Abstract
Objective
To evaluate high-resolution MRI of the proximal zone of the lunotriquetral ligament (LTL) using a microscopy surface coil with a 1.5 T scanner.
Design and subjects
The proximal zone of the LTL was reviewed in 90 subjects (23 asymptomatic normal volunteers and 67 patients with suspicion of triangular fibrocartilage complex injury) with high-resolution MRI using a 47-mm microscopy surface coil. High-resolution MR images were obtained with gradient recalled echo (GRE) T2*-weighted sequence and short tau inversion recovery imaging, with a 1- to 1.5-mm slice thickness, a 50-mm field of view, an imaging matrix of 140-224×512 using zero fill interpolation, and 3-4 excitations. As a qualitative analysis, the LTL was classified in shape and signal intensity.
Results
The triangle-shaped low-signal-intensity LTL was identified in 77 of 90 subjects (85.6%) on GRE images. The triangle was classified as regular (41.1%), broad-based (20.0%), narrow-based (6.7%), or asymmetrical (17.8%). The bar-shaped ligament was seen in one patient, and unclassified ligaments were seen in 12 patients. All volunteers showed triangle-shaped LTL. The MR signal intensity of the proximal zone in the LTL was characterized as homogeneously low intensity (type 1; 33.8%), linear intermediate or high signal intensity traversing the distal surface of the LTL (type 2; 45.5%), and linear intermediate or high intensity traversing both distal and proximal surfaces of LTL (type 3; 20.8%).
Conclusion
The proximal zone of the LTL showed a broad spectrum of normal variations in shape and signal intensity on high-resolution MR images with a microscopy coil.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Magnetic resonance imaging (MRI) is an excellent modality with which to assess hand and wrist pathology, including ligament injuries. Because each ligament of the hand and wrist is thin and short, high-resolution MRI is essential to diagnose disorders in this area. Recent MR technology allows the use of microscopy coils, which enable high-resolution MRI of the hand, wrist, and elbow at 1.5 T [1, 2]. High-resolution MRI implies small pixel size images yielded by a smaller field of view and a higher matrix with thinner section thickness. High-resolution MR images with a microscopy coil (23 mm or 47 mm in diameter) showed superior signal-to-noise ratios and contrast-to-noise ratios to those with a small surface coil (80 mm in diameter) and provided detailed anatomy of the triangular fibrocartilage complex (TFCC) [1].
The intercarpal ligaments of the wrist are a complex structure that plays an important role in wrist stability. However, accurate diagnosis of lunotriquetral ligament (LTL) injury with MRI is often difficult because of low resolution and low contrast. The accuracy of MRI in diagnosis of LTL tear has been disappointing, with sensitivities from 0–56% and specificities from 46–100% [3–5]. Smith et al. have reported that the proximal zone of the LTL showed a variety of shapes and signal intensities [6]. Therefore, it is important to gain familiarity with the normal MR appearance of the LTL proximal zone using high-resolution techniques to improve diagnosis of LTL injury. The purpose of the current study was to evaluate high-resolution MRI of the proximal zone of the LTL in asymptomatic normal volunteers and in patients with suspicion of TFCC injury, using a microscopy surface coil with a 1.5 T scanner.
Design and subjects
The proximal zone of the LTL was retrospectively assessed in 90 subjects (42 males and 48 females; 23 of these were asymptomatic normal volunteers, and 67 were patients being imaged for suspicion of TFCC injury) with high-resolution MRI using a 47-mm microscopy surface coil (Philips Medical Systems, Best, The Netherlands). The patients showed positive signs for the painful click test and pain due to ulnar deviation, and negative for traction and pronation/supination. However, patients who were diagnosed clinically with LTL injury were excluded from this study. The radiographs of all patients were negative for lunate triquetral dissociation, volar intercalated segment instability (VISI), and dorsal intercalated segment instability (DISI). MR images of the patients were performed as a routine MR examination of the TFCC injury between March 2002 and September 2003. Subject ages ranged from 14 to 67 years, with a mean age of 31.2 years (a mean age of 27.5 years for volunteers and 33.8 years for patients). Each volunteer and patient gave written informed consent. All MR images were obtained with a 1.5 T scanner (Gyroscan NT Intera, Philips Medical Systems, Best, The Netherlands). High-resolution coronal MR images were obtained with 2D gradient recalled echo (GRE) T2*-weighted sequence (T2*WI) (repetition time (TR)/ echo time (TE) / flip angle=270-608/13-18/40), and short tau inversion recovery (STIR) imaging (TR/TE/ inversion time (TI)=3007-5492/90/150), with a 1- to 1.5-mm slice thickness, a 0.1- to 0.15-mm interslice gap, a 50-mm FOV, an imaging matrix of 140-224×512 using zero fill interpolation, and 3-4 excitations. Twenty-one patients with wrist pain underwent arthroscopy or arthrography, which detected no evidence of LTL tears. The remaining 46 did not undergo arthroscopy or arthrography to confirm or rule out injury to the LTL.
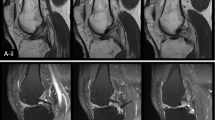
In our qualitative analysis, the shape and signal intensity of the LTL proximal zone, and the direction of high-signal-intensity direction inside the proximal zone were evaluated by consensus of two muskuloskeletal radiologists (HY, TU) using a 2D GRE sequence. The shape of the LTL proximal zone was classified into five types (type 1: regular triangle, type 2: broad-based triangle, type 3: narrow-based triangle, type 4: asymmetrical triangle, and type5: bar shape; Fig. 1). Our study chose the slice in which the largest triangle was found, and signal characteristics in the proximal LTL were evaluated in the same slice. The signal intensity of the LTL proximal zone was classified into three types (type 1: homogeneously low intensity, type 2: linear intermediate or high signal intensity traversing the distal surface, and type 3: linear intermediate or high intensity traversing both proximal and distal surfaces; Fig. 2) [6]. Among type 2 and type 3 signal intensities, the direction of intermediate or high signal intensity inside the proximal zone was classified into five types (type 1: radius–radius (RR) pattern, type 2: radius–ulna (RU) pattern, type 3: ulna–radius (UR) pattern, type 4: ulna–ulna (UU) pattern, and type 5: center (c) pattern) (Figs. 3 and 4). The RR pattern indicated high signal intensity traversing the radial side of the distal surface toward the radial side of the proximal surface, and the RU pattern indicated high signal intensity traversing the radial side of the distal surface toward the ulnar side of the proximal surface. The center pattern shows high signal intensity traversing the center of the proximal zone. The Mann-Whitney U-test was used to determine the significance of the differences in ages among analyzed groups. In each analysis, a P value of ≤0.05 was considered significant.
Drawing shows classifications for proximal LTL signal intensity; a type 1=homogeneously low intensity, b type 2=linear intermediate or high signal intensity traversing the distal surface, and c type 3=linear intermediate or high intensity traversing both proximal and distal surfaces. High-resolution MR images with a microscopy coil show corresponding signal intensity type; d=type 1, e=type 2, and f=type 3
Results
With thin sections in our study, the triangular shape of the LTL proximal zone could be consistently discerned over several slices. In addition, the linear shape was seen more often in or near the volar zone than in the proximal zone. Therefore, each subject had both linear and triangle shapes. The LTL in 77 of 90 subjects (85.6%) was found to be triangular-shaped (types 1-4) low signal intensity. The regular triangular shape (type 1) was most frequent (41.1%), followed by the broad-based triangle (type 2, 20.0%) and the asymmetrical triangle (type 3, 17.8%) (Table 1). The bar-shaped ligament was seen in only one patient. The LTL of 12 patients was not classified; one showed lunotriquetral coalition, one was not classified due to motion artifact, and ten were not classified due to difficulty of tracing a definite shape. These ten patients ranged in age from 34 to 67 years; their mean age was 53.4 years, making them significantly older than the remaining patients (p<0.0001) or normal volunteers (p<0.0001). All volunteers were found to have triangular-shaped LTL. Out of 77 patients with a triangular-shaped LTL proximal zone, the percentage of each signal intensity type was as follows; 33.8% type 1, 45.5% type 2, and 20.8% type 3 (Table 2). Two-thirds showed intermediate or high intensity inside the proximal LTL. Eight (30.8%) out of 26 patients with type 2 signal intensity showed linear high signal intensity on STIR images, while no type 3 patients did (Fig. 5). Of patients with non-classified LTL shape, six showed high signal intensity in the proximal zone with STIR. These cases could have suffered LTL tears. However, arthroscopy examination was not performed in five cases, because they were judged to have no indication for arthroscopy after MRI and physical examination. In one case, the proximal LTL could not be observed due to severe ulnotriquetral ligament injury on arthroscopy. Intermediate or high-signal-intensity direction pattern inside the proximal zone was assessed in the type 2 and type 3 signal-intensity patterns. RR and RU patterns were most frequent (both patterns were found in 29.4% of 51 subjects; Table 3). Both volunteers and patients with suspicion of TFCC injury revealed similar distribution in signal-intensity and high-signal-intensity direction characteristics (Tables 2 and 3).
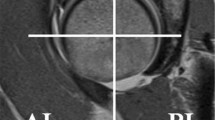
a GRE image shows type 2 LTL signal intensity (linear intermediate or high signal intensity traversing the distal surface) (arrow). There is a small amount of fluid collection adjacent to distal surface of the proximal zone with (b) STIR sequence (arrow), while no signal intensity or morphological change is seen in proximal area inside the LTL with STIR, suggesting no injury
Discussion
The LTL is an intrinsic wrist ligament that is V-shaped on sagittal section and has three separate zones (dorsal, proximal, and volar). The dorsal and volar zones are ligamentous. The former is highly important functionally, particularly as a restraint to rotation, while the latter is the strongest and thickest of all three zones and transmits the extension moment of the triquetrum [7, 8]. The proximal zone is fibrocartilaginous, and shows close approximation to the triangular fibrocartilage complex histologically. It is thin (≤1–1.5 mm) and difficult to see reliably [7]. Many previous studies have discussed LTL injuries using the coronal plane even though the proximal portion of the LTL has poor biomechanical function compared to the dorsal and volar portions. It seems important, therefore, to know normal findings of the LTL in the coronal plane. The axial plane is better for assessing injuries to the dorsal and volar portion, which are biomechanically more important. High-resolution MRI of the dorsal and volar injuries with axial planes using a microscopy coil would be more clinically useful, and a preliminary study has shown this [9].
Earlier MR studies for diagnosis of LTL tears showed relatively good results. Zlatkin et al. reported sensitivity of 56%, specificity of 100%, and accuracy of 90% with MR imaging in the diagnosis of LTL tears compared with arthrography [4]. Schweitzer et al. reported that the average sensitivity of nonvisualization of the LTL with MRI was 68.8%, with average specificity 56.1% and accuracy 59.6%, when compared with arthroscopy [3]. With regard to abnormal morphology of the LTL, the average sensitivity was 31.2%, with average specificity of 90.2%, and average accuracy of 77.8% for LTL tears, with arthroscopy as the standard. However, some other studies showed relatively poor results, reporting 0–22% sensitivity of MRI compared with arthroscopy [5, 10], although one study used a 0.5 T MR machine. Consistent visualization of the LTL with a low-field-strength extremity magnet is difficult [11]. Even with a 1.5 T scanner, partial tears showed lower sensitivity and specificity than complete tears, suggesting that MRI was not accurate for diagnosing partial LTL tears [12]. Zanetti et al. reported sensitivity of 28.6–35.7% and specificity of 81.3–93.8% with standard MRI for LTL tears, while direct MR arthrography yielded sensitivity of 21.4–35.7% and specificity of 93.8% [13]. These low sensitivities in recent studies seem disappointing, given the advances in MR technology of magnets, gradient strength, coils, and pulse sequences. The poor results may be explained by inappropriate slice thickness and pulse sequences, resulting in low spatial resolution and poor-contrast images. Dedicated coils for the wrist should have been used to obtain high signal-to-noise ratio images. There may be a lack of familiarity with normal anatomical MR findings of the LTL. A thorough review of LTL morphology and signal intensity with high-resolution techniques will improve the accuracy of diagnosis of LTL tears.
Classifications of LTL shape and signal intensity have been reported elsewhere [6]. LTL shape is classified as linear, delta-shaped, amorphous, or not seen. Smith et al. found the LTL to be linear in 63% and delta-shaped (triangular-shaped) in 35% of subjects [6], while our study suggested 85.6% of subjects had triangular shape. The 3-mm section thickness and 10-cm FOV used in the previous study [6] might have made it difficult to discriminate between a linear shape in or near the volar zone and a delta shape in the proximal zone. The appearance of an intercarpal ligament on an MRI depends on section thickness and spatial resolution.
The previous study found homogeneous low signal intensity in 73% and linear intermediate signal intensity traversing all or part of the LTL in 25% of subjects [6], whereas homogeneous low signal intensity was found only in 33%, with the remaining subjects having intermediate or high signal intensity traversing proximal LTL in this study. This discrepancy could be explained by the differences in section thickness and spatial resolution, as well as contrast between the study of Smith & Snearly and our own [6]. The signal-to-noise ratios for each structure and contrast-to-noise ratios among structures in the wrist when using microscopy coils was significantly higher than those using an 80-mm surface coil using 5-cm FOV [1]. The high intensity in the LTL proximal zone with STIR sequence was seen in type 2 signal intensity pattern, not type 3 signal intensity pattern, which may suggest a small amount of effusion in the lunotriquetral joint is trapped into the folded LTL between the lunate and triquetral bones. High-resolution MRI with a microscopy coil allowed clear visualization of subtle linear intermediate and high signal intensity in the LTL proximal zone in the current study.
Interestingly, ten patients whose LTLs could not be classified as either triangular- or bar-shaped (except for lunotriquetral coalition and motion artifact) were significantly older than the remaining patients and normal volunteers. Of the ten, six patients showed high signal intensity even with STIR sequence. This may suggest a degenerative change or minor injury in the LTL, though no confirmation of pathology was available [14]. Smith et al. also suggested that the amorphous LTL shape in their cases represented diffuse degenerative changes [6]. Schweitzer et al. reported that failure to visualize the scapholunate ligament indicated a tear, but this was not helpful in evaluation of the LTL [3]. The lack of visualization may reflect the fact that the LTL is a very thin structure, and degeneration renders its signal intensity very similar to that of the surrounding tissue, especially cartilage.
High-resolution MRI with a microscopy coil has several advantages. Firstly, small FOV (high-resolution) imaging with high signal-to-noise ratio becomes available. Secondly, this technique allows excellent contrast between the LTL proximal zone and surrounding tissue, making it easier to discern the triangular shape and detect intermediate or high signal intensity in the proximal zone. Thirdly, thin sections allowed us to visualize the triangular shape in multiple slices, and to discriminate between the triangular shape in the proximal zone and the band shape in the volar zone. Fourthly, this system is commercially available, allowing combination of almost all sequences with 2D or 3D acquisition. Therefore, our study supports the contention that high-resolution MRI with a microscopy coil can detect a wide variety of normal morphological and signal intensity variations in the LTL.
There are several limitations in our study. Firstly, 3D GRE sequence was not used in this evaluation, even though some studies suggest that this sequence provides detailed information about the wrist [15–20]. However, we used section thickness on 2D MR images similar to that used in previous 3D studies, higher spatial resolution, and smaller FOV (50 mm). Secondly, because each slice shows only small changes in LTL shape and signal intensity, the selection of the slices might have been subjective. Thirdly, the mean age of the normal volunteers in this study is younger than that of patients. The selection of asymptomatic patients with different age ranges would be preferable. Fourthly, this study is a retrospective study in which patients with suspicion of TFCC injury and normal volunteers were included. The reason we choose the LTL is because this ligament was included in 5-cm FOV for evaluating the TFCC. The 5-cm FOV is not large enough to cover all intrinsic ligaments. Therefore, we need a different coil setting with larger FOV for that. Fifthly, though it would be useful to be familiar with these variations for purposes of improving diagnosis of LTL tears, such a wide variety might also complicate diagnosis if based only on LTL shape and signal intensity. Further evaluations will be needed with additional indirect findings such as bone-marrow edema or fluid collection, or the use of other MR techniques such as MR arthrography or 3D reconstruction with isotropic acquisition for accurate diagnosis of LTL tears. Sixthly, because the LTL dorsal and volar portion is biomechanically more important, high-resolution MRI of these injuries with axial planes using a microscopy coil should be assessed in a future study.
In conclusion, the proximal zone of the LTL showed a broad spectrum of normal variations in shape and signal intensity, which was clearly visualized on high-resolution MR images using a microscopy coil.
References
Yoshioka H, Ueno T, Tanaka T, Shindo M, Itai Y. High-resolution MR imaging of triangular fibrocartilage complex (TFCC): comparison of microscopy coils and a conventional small surface coil. Skeletal Radiol 2003;32:575–581
Yoshioka H, Ueno T, Tanaka T, Kujiraoka Y, Shindo M, Takahashi N, Nishiura Y, Ochiai N, Saida Y. High-resolution MR imaging of the elbow using a microscopy surface coil and a clinical 1.5 T MR machine: preliminary results. Skeletal Radiol 2004;33:265–271
Schweitzer ME, Brahme SK, Hodler J, Hanker GJ, Lynch TP, Flannigan BD, Godzik CA, Resnick D. Chronic wrist pain: spin-echo and short tau inversion recovery MR imaging and conventional and MR arthrography. Radiology 1992;182:205–211
Zlatkin MB, Chao PC, Osterman AL, Schnall MD, Dalinka MK, Kressel HY. Chronic wrist pain: evaluation with high-resolution MR imaging. Radiology 1989;173:723–729
Johnstone DJ, Thorogood S, Smith WH, Scott TD. A comparison of magnetic resonance imaging and arthroscopy in the investigation of chronic wrist pain. J Hand Surg [Br] 1997;22:714–718
Smith DK, Snearly WN. Lunotriquetral interosseous ligament of the wrist: MR appearances in asymptomatic volunteers and arthrographically normal wrists. Radiology 1994;191:199–202
Daunt N. Magnetic resonance imaging of the wrist: anatomy and pathology of interosseous ligaments and the triangular fibrocartilage complex. Curr Probl Diagn Radiol 2002;31:158–176
Shin AY, Battaglia MJ, Bishop AT. Lunotriquetral instability: diagnosis and treatment. J Am Acad Orthop Surg 2000;8:170–179
Yoshioka H, Ueno T, Tanaka T, Shindo M, Lang P. High-resolution MR imaging of the intercarpal ligaments with a microscopy coil. In: Proceedings of RSNA 90th Scientific Assembly and Annual Meeting 2004
Haims AH, Schweitzer ME, Morrison WB, Deely D, Lange RC, Osterman AL, Bednar JM, Taras JS, Culp RW. Internal derangement of the wrist: indirect MR arthrography versus unenhanced MR imaging. Radiology 2003;227:701–707
Ahn JM, Brown RR, Kwak SM, Kang HS, Muhle C, Botte MJ, Trudell D, Haghighi P, Resnick D. Evaluation of the triangular fibrocartilage and the scapholunate and lunotriquetral ligaments in cadavers with low-field-strength extremity-only magnet. Comparison of available imaging sequences and macroscopic findings. Invest Radiol 1998;33(7):401–406
Manton GL, Schweitzer ME, Weishaupt D, Morrison WB, Osterman AL, Culp RW, Shabshin N. Partial interosseous ligament tears of the wrist: difficulty in utilizing either primary or secondary MRI signs. J Comput Assist Tomogr 2001;25:671–676
Zanetti M, Bram J, Hodler J. Triangular fibrocartilage and intercarpal ligaments of the wrist: does MR arthrography improve standard MRI? J Magn Reson Imaging 1997;7:590–594
Kang HS, Kindynis P, Brahme SK, Resnick D, Haghighi P, Haller J, Sartoris DJ. Triangular fibrocartilage and intercarpal ligaments of the wrist: MR imaging. Cadaveric study with gross pathologic and histologic correlation. Radiology 1991;181:401–404
Totterman SM, Miller R, Wasserman B, Blebea JS, Rubens DJ. Intrinsic and extrinsic carpal ligaments: evaluation by three-dimensional Fourier transform MR imaging. AJR Am J Roentgenol 1993;160:117–123
Totterman SM, Miller RJ. Triangular fibrocartilage complex: normal appearance on coronal three-dimensional gradient-recalled-echo MR images. Radiology 1995;195:521–527
Totterman SM, Miller RJ. Scapholunate ligament: normal MR appearance on three-dimensional gradient-recalled-echo images. Radiology 1996;200:237–241
Totterman SM, Miller RJ, McCance SE, Meyers SP. Lesions of the triangular fibrocartilage complex: MR findings with a three-dimensional gradient-recalled-echo sequence. Radiology 1996;199:227–232
Potter HG, Asnis-Ernberg L, Weiland AJ, Hotchkiss RN, Peterson MG, McCormack RR Jr. The utility of high-resolution magnetic resonance imaging in the evaluation of the triangular fibrocartilage complex of the wrist. J Bone Joint Surg Am 1997;79:1675–1684
Hobby JL, Tom BD, Bearcroft PW, Dixon AK. Magnetic resonance imaging of the wrist: diagnostic performance statistics. Clin Radiol 2001;56:50–57
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoshioka, H., Tanaka, T., Ueno, T. et al. High-resolution MR imaging of the proximal zone of the lunotriquetral ligament with a microscopy coil. Skeletal Radiol 35, 288–294 (2006). https://doi.org/10.1007/s00256-005-0070-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-005-0070-4