Abstract
Objective
To try to define an association between clinical history and the finding of isolated teres minor denervation on routine magnetic resonance (MR) examination of the shoulder.
Design
A retrospective review of all shoulder MR examinations performed at our institution over a 2-year period (n=2,563)
Patients
All patients and MR examinations demonstrating isolated denervation of the teres minor muscle as determined by review of this subset of patients (n=61)
Results
A 3% incidence of isolated teres minor denervation was found. No patient had a clinical history concerning the classic quadrilateral space syndrome, and no patient had a structural lesion in the quadrilateral space.
Conclusions
Isolated teres minor denervation is not an uncommon finding on routine shoulder MR imaging and may be associated with pathology other than a structural lesion in and about the axillary neurovascular structures, such as rotator cuff injuries and traction injury on the axillary nerve sustained during a glenohumeral joint translational event.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The finding of isolated teres minor denervation on magnetic resonance (MR) imaging examinations of the shoulder had, until recently, been considered by some to be highly suggestive of the “quadrilateral space syndrome;” however, as other authors have anecdotally observed, it is encountered not infrequently during routine MR examinations of the shoulder and apparently in patients who have no such clinical signs or symptoms suggestive of this diagnosis [1]. Cahill and Palmer first described quadrilateral space syndrome in which the neurovascular bundle, comprised of the posterior humeral circumflex artery and axillary nerve, may be compressed by fibrous bands [2]. The diagnosis has traditionally been based on clinical presentation with angiographic confirmation demonstrating fibrous adhesions about the posterior humeral circumflex artery [3]. Treatment is usually conservative, though reports of patients requiring surgical decompression of the fibrous tissue have been reported [4]. The purpose of our study was to evaluate other possible etiologies and the potential clinical relevance of isolated denervation of the teres minor muscle.
Materials and methods
Of the 2,563 shoulder MR examinations performed at our institution over a 2-year period, 8% (n=210) of patients were found to have denervation of one or more of the muscles about the shoulder. Sixty-six (3%) patients had isolated denervation of the teres minor and were therefore included in the review. Five patients were excluded secondary to confounding medical or surgical conditions or other clear structural cause for the denervation [bony exostosis compressing the axillary nerve following above-the-elbow amputation (n=1), posttraumatic heterotopic ossification compressing the axillary nerve after a fracture (n=1), distended pseudocapsule compressing the neurovascular bundle following shoulder hemiarthroplasty (n=1), posttraumatic brachial plexus neuroma (n=1), and global neuropathy from polio infection (n=1)], leaving 61 patients (65 shoulders) for review. Only one patient had undergone electrophysiologic testing. All patients in our study initially presented for treatment to orthopedic surgeons and sports medicine physicians who assessed the patients and ordered MR imaging of the shoulder.
All shoulder imaging was performed on a 1.5 T superconducting magnet (Horizon LX, GE Medical Systems, Milwaukee, WI, USA) using a phased-array shoulder coil (shoulder PA coil, Med Rad, Indianola, PA, USA). Sequences included oblique coronal fast spin echo sequence in the plane of the long axis of the scapula, repetition time (TR)/echo time (TE) 4000/34 (effective), slice thickness 3 mm, no interslice gap, FOV 16 cm, matrix 512×384, 2 NEX, echo train length 9–14; oblique coronal with frequency-selective fat suppression (Chemsat, General Electric Medical Systems, Milwaukee, WI, USA), TR/TE 4000/80 (effective), slice thickness 3 mm with no interslice gap, FOV 16 cm, 256x224 matrix, 2 NEX, ETL 8–10; oblique sagittal FSE, TR/TE 3500–4000/34 (effective), 4 mm slice thickness, skip 0.5 mm, FOV 16 cm, 512×224, 2 NEX; and axial FSE TR/TE 4000/34 (effective), slice thickness 3.5 mm with no interslice gap, FOV 15–16 cm, 512×384 matrix, 2 NEX, ETL 8.
Muscle denervation was diagnosed using established MR criteria [5, 6]. These include:
-
1.
In the acute stage: high signal intensity on fat-suppressed T2-weighted sequences within the muscle of the teres minor without fatty infiltration or loss of muscle bulk
-
2.
In the subacute stage: mixed edema and fatty infiltration
-
3.
In the chronic stage: diffuse fatty infiltration with loss of muscle bulk.
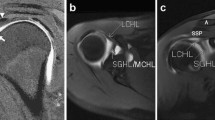
Denervation was also graded as mild, moderate and severe, depending on the degree of loss of muscle bulk and fatty infiltration (Figs. 1, 2, 3) MR images were reviewed independently by two musculoskeletal radiologists. Associated findings, such as rotator cuff tears, capsular injury, and labral pathology, were recorded. Clinical findings were also reviewed. Data such as clinical presentation as well as physical examination findings were recorded. The presence of neurological symptoms such as pain over the quadrilateral space and anterior aspect of the shoulder, as well as paresthesias in the arm and/or forearm with a nondermatomal distribution were recorded if present.
Axial fast spin echo proton density weighted image demonstrating moderate atrophy of the teres minor muscle (arrow). There is more extensive fatty replacement of the muscle fibers and loss of muscle bulk compared with Fig. 1. Note also the advanced glenohumeral joint arthrosis and full thickness cartilage loss over the glenoid and preferential posterior glenohumeral joint space narrowing
Results
All 61 patients with teres minor denervation had a normal deltoid on MR images. Associated findings on shoulder MR imaging included a tear of at least one of the tendons of the rotator cuff (n=47), glenohumeral joint capsular injury (n=14), anterior (n=14) or posterior (n=31) labral tears or evidence of recent glenohumeral joint dislocation with a Bankart lesion (n=4), and moderate-to-severe glenohumeral joint arthrosis (n=29). Detailed clinical data were available on 51% (n=31) of patients. Of these, nine had undergone prior shoulder surgery. Specifically, patients underwent total shoulder arthroplasty (n=1), hemiarthroplasty (n=1), anterior capsular shift (n=1), rotator cuff (n=4), and labral repair (n=2). There were no patients who had clinical signs or symptoms indicative of quadrilateral space syndrome. No patient had a structural lesion in the quadrilateral space or evidence for fibrous adhesions about the axillary nerve or posterior circumflex humeral artery on MR examination.
Clinical history of many patients included a history of shoulder injury, with athletic injuries frequently reported. Activities including weight lifting and heavy lifting were noted in six patients. Specifically, a history of regular weight lifting was noted in three patients. Two patients reported lifting a heavy object, and one patient reported both a history of regular weight lifting as well as carrying heavy objects. History of shoulder dislocation was reported in four patients, with a questionable history of dislocation reported in another patient. Nine patients reported a history of fall leading to their shoulder pain, with one patient reporting two falls. Specific sporting activities were reported in some falls, with three patients reporting a history of fall while skiing and one patient while diving. Occupations of patients included dentistry (n=1), violinist (n=1), welder/iron worker (n=1), and lifeguard (n=1).
Physical examination findings included normal neurological exam in all patients except for three. One patient with was found to have numbness and tingling in the ulnar and median nerve distributions, felt to be possibly secondary to a plexus injury; one patient had numbness and tingling in the shoulder; and one patient had numbness in the forearm. One patient also reported pain in the forearm, though no neurological deficits were noted.
Only one patient underwent electrophysiologic testing, which showed chronic neurogenic changes in the middle and posterior heads of the deltoid and reduced recruitment on submaximal effort. It did not include detailed electromyographic testing of the teres minor or cervical paraspinal muscles. Therefore, this study failed to rule out a cervical radiculopathy responsible for the observed teres minor denervation.
Discussion
The teres minor is considered to be both an external rotator of the humerus and a stabilizer of the glenohumeral joint. The etiology of the observed loss of function in isolated teres minor denervation and its effect on shoulder function has not been described. Atypical shoulder pain secondary to nerve injury may often represent a diagnostic challenge. The lack of a clear diagnosis can result in inappropriate treatment and therefore potentially prolonged disability [7]. The goal of our study was to highlight the incidence of isolated teres minor denervation and to correlate clinical and MR data.
The anatomic course of the branch of the axillary nerve to the teres minor can help to explain its occasional selective injury. The axillary nerve arises from the cervical cord, comprised of the fifth and sixth cervical nerve roots, and subsequently directly as a branch of the posterior cord of the brachial plexus [8]. It descends inferolaterally, anterior to the subscapularis muscle, passes through the quadrilateral space (teres minor superiorly, teres major inferiorly, long head of the triceps medially, and the humeral neck laterally) at the inferior border of the subscapularis. The axially nerve then gives off branches to the deltoid muscle, teres minor muscle, superior lateral brachial cutaneous nerve, and also supplies the shoulder. Specifically, at the posterosuperior border of the quadrilateral space or the inferior border of the teres minor, the axillary nerve is divided into the posterior and anterior branches. The posterior branch then supplies the teres minor muscle and superior lateral brachial cutaneous nerve [9]. The posterior branch may also supply the posterior deltoid. Selective injury to the axillary nerve supplying the teres minor may occur due to its relatively superficial position and/or many smaller posterior branches [9].
Selective teres minor denervation may occur in the quadrilateral space syndrome in which the axillary nerve is compressed or otherwise affected by a structural lesion in the quadrilateral space. While this diagnosis may be fairly straightforward when an obvious structural lesion such as fibrous bands or other mass is found, it may be more challenging when these findings are not present on diagnostic imaging studies, such as in the series of cases presented here. In these cases, other etiologies are postulated.
Prior surgical intervention, trauma, or chronic irritation of the axillary nerve between the muscles of the rotator cuff may be responsible for axillary nerve-root injury. Several patients in our series had prior surgical intervention. The close proximity of the axillary nerve to posterior surgical arthroscopic portals has been described, with both the Bankart procedure and inferior capsular shift procedures reported to be associated with axillary nerve injury [8, 10]. Capsular thermoplication may result in marked thickening of the joint capsule, including the axillary recess, possibly injuring the axillary nerve supplying the teres minor where it lies in close approximation to the posteroinferior capsule.
Acute translational events such as a glenohumeral joint subluxation or dislocation may selectively injure the axillary nerve branch to the teres minor. The relatively fixed position of the quadrilateral space may make it particularly susceptible to injury during such a subluxation event [7]. Several patients in our series had evidence of a subacute or remote translational event with remodeling or frank disruption of the capsule with or without concomitant labral tear.
Chronic irritation of the axillary nerve between muscle bellies of the rotator cuff can occur in throwing athletes in the extremes of joint motion [11]. Increased nerve friction may occur during shoulder movement close to the long head of the triceps resulting in nerve swelling [12]. Cadaveric examinations of the shoulder have demonstrated marked perineural thickening, decreased nerve fiber number, and myxoid globular degeneration in the endoneurium noted at the bifurcation into the teres minor in elderly patients, suggesting that chronic traction and irritation of the nerve over time may contribute to its injury [13].
The specific mechanism of axillary nerve injury resulting in selective teres minor denervation may often be unclear; however, MR imaging as well as detailed electromyographic testing can be useful in isolating the specific location of nerve injury. The coupling of both imaging and electrodiagnostic testing can be extremely useful in characterizing neurogenic edema and denervation in the shoulder [14]. Electromyographic studies may also identify denervation of other muscles that may not be detected on MR. Bredella et al. report the results of five patients with denervation syndromes of the shoulder undergoing MR imaging and electrophysiologic studies and found that both tests contributed important clinical information [14]. In their series, for example, one patient had fatty atrophy of the teres minor muscle caused by an axillary nerve cyst, with electrophysiologic findings of an axillary nerve block. While electrophysiologic studies were not performed in the majority of our patients, we feel that electrophysiologic studies would have significantly assisted in characterizing the nerve injury responsible for isolated teres minor denervation. Furthermore, electrodiagnostics may have demonstrated denervation of other muscles (albeit to a lesser extent) not seen on MR imaging, suggesting another cervical root or brachial plexus injury. In the one electrophysiologic study performed in our series, there were no axillary nerve conduction studies performed nor were there any electromyographic assessment of the teres minor muscle, despite chronic neurogenic changes found in the deltoid muscle and the denervation in the teres minor seen on MR imaging.
There were several limitations in our study. Clinical data were available on only 50% of patients, limiting our ability to completely correlate clinical and imaging data. It is possible that patients did not report accurate histories of shoulder injury or trauma to their physicians in instances where these injuries took place several years prior. Furthermore, since electrophysiologic studies were not performed in the vast majority of patients, an underlying cervical radiculopathy or brachial plexopathy with preferential involvement of the teres minor, although unlikely, cannot be completely ruled out.
In conclusion, we have found that isolated teres minor denervation occurs not infrequently in approximately 3% of patients undergoing routine shoulder MR imaging. The pathophysiology of the denervation is not totally clear, but prior surgical intervention, a history of trauma such as an anterior glenohumeral joint translational event, or altered biomechanics from chronic rotator cuff insufficiency, may play a role.
References
Linker CS, Helms CA, Fritz RC. Quadrilateral space syndrome: findings at MR imaging. Radiology 1993; 188:675–676
Cahill BR, Palmer RE. Quadrilateral space syndrome. J Hand Surg 1983; 8:65–69
Chautems RC, Glauser T, Waeber-Fey MC, Rostan O, Barraud GE. Quadrilateral space syndrome: case report and review of the literature. Ann Vasc Surg 2000; 14:673–676
Lester B, Jeong GK, Weiland AJ, Wickiewicz TL. Quadrilateral space syndrome: diagnosis, pathology and treatment. Am J Orthop 1999; 28(12): 718–725
Fleckenstein JL, Watumull D, Conner KE, Ezaki M, Greenlee Jr RG, Bryan WW, Chason DP, Parkey RW, Peshock RM, Purdy PD. Denervated human skeletal muscle: MR imaging evaluation. Radiology 1993; 187:213–218
Uetani M, Hayashi K, Matsunaga N, Imamura K, Ito N. Denervated skeletal muscle: MR imaging; work in progress. Radiology 1993; 189:511–515
McIlveen SJ, Duralde XA, D’Alessandro DF, Bigliani LU. Isolated nerve injuries about the shoulder. Clin Orthop 1994; 306:54–63
Perlmutter GS. Axillary nerve injury. Clin Orthop 1999; 368:28–36
Zhao X, Hung LK, Zhang GM, Lao J. Applied anatomy of the axillary nerve for selective neurotization of the deltoid muscle. Clin Orthop 2001; 390:244–251
Bryan WJ, Schauder K, Tullos HS. The axillary nerve and its relationship to common sports medicine procedures. Am J Sports Med 1986; 14(2):113–116
Francel TJ, Dellon AL, Campbell JN. Quadrilateral space syndrome: diagnosis and operative decompression technique. Plastic Recon Surg 1991; 87(5):911–916
Gitlin G. Concerning the gangliform enlargement (“pseudoganglion”) of the nerve to the teres minor muscle. J Anat 1957; 57:466–470
Hashimoto T, Hamada T, Nakamura T, Sasaguiri Y, Suzuki K. Myxoid and globular degeneration of nerves in the shoulder joint. Clin Orthop 1995; 320:55–64
Bredella MA, Tirman PFJ, Fritz RC, Wischer TK, Stork A, Genant HK. Denervation syndromes of the shoulder girdle: MR imaging with electrophysiologic correlation. Skeletal Radiol 1999; 28:567–572
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sofka, C.M., Lin, J., Feinberg, J. et al. Teres minor denervation on routine magnetic resonance imaging of the shoulder. Skeletal Radiol 33, 514–518 (2004). https://doi.org/10.1007/s00256-004-0809-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-004-0809-3