Abstract
Objective
To evaluate whether MRI correlates with CT and SPECT imaging for the diagnosis of juvenile spondylolysis, and to determine whether MRI can be used as an exclusive image modality.
Design and patients
Juveniles and young adults with a history of extension low back pain were evaluated by MRI, CT and SPECT imaging. All images were reviewed blindly. Correlative analyses included CT vs MRI for morphological grading and SPECT vs MRI for functional grading. Finally, an overall grading system compared MRI vs CT and SPECT combined. Statistical analysis was performed using the kappa statistic.
Results
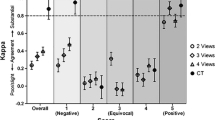
Seventy-two patients (mean age 16 years) were recruited. Forty pars defects were identified in 22 patients (31%), of which 25 were chronic non-union, five acute complete defects and ten acute incomplete fractures. Kappa scores demonstrated a high level of agreement for all comparative analyses. MRI vs SPECT (kappa: 0.794), MRI vs CT (kappa: 0.829) and MRI vs CT/SPECT (kappa: 0.786). The main causes of discrepancy were between MRI and SPECT for the diagnosis of stress reaction in the absence of overt fracture, and distinguishing incomplete fractures from intact pars or complete defects.
Conclusions
MRI can be used as an effective and reliable first-line image modality for diagnosis of juvenile spondylolysis. However, localised CT is recommended as a supplementary examination in selected cases as a baseline for assessment of healing and for evaluation of indeterminate cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spondylolysis is a defect of the pars interarticularis, and is most commonly encountered in the lower lumbar spine. A number of factors may predispose to the development of spondylolysis [1,2]. One cause is a stress fracture occurring during adolescence [2, 3, 4,5], which is frequently encountered in physically active individuals and may occur in many different sporting activities, including cricket, soccer, American football, weightlifting, rowing, and gymnastics [6].
Imaging may be utilised to detect spondylolysis, distinguish acute and active lesions from chronic inactive non-union, and to assess bony healing in follow-up of acute lesions. Conventional radiography is often the first-line imaging modality, and techniques include routine anteroposterior (AP) and lateral views, oblique views and angled AP views [7,8]. However, although chronic non-union may be demonstrated, radiography is unreliable for detection of early and acute lesions [2,9].
Isotope imaging with single photon emission tomography (SPECT), is considered to be an extremely sensitive technique for early diagnosis of acute lysis [5, 9,10], and may be predictive of the ability for lysis to heal. Unfortunately, SPECT is nonspecific, detects only 17% of chronic lesions [10], and cannot distinguish between stress reaction and overt fractures. Developmental lesions acquired in the first decade are often asymptomatic and usually inactive on isotope studies.
Computed tomography (CT) is probably the best method for demonstrating spondylolytic defects [11, 12, 13,14], and may also be used for assessment of healing. Reverse-angle axial oblique CT has been utilised successfully for identifying defects, by demonstrating discontinuity in the bony ring of the posterior elements of the vertebra [12] (Fig. 1). However, CT is limited in detection of other pathological processes, and it cannot reliably distinguish between active and inactive lesions. Magnetic resonance imaging (MRI) has the advantage of not utilising ionising radiation, and early studies of MRI in spondylolysis and spondylolisthesis described a morphological grading system of pars defects [15, 16,17] (Fig. 2). Signal changes that mirrored the Modic type changes of vertebral endplates have also been described [18]. However, most of this work was predominantly performed in the adult population and did not utilise fat-suppressed T2-W sequences. MRI has been shown to demonstrate the normal pars with high interobserver correlation [17,19]. A new grading system has been described that utilises both the morphological information of MRI combined with the presence or absence of marrow oedema on fat-suppressed T2-W images [20]. This distinguishes between stress reaction and active and inactive spondylolysis, and has also been shown to have a high interobserver correlation. However, to our knowledge there have been no correlative studies assessing MRI with other imaging modalities, in order to determine the reliability of MRI in detection and diagnosis of adolescent spondylolysis. The aim of this paper was to determine the level of correlation of MRI with SPECT and CT imaging, and to determine if MRI can effectively replace CT and SPECT imaging.
Graphical representation ( A) of the positioning plane for reverse-angle oblique axial CT and MRI. The CT image ( B) demonstrates a break in the left pars interarticularis due to a unilateral spondylolytic defect. A multiplanar reformatted (MPR) image from a sagittal 3D gradient echo MRI in a different patient ( C) illustrates a normal posterior arch with continuous marrow signal and an intact low-signal cortex
Pars grading on sagittal T1-W MR imaging. A grade I pars ( Ahas continuous marrow signal throughout the pars interarticularis ( white arrow), with intact cortical margins. In grade II pars ( B) an area of low signal ( open black arrow) due to sclerosis or partial volume effects is present. A pars grade IV defect ( C) is manifested by interruption of the cortical margin and the normal marrow signal ( black arrow)
Method
Adolescents and young adults with a history of recent onset, or exacerbation of extension back pain were recruited for the study. Referrals were accepted from primary care physicians, sports physicians and spinal surgeons. In all cases the patients underwent imaging with CT, SPECT and MRI, usually on the same day. Ethics approval was obtained prior to undertaking the study. Informed consent was obtained either from the patient or from a parent in the case of children under 16 years of age. The radiation dose from SPECT was justified on the grounds that adolescents with extension back pain would conventionally be investigated with a SPECT scan. The CT was justified as an alternative to conventional radiography, which was not routinely performed, and as a means of providing a gold standard for confirming pars integrity. In some cases radiographs had been performed at the request of a primary care physician, but these were not repeated, and no supplementary views, such as obliques, were obtained.
SPECT
SPECT imaging was initiated approximately 3 h after administration of an appropriate paediatric dose (reduced in proportion to body weight against an approved adult diagnostic reference level of 600 MBq) of 99Tcm–HDP (Mallinckrodt Medical). Images were acquired with a single-headed rectangular gamma camera (Camstar XRT, GE Medical Systems) fitted with a low-energy, high-resolution collimator. Projection data was acquired into a 64×64 matrix (Gamma II, Nuclear Diagnostics) at each of 32 angles over a 180° rotation around the subject’s back. Tomographic reconstruction was performed on a Hermes Workstation (Nuclear Diagnostics), using a method of filtered back projection, and images were produced in the axial, sagittal and coronal planes.
MRI
All MR examinations were performed on a 1T Siemens Impact/Expert system, using a phased-array spine coil. Each examination included 3 mm sagittal T1-W images and 3 mm reverse-angle oblique axial T1-W images (TE 14/ TR 420–630/ interslice gap 0.3 mm), and a sagittal 3D spoiled gradient echo (FLASH) sequence (TE 7/ TR 27/ FA 30°/ effective slice thickness 1.9 mm). Fluid-sensitive sequences included 4 mm sagittal short inversion-time inversion-recovery (STIR) images, and 3 mm reverse-angle oblique axial STIR images (TI 150/ TE 60/ TR 3,900–5,900/ interslice gap 0.8 mm). In some cases the sagittal STIR was replaced with 4 mm sagittal fat-saturated T2-W images (TE 120/ TR 5,000/ interslice gap 0.8 mm). The sagittal images were acquired with 280–300 mm rectangular field of view (FOV), and the reverse axial images at 230 mm FOV. The matrix size was 256 in the frequency encoding direction, and varied from 170–190 in the phase encoding direction. The reverse-angle oblique axial T1-W and STIR images were acquired through the lower three lumbar levels only.
CT
CT imaging was performed after the SPECT and MRI examinations on a Tomoscan SR 7000 (Philips Medical Systems). Images were acquired in the reverse-angle axial plane at the L4 and L5 levels. Approximately six to seven contiguous slices were acquired at each level with 3 mm slice thickness, (table index 3 mm, 120 kV, 175 mA, and a 2 s scan time). The effective dose was 1.0 mSv for each level, plus 0.2 mSv for the topogram image. For most patients this resulted in a total effective dose of 2.2 mSv. This compares with a total effective dose of 1.0 mSv for a conventional three-view lumbar spine radiograph. Spiral imaging through L4 and L5 was not performed, as this would have significantly raised the radiation dose, and multi-slice CT with dose-reduction techniques was not available during the period of the study.
If any abnormality was detected above the L4 on either SPECT or MRI, further CT images were also acquired at that level.
Data analysis
Every pars interarticularis was assessed individually on each image modality by one of three experienced skeletal radiologists: MRI (A.J.G.), CT (R.C.) and SPECT (I.G.H.). Each radiologist was blinded to the results of the other image modalities.
The SPECT images were reported as either positive (increased uptake in the pars greater than the adjacent vertebral body, or an ipsilateral pars at an adjacent level) or negative (uptake equal or less than the adjacent vertebral body, or adjacent pars). Two grading systems were used for the MRI images. Firstly, the morphological appearance of each pars was assessed on the T1-W and 3D gradient refocused echo (GRE) sequences, using a previously described grading system modified for this study (Table 1). The 3D GRE images were evaluated in the sagittal plane, and with multiplanar reconstruction, using either a reverse-angle oblique axial or oblique sagittal plane (Fig. 1C and Fig. 3). Secondly, the STIR/ fat-saturated T2-W images were evaluated for the presence or absence of marrow oedema. The CT images of each pars were graded using the same system as for the T1-W/3D GRE MR images. During the study, partial fractures of the pars were encountered (Fig. 4) that had not been previously described on the MRI grading system. Consequently, the system was modified, and grade IV pars were divided into incomplete (IVa) and complete (IVb) fractures.
Graphical representation ( A) of the positioning plane for oblique sagittal MPRs. This position produces the MRI equivalent of the oblique radiograph “Scotty dog” appearance, with a normal intact pars ( white arrow) ( B), and a spondylolysis with a break in the neck of the “Scotty dog” ( black arrow ( C). Both MR images were acquired from a 3D sagittal gradient echo sequence
A unilateral grade 2 incomplete pars defect. The coronal SPECT image ( A) demonstrates an active area in the left pars of L5. The sagittal 3D gradient echo image ( B) shows interruption of the inferior cortex of the pars ( black arrow), with an area of reactive marrow oedema on the reverse-angle STIR image ( white arrow) ( C). The fracture line propagates from the inferior and medial cortex on the CT image ( D), but does not breach the lateral cortex ( white arrowheads)
Comparative analyses between the different imaging modalities were performed using the kappa statistic [21] (levels of agreement: <2.0, poor; 2.0 to 0.4, fair; 0.41 to 0.6, moderate; 0.61 to 0.8, good; 0.81 to 1.0, excellent). The morphological grading for each pars, on CT and MRI were compared. Increased uptake on the SPECT images was compared with the presence or absence of marrow oedema on the STIR/fat-saturated T2-W MR images. Finally, an overall grading system (Table 2) was used to compare the combined information from the CT and SPECT images with MRI. For the purposes of this grading system, all grade I and grade II pars were considered to be intact (grade 0: normal, or grade 1:stress reaction), and any pars graded indeterminate by MRI (grade III) were considered to be complete defects (grades 3 or 4, dependant on the presence of marrow oedema).
Any discrepancies between the MRI grading and the CT and SPECT grading were reviewed. In each case the final diagnosis used as the gold standard was derived from the combined grading of CT and SPECT, to distinguish between stress reaction and fracture, and active and inactive lesions.
Results
Seventy-two patients were recruited into the study. The age range was 8–26 years (mean age 16 years). There were 45 males and 27 females. Forty pars defects were identified in 23 patients (32%). Bilateral defects were identified in 13 patients, three of whom also had defects at a second contiguous level. Unilateral isolated defects were seen in another ten cases. No cases were encountered with defects at more than two lumbar levels. Twenty-five of the pars defects were chronic established lysis. Fifteen defects were acute or active lesions with increased activity on the SPECT scan (Fig. 5), ten of which were partial or incomplete fractures. One patient has been excluded from the final analysis, as SPECT and MRI both showed a focal lesion in the posterior elements of L2 that was considered to be an osteoid osteoma. Subsequently, a localised spiral CT examination was performed in order to optimally demonstrate the lesion, and further reverse-angle oblique imaging of the lower lumbar levels was not considered to be appropriate.
Acute or active grade 3 bilateral spondylolysis with increased uptake on the coronal SPECT image ( A). The defects are evident on reverse-angle T1-W images ( black arrows) ( B), and oedema is present on the equivalent STIR image ( white arrows) ( C). The correlative reverse-angle CT demonstrates bilateral pars defects ( D)
Comparative analysis
SPECT vs MRI
All ten lumbar pars of each patient were evaluated for this analysis in the remaining 71 patients (710 pars). The results are presented in Table 3, and the kappa statistic was 0.794, showing good agreement between SPECT and MRI. In view of the high number of negative cases in the upper lumbar spine, which might distort the kappa statistics, the kappa value was recalculated for the L4 and L5 levels only. This remained good agreement (kappa: 0.774).
There were nine cases of discordance, which are discussed further in the overall comparative analysis.
CT vs MRI
The comparison of CT and MRI is presented in Table 4. There were a total of 294 pars evaluated by both studies. In four patients a total of an extra ten pars above the L4 were evaluated because of suspected abnormality either on SPECT or MRI. The kappa statistic showed an excellent level of agreement (kappa: 0.829). The grade I and grade II pars have been considered as a single group to simplify the analysis, because on CT both grades are considered to be intact.
There were several cases of discordance. Four complete defects on CT were graded indeterminate on MRI. All four of these pars defects occurred in one patient in whom there was significant movement artifact. They occurred at the L2 and L3 levels, and although there was a high degree of suspicion of complete defects, the exact criteria for categorising grade IV could not be met. One complete defect on CT was graded intact by MRI, although on review, a defect was evident in a dysplastic pars with associated spina bifida occulta. In another case an intact but dysmorphic pars with a step in the cortex was demonstrated on CT. This may have been the result of an old healed fracture. On MRI the sagittal image displayed typical features of a grade IV complete defect (Fig. 6).
The greatest area of discordance was encountered with pars graded as incomplete or partial defects on CT. This is discussed further in the overall comparative analysis.
CT/SPECT vs MRI
For the purposes of the comparative analysis, all pars that had been graded as indeterminate (grade III) by MRI were considered to be complete defects. The results are presented in Table 5. The kappa statistic gave good agreement (kappa: 0.786). Discordance was greatest for the diagnosis of stress reaction (grade 1). Only one of 11 cases showed concordance, and the ten cases of discordance account for all the cases of discordance in the SPECT vs MRI comparative analysis.
Discordance was also noted for the diagnosis of incomplete defects (grade 2). Out of ten cases, three were downgraded to stress reaction (grade 1) by MRI, and three of ten were diagnosed as complete acute defects (grade 3), and two of these were indeterminate on the CT vs MRI grading. However, all cases of incomplete defects demonstrated marrow oedema on MRI correlating with a positive SPECT scan.
Summary
Of the 40 pars defects diagnosed in this study, using the CT and SPECT combined as the gold standard, 29 of 40 (73%) were correctly graded by MRI. However, 39 of 40 (98%) demonstrated some MRI abnormality, either signal change or morphological abnormality. Discordance was greatest for the diagnosis of stress reaction in the absence of a pars defect, and for the grading of incomplete defects.
Discussion
Isthmic spondylolysis is thought to most commonly occur as a developmental phenomenon during the first decade of life [1,22], but stress fractures during adolescence are also encountered. There may also be a genetic predisposition [2]. Fredrickson reported a 4.4% incidence of spondylolysis at age 6 years, rising to 6% by adulthood in a longitudinal study [1]. However, nearly two-thirds of subjects in this study were lost to follow-up after age 10–12 years. The adult incidence may have been higher, and has been reported to occur in up to 10% of the general population [5,23]. The true prevalence of spondylolysis occurring during teenage years as the result of a stress injury is not well documented, but has been reported to occur in up to 40% in some athletes.
Low back pain is a common symptom among both juveniles and adults, and a number of different pathophysiological processes may occur, either in isolation or in combination [24]. Many of these processes may be diagnosed by MRI. In this study, as well as spondylolysis, MRI also demonstrated vertebral endplate irregularities, ring apophyseal injuries, intervertebral disc abnormalities including fissures, degeneration and protrusion, one osteoid osteoma and one transverse process fracture. Lytic spondylolisthesis was present in only one patient, with chronic inactive bilateral defects. No foraminal stenosis resulting from changes secondary to chronic lysis was encountered in this group of patients. While MRI may be helpful in determining which abnormalities are the most likely contributors to back pain, it is well recognised that abnormalities may be detected on MR in asymptomatic patients [25].
In spondylolysis the aim of MRI is to first detect lysis, and subsequently categorise defects as part of treatment planning and prognosis. Healing is not a feature of developmental spondylolysis, and patients with chronic inactive lysis can usually return to normal physical activities. However, acute stress fractures of the pars may unite with conservative measures, if detected early [26,27]. Conservative treatment typically involves cessation or reduction of sporting activities until bony union is achieved. In some cases a spinal brace may be used in treatment, although these are poorly tolerated. Conversely, delayed diagnosis and treatment is associated with non-union. Long-term complications may occur in up to a quarter of all patients with established spondylolysis, and these include chronic low back pain, spondylolisthesis and sciatica [18, 28, 29, 30, 31,32]. However, it is not clear if there are differences in the long-term morbidity of those patients with developmental defects versus those with spondylolysis acquired during adolescence as a result of a stress fracture. Longitudinal imaging studies are required to determine if any differences in outcome exist between the two groups.
The grading systems used in this study have previously been verified. The interobserver agreement for the morphological grading system has been shown to have good or excellent levels of agreement using the kappa statistic [17]. Similarly Hollenberg et al. also demonstrated high reliability coefficients for interobserver and intra-observer variation for their classification system [20].
The results from this study indicate that MRI is an accurate means of demonstrating the normal pars interarticularis (grade 0), acute complete defects (grade 3) and chronic established defects (grade 4). However, there appear to be some limitations in the ability to accurately diagnose stress reaction and incomplete defects.
There is a notable discordance between MRI and SPECT in the diagnosis of stress lesions of the pars in the absence of an actual defect or spondylolysis. It is interesting to observe that in four out of seven of the pars where marrow oedema was evident on MRI, and the SPECT image was normal, there was an association with a lysis on the contralateral side or at another level (Fig. 7). However, in all cases where SPECT was positive, and MRI normal, there was no association with lysis on the contralateral side or at other levels. This finding questions the significance of a positive SPECT scan, in the absence of any evidence of a fracture on CT, and whether this necessarily indicates the site of back pain. Positive SPECT scans have been reported to occur in non-painful sites in athletes [33], suggesting a physiological stress response and adaptation. It is not clear from this study why oedema should be present on MRI in the absence of a positive SPECT scan.
A unilateral spondylolytic defect with discordance between the MRI and SPECT of the contralateral pars. The SPECT ( A) shows unilateral uptake in the right L5 pars. The corresponding right parasagittal STIR ( B) and T1-W ( C) images show the presence of marrow oedema ( white arrow) and the spondylolytic defect ( black arrow). However, the parasagittal STIR image of the left-sided pars ( D) also demonstrates reactive marrow oedema ( open white arrow). CT ( E) confirms a right-sided unilateral defect
Incomplete fractures (grade 2) were also encountered in our study. This grade of spondylolysis has not previously been well described. Hollenberg et al. [20] utilised grade 2 to describe thinned, fragmented or irregular pars with marrow oedema. However, that study did not utilise sequences with slice thickness less than 3 mm, and it may be that some of these cases were indeed incomplete fractures. Even using 3D gradient echo sequences with a slice thickness of 1.9 mm, only four of ten incomplete fractures were correctly graded in our study. This may be due to partial volume effects, and improving coil technology may help to further reduce slice thickness, and improve delineation of incomplete fractures.
In this study, we have utilised a thin-section 3D gradient echo sequence, which is not a routine sequence for MRI examination of the lumbar spine, but it is a useful technique for evaluation of the pars interarticularis. In a previous pilot study, we found that only 192 of 290 (66%) of pars were confirmed intact on the sagittal 3 mm T1-W images using the presence of continuous marrow through the pars as a determining factor (grade I) [17]. However, 270 of 290 (93%) of pars were graded type I, when all pulse sequences, including the 3D sequence, were evaluated in combination. The number of pars graded as low signal or sclerotic (grade II), fell from 31% to 6% when all pulse sequences were evaluated. Similar figures were observed in this study, in which the CT provided a gold standard for confirmation of intact pars. Utilisation of multiplanar reconstruction has proved necessary only in the minority of pars.
While it has been argued that slice thickness less than 3 mm is not required, as nearly all sclerotic or low-signal pars will be intact [19], thicker slices will undoubtedly be less sensitive in demonstrating incomplete defects. We believe that it is important to distinguish between complete and incomplete fractures, because this may be a prognostic factor for healing. In our experience incomplete fractures frequently heal spontaneously, whereas there is a higher incidence of non-union for complete acute defects. Indeed, some cases of incomplete defects may represent pars fractures during a healing phase, rather than fractures in evolution.
Evaluation of dysplastic pars is also problematic. In this study, the false-positive and false-negative cases occurred in patients with morphological abnormalities of the pars, despite careful evaluation of the thin-slice 3D images. Furthermore, routine slice thickness of 3–4 mm may well lead to a greater incidence of indeterminate scans, which in turn may then require supplementary evaluation by other means such as CT. Although the MRI protocols are non-routine, the acquisition time of the scan sequences are comparable with standard protocols, and are generally well tolerated. Significant movement artifact was infrequently encountered, and no more than expected with a juvenile population.
A protocol with MRI as the first-line examination for adolescents with back pain is suggested from this study (Fig. 8), with targeted CT being performed in patients with acute defects or stress reaction, and in indeterminate cases. SPECT imaging may be abandoned, except where MRI is contraindicated or non-diagnostic due to poor patient compliance. If this protocol had been applied to the cohort of patients in this study, 54 of 71 (76%) patients would have had an MRI scan alone, with 41 of 71 (58%) diagnosed as negative for the presence of spondylolysis or stress reaction, and 10 of 71 (14%) diagnosed with chronic inactive spondylolysis. The remaining 17 patients (24%) would have had supplementary CT examination, and only in two cases would the examination have been negative. There would have been one false-positive diagnosis (1.5%) on MRI of a chronic defect, and one false-negative diagnosis. Other pathology would have also been identified by MRI, some of which may not have been demonstrated by other image modalities.
There are some limitations of this study. Evaluation of intra-observer and interobserver variation of each imaging method has not been performed. In construction of the overall grading, the indeterminate pars were considered as complete defects. The grading system by Hollenberg et al. [20] includes no provision for indeterminate cases. However, creating a further category makes the system unwieldy, and has no significant influence on the kappa score in this study. It is important not to assume that a pars is normal if the MRI grading is indeterminate, and from a practical viewpoint, in our protocol all indeterminate pars would have supplementary CT.
Similarly, we have combined grade I and grade II pars into one group for the comparative analyses. The only absolute determining factor for confirming intact pars on MRI is demonstration of continuous marrow throughout the pars interarticularis with an uninterrupted cortex. However, all grade II pars were also intact in this study. Saifuddin [15] described a variant of the type I pars with a thin, discrete sclerotic or low-signal line running across the pars in which a defect was present in some cases. However, this finding appears to occur rarely, at least in the juvenile population, and was not encountered in our series.
In order to obtain high-resolution images, it has been necessary to minimise slice thickness and field of view, while keeping a large matrix size. This will adversely affect the signal-to-noise ratio, but image quality was considered to be adequate. A previous study has demonstrated 93% of intact pars will be graded as type I using these protocols [17].
Finally, we have only evaluated juveniles and young adult patients. Therefore, it is not possible to conclude whether MRI is an accurate modality for diagnosis of pars defects in older age groups where the presence of facet osteoarthritis and hypertrophic new bone formation might obscure associated spondylolysis. We do not routinely employ the protocols described in this paper for all lumbar spine examinations, but confine its use to young patients with suspected spondylolysis.
Conclusions
The results of this study indicate that it is reasonable to utilise MRI as a first-line image modality for investigation of juvenile spondylolysis. MRI can effectively replace SPECT imaging in the majority of cases. Localised CT is recommended only for acute defects as a baseline for follow-up and for supplementary evaluation of indeterminate cases. Distinguishing between partial and incomplete fractures remains the challenge for MRI. Recognition of incomplete fractures depends on the identification of disruption of the inferior cortex of the pars interarticularis, in association with marrow oedema. Some cases of incomplete fractures have been accurately documented in this study using the 3D MRI sequence. However, more research is required to assess if the accuracy of MRI can be further improved in detection of incomplete fractures.
References
Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am 1984;66(5):699–707.
Wiltse LL, Widell EH Jr, Jackson DW. Fatigue fracture: the basic lesion is isthmic spondylolisthesis. J Bone Joint Surg Am 1975;57(1):17–22.
Rosenberg NJ, Bargar WL, Friedman B. The incidence of spondylolysis and spondylolisthesis in non-ambulatory patients. Spine 1981;6:35–37.
Wiltse LL, Newman PH, Macnab I. Classification of spondylolisis and spondylolisthesis. Clin Orthop 1976 (117):23–29.
Collier BD, Johnson RP, Carrera GF, et al. Painful spondylolysis or spondylolisthesis studied by radiography and single-photon emission computed tomography. Radiology 1985;154:207–211.
Gundry CR, Fritts HM Jr. MR imaging of the spine in sports injuries. Magn Reson Imaging Clin N Am 1999;7(1):85–103.
Libson E, Bloom RA. Anteroposterior angulated view. A new radiographic technique for the evaluation of spondylolysis. Radiology 1983;149:315–316.
Libson E, Bloom RA, Dinari G, et al. Oblique lumbar spine radiographs: importance in young patients. Radiology 1984;161:98–90.
Papanicolaou N, Wilkinson RH, Emans JB, Treves S, Micheli LJ. Bone scintigraphy and radiography in young athletes with low back pain. AJR Am J Roentgenol 1985;145:1039–1044.
Pennell RG, Maurer AH, Bonakdarpour A. Stress injuries of the pars interarticularis: radiologic classification and indications for scintigraphy. AJR Am J Roentgenol 1985;145:763–766.
Grogan JP, Hemminghytt S, Williams AL, et al. Spondylolysis with computed tomography. Radiology 1982;145:763–742.
Langston JW, Gavant ML. “Incomplete ring” sign: a simple method for CT detection of spondylolysis. J Comput Assist Tomogr 1985;9:726–729.
Rothman SLG, Glenn WV. CT multiplanar reconstruction in 253 cases of lumbar spondylolysis. AJNR Am J Neuroradiol 1984;5:81–90.
Teplick JG, Laffey PA, Berman A, et al. Diagnosis and evaluation of spondylolisthesis and/or spondylolysis on axial CT. AJNR Am J Neuroradiol 1986;7:479–491.
Saifuddin A, Burnett SJ. The value of lumbar spine MRI in the assessment of the pars interarticularis. Clin Radiol 1997;52(9):666–671.
Johnson DW, Farnum GN, Latchaw RE, Erba SM. MR imaging of the pars interarticularis. AJR Am J Roentgenol 1989;152(2):327–332.
Campbell RS, Grainger AJ. Optimization of MRI pulse sequences to visualize the normal pars interarticularis. Clin Radiol 1999;54(1):63–68.
Ulmer JL, Elster AD, Mathews VP, Allen AM. Lumbar spondylolysis: reactive marrow changes seen in adjacent pedicles on MR images. AJR Am J Roentgenol 1995;164(2):429–433.
Udeshi UL, Reeves D. Routine thin slice MRI effectively demonstrates the lumbar pars interarticularis. Clin Radiol 1999;54(9):615–619.
Hollenberg GM, Beattie PF, Meyers SP, Weinberg EP, Adams MJ. Stress reactions of the lumbar pars interarticularis: the development of a new MRI classification system. Spine 2002;27(2):181–186.
Altman DG. Practical statistics for medical research. In: London: Chapman and Hall; 1991. p. 403–409.
Beutler WJ, Fredrickson BE, Murtland A, Sweeney CA, Grant WD, Baker D. The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Spine 2003;28(10):1027–1035; discussion 1035.
Grenier N, Kressel HY, Schiebler ML, Grossman RI. Isthmic spondylolysis of the lumbar spine: MR imaging at 1.5 T. Radiology 1989;170(2):489–493.
Heitoff KB, Gundry CR, Burton CV, et al. Juvenile discogenic disease. Spine 1994;19:335–340.
Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 1994;331(2):69–73.
Micheli LJ, Wood R. Back pain in young athletes. Significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med 1995;149(1):15–18.
Ralston S, Weir M. Suspecting lumbar spondylolysis in adolescent low back pain. Clin Pediatr (Phila) 1998;37(5):287–293.
Watkins RG, Dillin WH. Lumbar spine injury in the athlete. Clin Sports Med 1990;9:419–448.
Steiner ME, Micheli LJ. Treatment of symptomatic spondylolysis and spondylolisthesis with the modified Boston brace. Spine 1985;10:937–943.
Blanda J, Bethem D, Moats W, Lew M. Defects of the pars interarticularis in athletes: a protocol for non-operative treatment. J Spinal Disord 1993;6:406–411.
Wiltse LL. The effect of the common anomalies of the lumbar spine upon disk degeneration and low back pain. Orthop Clin North Am 1971;2:569–582.
Rauch RA, Jinkins JR. Lumbosacral spondylolisthesis associated with spondylolysis. Neuroimaging Clin N Am 1993;3:543–555.
Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, Macintyre JG. Scintigraphic uptake of 99mTc at non-painful sites in athletes with stress fractures: the concept of bone strain. Sports Med 1987;4:65–75.
Acknowledgements
The authors would like to gratefully thank all the radiography staff in MRI and CT and the technicians in nuclear medicine for their enduring support during this study. Many thanks
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Campbell, R.S.D., Grainger, A.J., Hide, I.G. et al. Juvenile spondylolysis: a comparative analysis of CT, SPECT and MRI. Skeletal Radiol 34, 63–73 (2005). https://doi.org/10.1007/s00256-004-0878-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-004-0878-3