman Zachary D. Combined CT venography and pulmonary angiography in suspected thromboembolic disease: diagnostic accuracy for deep venous evaluation. AJR Am J Roentgenol 2000;174:61–65
Cham Matthew D, Yankelevitz David F, Shaham Dorith, Shah Ami A, Sherman Leonard, Lewis Andrew, Rademaker Jurgen, Pearson Gregory, Choi Junsung, Wolff William, Prabhu Pilar M, Galanski Michael, Clark Robert A, Sostman H Dirk, Henschke Claudia I. Deep venous thrombosis: detection by using indirect CT venography. Radiology 2000;216:744–751
Macdonald PS, Kahn SR, Miller N, Obrand D. Short-term natural history of isolated gastrocnemius and soleal vein thrombosis. J Vasc Surg 2003;37:523–527
Hollerweger A, Macheiner P, Rettenbacher T, Gritzmann N. Sonographic diagnosis of thrombosis of the calf muscle veins and the risk of pulmonary embolism. Ultraschall Med 2000;21:66–72
Ohgi S, Tachibana M, Ikebuchi M, Kanaoka Y, Maeda T, Mori T. Pulmonary embolism in patients with isolated soleal vein thrombosis. Angiology 1998;49:759–764
Krunes U, Teubner K, Knipp H, Holzapfel R. Thrombosis of the muscular calf veins—reference to a syndrome which receives little attention. Vasa 1998;27:172–175
Labropoulos N, Webb KM, Kang SS, Mansour MA, Filliung DR, Size GP, Buckman J, Baker WH. Patterns and distribution of isolated calf deep vein thrombosis. J Vasc Surg 1999;30:787–791
Atri M, Herba MJ, Reinhold C, Leclerc J, Ye S, Illescas FF, Bret PM. Accuracy of sonography in the evaluation of calf deep vein thrombosis in both postoperative surveillance and symptomatic patients. AJR Am J Roentgenol 1996;166:1361–1367
Rumack CM, Wilson SR, Charboneau JW. Diagnostic ultrasound, 2nd ed. St. Louis, Mo: Mosby; 1998. pp. 944–949
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parellada, A.J., Morrison, W.B., Reiter, S.B. et al. Unsuspected lower extremity deep venous thrombosis simulating musculoskeletal pathology. Skeletal Radiol 35, 659–664 (2006). https://doi.org/10.1007/s00256-006-0128-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-006-0128-y