Abstract
The SAPHO syndrome was a term coined to include a variety of musculoskeletal disorders associated with skin conditions, mainly palmoplantar pustulosis and acne conglobata. It is more correctly a spectrum which includes the following: skin lesions, osteoarticular manifestations of synovitis hyperostosis and osteitis affecting particular target sites, and·a clinical course marked by relapses and remissions. The major sites of involvement are the anterior chest wall, the spine, long bones, flat bones, and large and small joints. The distribution and severity of involvement varies from the adult to the pediatric form of chronic recurrent multifocal osteomyelitis (CRMO). The diagnosis of SAPHO syndrome is not difficult when the typical osteoarticular lesions are located in characteristic target sites. The diagnosis is more difficult if atypical sites are involved and there is no skin disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The association of musculoskeletal disorders with acne conglobata was first noted in 1961 [1]. The entity of chronic recurrent multifocal osteomyelitis (CRMO) was described in 1972 [2] and the association between some cases of CRMO and palmoplantar pustulosis was noted in 1978 [3]. Subsequently a wide variety of clinical and radiological manifestations associated with skin conditions and osteoarticular disorders appeared in the literature with up to 50 different names, including pustulotic arthro-osteitis, sternocostoclavicular hyperostosis and acne-associated spondyloarthropathy.
In 1987 Chamot et al. [4], in a review of 85 cases, first described "le syndrome acne pustulose hyperostose osteite" and coined the acronym SAPHO. The subsequent alteration of the designation for the first initial of the acronym from syndrome to synovitis [5] highlights what has been perceived by some as the inappropriateness of the acronym to describe a syndrome. Other authors have subsequently proposed that it be considered as a spectrum or concept [6, 7, 8, 9, 10] to include several idiopathic disorders which share the same clinical, radiological and pathological characteristics. This thesis is supported by the fact that not all the components can coexist, i.e. acne and pustulosis.
The fundamental component of the SAPHO spectrum is an inflammatory osteitis, which may or may not be associated with dermatological components usually with negative bacterial cultures [11]. The main target area is the anterior chest wall, with lesser involvement of the spine and peripheral skeleton.
Clinical and biological features
The spectrum of SAPHO and CRMO includes the following:
Skin lesions
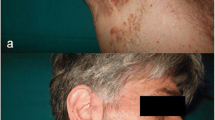
The skin diseases which are typically seen are palmoplantar pustulosis (PPP) and acne. PPP is a chronic eruption of yellowish intradermal sterile pustules on the palms and soles (Fig. 1). Acne is usually of the severe form (acne fulminans; acne conglobata; hidradenitis suppurativa) (Fig. 2). The prevalence of bone lesions in patients with PPP ranges from 10% to 33% [7, 8, 9, 12]. On the other hand the incidence of PPP and acne in patients with the SAPHO spectrum has been reported as 55.7% and 18.3% respectively [11]. Most series report 60% skin involvement [7]; however, an incidence as low as 20% has been described [13, 14]. The absence of skin manifestations does not exclude the SAPHO spectrum. Skin lesions may precede, occur simultaneously with, or follow the onset of osteoarticular manifestations [11]. In most cases the interval between the onset of skin and osteoarticular lesions is less than 2 years [10] but intervals as long as 20 and 38 years have been recorded [11, 15].
Various patterns of psoriasis can also be associated with the SAPHO syndrome, especially pustular psoriasis. It can be difficult to differentiate this type of psoriasis from PPP [11]. It has been reported that approximately two thirds of patients with sternocostoclavicular hyperostosis also will experience characteristic skin conditions, including psoriasis vulgaris [10].
Osteoarticular lesions
The osteoarticular manifestations include synovitis, hyperostosis and osteitis. Hyperostosis and osteitis are manifestations of a chronic inflammatory reaction involving both the cortex and the medullary canal with associated endosteal and periosteal thickening. This results in diffuse cortical thickening and narrowing of the medullary canal with or without areas of osteolysis. Bone sclerosis may be homogeneous but may also include areas of osteolysis within it [16]. Inflammatory enthesopathy is also a feature [7, 17].
Involvement of particular target sites
The pattern of osteoarticular involvement is age-dependent. Synovitis in adults affects the joints of the anterior chest wall, the sacroiliac joints and, to a lesser extent, peripheral joints in the form of a mono- or polyarthritis.
Hyperostosis in adults predominantly involves the anterior chest wall but also can present as an unusual form of spondylodiscitis and more rarely involve the pelvis or long bones.
CRMO is the manifestation of the SAPHO spectrum seen in children and young adults with a predilection for the anterior chest wall, particularly the clavicle, with multiple and sometimes symmetrical lesions involving the metaphyses of long bones [2, 3, 18].
Osteoarticular lesions with non-specific histopathology
In the early stages of the SAPHO spectrum the changes are indistinguishable from those of osteomyelitis. The intermediate stage is characterised by an infiltrate composed of mononuclear cells, whilst enlarged and sclerotic trabeculae together with increased marrow fibrosis develop in the later stage [13, 14].
A chronic clinical course marked by relapses and remissions
The clinical course of the SAPHO spectrum varies greatly from patient to patient. Some experience only one or two rheumatological flares, during prolonged follow-up. Others suffer continuously from arthritis or osteitis, frequently with additional sites of inflammation over time. In fact, most patients experience pain, soft tissue swelling, and limitation of motion referable to the involved skeletal sites [7, 11].
Systemic manifestations are unusual, but fever is sometimes encountered. Routine blood testing indicates the existence of an inflammatory reaction with modestly elevated erythrocyte sedimentation rates and C-reactive protein values.
There is a variable age of presentation. CRMO is seen in children and adolescents [18] whilst the SAPHO spectrum is a disease of young adults [11]. There tends to be a female preponderance in both CRMO and SAPHO [11, 18)].
Radiological features
One or more skeletal sites can be involved. When multiple, the lesions can occur either simultaneously or successively. In fact, the distribution of the disease depends on the age of the patient. In young or in middle-aged adults the disease predominates in the sternocostoclavicular region followed by the spine, pelvis and long bones. In children, the disease predominates in the long bones followed by the clavicle and the spine. In both populations, the radiological features are dominated by hyperostosis and osteitis. The radiological features are those of synovitis, arthritis and chronic inflammatory bone disease.
Adults
Anterior chest wall lesions
In adults, the sternocostoclavicular region is the most frequent site of the disease (65–90% of patients). All the components of the anterior chest wall can be involved, particularly the sternoclavicular (SCJ), upper costosternal (CSJ), costochondral (CCJ) and manubriosternal (MSJ) junctions. This region often demonstrates characteristic radiological features. Three stages of involvement have been described [19]. Stage 1 is localised to the region of the costoclavicular ligament and may be a primary enthesopathy (Fig. 3). It can be demonstrated on CT as a soft tissue mass with evidence of new bone. Stage 2 evolves with the development of an arthropathy in the sternoclavicular joint (Fig. 4A) and sclerosis (Fig. 4B) involving the medial end of the clavicle; the first rib and the adjacent sternum with sclerotic hypertrophy of the costal cartilage (Fig. 5). Stage 3 is a continuum with osteosclerosis, hyperostosis and bone hypertrophy affecting the medial ends of the clavicles, the sternum and upper ribs with arthritis in the adjacent joints. There may be isolated involvement of the clavicle (Fig. 6) and sternum [16].
Axial CT scans through the SCJs showing stage 2 involvement with: A, B sclerosis of the medial end of the right clavicle; B arthropathy of the sternoclavicular joint; and C sclerosis of the first costal cartilage and adjacent manubrium. Coronal MR images show capsular thickening on T1-weighted images (D); marrow oedema on T2-weighted images (E) with contrast enhancement (F)
Osteitis presents usually as osteosclerosis with a homogeneous fibrillary pattern [11]. Hyperostosis, which is highly characteristic of SAPHO, is characterised by a chronic periosteal reaction and cortical thickening leading to bone hypertrophy. There may be an associated enthesopathy leading to ligamentous ossification, and bony bridges between ribs and across joints (SCJ, CCJ and MSJ) [7, 20] (Fig. 7). Joint erosions (Fig. 8) involving the adjacent articulations are frequently seen as a result of a primary arthritis or an extension of the adjacent osteitis. They frequently lead to ankylosis particularly of the sternocostal and costoclavicular junctions (Fig. 9).
There is usually involvement of the soft tissues immediately adjacent to the involved bones and joints (Fig. 10). Histological examination shows this to be a non-specific chronic inflammatory change. It may be quite extensive and can be mistaken for tumour or lymphadenopathy (Fig. 11). There may be resulting compression and thrombosis of adjacent veins [21].
Nuclear medicine is extremely sensitive in the detection of anterior chest wall lesions. The "bull's head" pattern of increased activity (Fig. 12) is a highly specific sign and may obviate the need for biopsy [8]. CT scanning is the optimal modality to demonstrate the osteoarticular lesions. Targeted scans, particularly with multislice CT and reformatted images, will accurately demonstrate the extent of involvement of the anterior chest wall. Enhanced CT will demonstrate the soft tissue involvement. MR imaging will demonstrate the changes due to arthritis and bone marrow oedema utilising fat-suppressed T2-weighted or STIR sequences (Fig. 5); however, erosions and bony sclerosis are not well displayed. MR imaging may, however, be useful in follow-up of patients to differentiate active from chronic lesions (Fig. 13).
Spine
The spine is the second most common site of disease in adults being involved in 33% of cases [11, 17, 22, 23]. The lesions are usually segmental. The thoracic spine is most frequently affected followed by the lumbar and cervical spine. Several segments (up to four) may be affected [22]. There are four main radiographic manifestations:
Non-specific spondylodiscitis
This may be the initial manifestation of SAPHO [24]. Erosive lesions tend to affect the inferior vertebral end plates with focal lesions being either adjacent to the end plates or at the corners of the vertebral bodies [12]. Radiographs and reformatted CT images reveal irregularity and erosions with sclerosis of the end plates and narrowing and often complete obliteration of the adjacent discs (Fig. 14A). Active lesions may show only mild uptake on a bone scan [22]. MR imaging provides better definition of the extent of the inflammatory process in relation to the bone marrow and the intervertebral disc (Fig. 14B) and allows differentiation of the SAPHO spectrum from infectious spondylodiscitis. Active lesions are demonstrated as either focal or diffuse hypointense lesions on T1-weighted gadolinium-enhanced scans and hyperintense on T2-weighted images (Figs. 14, 16). There may be a diffuse pattern of abnormal signal intensity in the marrow with involvement of the posterior elements with low signal intensity on T1-weighted and increased signal intensity on T2-weighted images. However, abscesses and epiduritis are not seen and the adjacent intervertebral disc usually demonstrates at least some focal areas with low signal intensity on T2-weighted images.
Osteosclerosis of one or more vertebral bodies
Histopathology shows inflammatory changes in the vertebral body and not in the disc spaces (Fig. 15A) [20]. Sclerotic reactive changes are initially seen in association with erosive lesions in the end plates. In chronic cases osteosclerosis may be diffuse, particularly when associated with ankylosis(Fig. 15B).
A Lateral tomogram showing uniform sclerosis of the body of T4 in an 18-year-old male. B Sagittal reformatted CT image 17 years later shows involvement of four segments with ankylosis of the intervertebral discs and active disease at the level below. C Sagittal T2-weighted MR image showing high signal intensity in the posterior aspects of the T7 and T8 vertebral bodies with low signal intensity in the intervening disc. D T1-weighted axial images at the T8 level show symmetrical paravertebral fatty masses
Paravertebral ossifications
Diffuse paravertebral ossifications may be encountered. They include marginal syndesmophytes but most frequently they are non-marginal asymmetrical paravertebral ossifications which are similar to, but not the same as, the syndesmophytes encountered in psoriatic arthropathy [10]. Hyperostosis with massive bridging along the anterior aspect of the spine may be seen in chronic cases (Fig. 16) [24] and may be accompanied by ankylosis of the disc spaces and associated kyphosis [22] (Fig. 15). These changes are well demonstrated on multi-slice CT with reformatted images and can be also seen on MR imaging. Paravertebral fatty masses may develop as well. These are usually symmetrical and hyperintense on T1-weighted imaging (Fig. 15D).
Sacroiliac joint involvement
The sacroiliac joints are involved in 13–52% of cases [11, 17, 22]. Sacroiliitis is frequently unilateral [4, 10]. Unilateral involvement is more frequently seen than in ankylosing spondylitis [16]. CT may show unusual sclerosis and hyperostosis predominantly on the iliac side of the joint which may extend further into the iliac bone.(Fig. 17) The association between a moderate form of sacroiliitis and extensive osteosclerosis of the adjacent iliac bone is highly suggestive of the SAPHO spectrum.
Long bones
Involvement of the long bones occurs in approximately 30% of patients. The disease predominantly affects the metadiaphyseal regions of the distal femur and proximal tibia, but the fibula, humerus, radius and ulna can also be involved. On plain film, the lesions are characterised by osteosclerosis with thickening of the trabeculae and cortices and periosteal new bone formation, usually with enlargement of the bone (Fig. 18). The medullary canal may be narrowed. Except for the sequestra and abscess formation, which are not present in the SAPHO spectrum, these features are those of a chronic osteomyelitis. However, especially at an early stage, the lesion may appear more aggressive, with areas of osteolysis. Isolated periostitis of long bones has also been described but represents an unusual feature of the SAPHO spectrum (Fig. 19).
Flat bones
The ilium and the mandible may be involved in up to 10% of cases [11]. Sclerosis of the ilium is usually associated with sacroiliac joint involvement (Fig. 17). There may be diffuse sclerosis involving the mandible, particularly the cancellous bone, with an extensive organised periosteal reaction (Fig. 20) [25]. There may be an extension to the adjacent temporomandibular joint.
Peripheral arthritis
Arthritis has been reported in up to 92% of cases [11] with axial involvement in 91% of cases and peripheral joint involvement in 36% of cases [11]. Joint destruction is a rare feature. The knees, hips and ankles are the most frequently involved joints (Fig. 21) but small joints of the hands and feet can also be involved (Fig. 22) [26, 27]. Radiographic features of the acute phase of the disease include changes due to asymmetrical synovial inflammation with juxta-articular osteoporosis [28]. Advanced cases may show joint space narrowing with marginal or central erosions (Fig. 23). The changes can exceptionally be followed by ankylosis (Fig. 24) hyperostosis and enthesopathy.
Children
In children the disease usually presents as CRMO. There is a predilection for the metaphyses of long bones usually in the lower extremity (tibia, femur, fibula) followed by the clavicles and the spine [21]. Asymmetrical involvement of the sacroiliac joints may occur (Fig. 25). Although involvement of the pelvic bones and peripheral joints is usually not encountered in children, there may be involvement of the carpus (Fig. 26A) and tarsus. The lesions are often multiple and sometimes symmetrical [2] but the disease may manifest itself at a single site [29].
Long bones
In tubular bones, osteolysis is sometimes observed, especially at the beginning of the disease, and usually involves the metaphyseal bone adjacent to the growth plate (Fig. 26B). However, this is rapidly followed by progressive sclerosis and radiographs most frequently demonstrate association of both osteolytic and osteoproliferative changes. Periosteal reaction is minimal, if present at all (Fig. 27). Concomitant involvement of the epiphyseal bone is a rare finding and premature closure of the growth plate has exceptionally been reported [11]. MR imaging is useful in assessing the extent and activity of such lesions (Fig. 28). It usually reveals more pronounced involvement of the bone marrow which is not evident on conventional radiography. During the active phase, bone marrow involvement is manifested as decreased signal intensity on T1-weighted images with scattered foci of increased signal intensity on T2-weighted images.
Frequently, associated soft tissue swelling is evident but there is no abscess formation. These changes heal with sclerosis during quiet periods, resulting in progressive hyperostosis and sclerosis of the metadiaphyseal bone.
Clavicles
The radiographic features of lesions in the clavicle in the early stage are characteristically lytic medullary destruction involving the medial end. Periosteal reaction may be profuse with an onion-skin appearance resembling malignancy (Fig. 29) but without sequestra. The signal intensity on MR imaging, which is increased on T1-weighted images and decreased on T2-weighted images, is non-specific. MR imaging will demonstrate the surrounding soft tissue oedema, which may be profound (Fig. 30) but there is no abscess formation. The course of the disease usually consists of several exacerbations during which further medullary destruction and periosteal new bone may occur with evidence of healing with sclerosis. MR imaging is also useful for identifying relapses. Quiescent lesions will show as decreased signal intensity on T1- and T2-weighted images with increased signal intensity in focal areas during exacerbations. There is progressive hyperostosis and sclerosis of the clavicle over a period of time with or without expansion (Fig. 30C) and small lucent areas. This may gradually extend laterally and even involve the outer ends. In contrast to the adult disease, the sternoclavicular joint, sternum and ribs are rarely involved and ligamentous ossification and bony bridging across the sternocostoclavicular joint is not a feature.
Axial CT scan of the right clavicle of a 2-year-old female showing extensive sclerosis of the clavicle and an organised periosteal reaction. B Axial T2-weighted MR image shows extensive marrow and soft tissue oedema related to the mid-shaft of the clavicle. C AP radiograph shows subsequent marked expansion of the medial shaft with sclerosis
Spine
Involvement of the spine can present as a spondylodiscitis-like lesion which is usually confined to one vertebral body. The lesions are predominantly lytic and associated with irregularity of the vertebral end plate with adjacent bone marrow changes. On MR imaging they may show decreased signal intensity on both T1- and T2-weighted images or increased signal intensity on T2-weighted images (Fig. 31) [30, 31]. There may be subsequent collapse of the vertebral body. The adjacent disc usually shows minimal involvement but the lesion does not cross the intervertebral disc space as is seen in infectious spondylitis. The lesions may gradually heal but the MR findings may persist for years after presentation.
Pathogenesis
The pathogenesis of the SAPHO spectrum remains unknown but two hypotheses have been suggested:
Infection by an agent of low virulence
The first hypothesis is that the bone lesions in SAPHO are due to a pathogen of low virulence which is transmitted via a blood-borne route. Alternatively there maybe an autoimmune response triggered by a bacterial or viral pathogen [32, 33]. Pathological examination of biopsy specimens from the bone lesions shows non-specific acute, subacute or chronic osteomyelitis. Moreover the radiological features of SAPHO in the spine and long bones may suggest subacute or chronic infection. Finally Propionibacterium acnes has been isolated in bone biopsy specimens, synovial tissue and fluid from SAPHO patients, suggesting a possible causative role for this organism [34, 35, 36, 37, 38, 39]. However, P. acnes is an anaerobic saprophyte that is frequent in the skin and which is a common contaminant of specimens obtained via a transcutaneous route. Moreover, trials of antibiotics have generally been unhelpful [40], although there are case reports of dramatic responses to prolonged courses of doxycycline [41].
Seronegative spondyloarthropathy
A link with seronegative spondyloarthropathies has also been suggested due to the high frequency of axial involvement (sacroiliitis and spinal lesions); asymmetrical paravertebral ossification indistinguishable from that encountered in psoriatic spondylarthropathy; and the possible association with psoriasis and with inflammatory bowel diseases (i.e. Crohn's disease or ulcerative colitis). HLA B27 is reported as being positive in 13–30% of cases [4, 11, 40]. In other series [21, 27] there was no significant difference in the frequency of HLA B and C antigens in the cases reported from those in controls. Rheumatoid factor is negative.
Diagnosis
The radiologist plays a key role in the diagnosis of the SAPHO spectrum because awareness of this entity facilitates differentiation from other diseases which can share similar radiological features (especially osteomyelitis, osteosarcoma, Ewing sarcoma and Paget's disease). The diagnosis is not difficult when typical bone lesions (sclerosis and hyperostosis) are located in characteristic target sites (anterior chest wall, spine and sacroiliac joint in adults; metaphyses of long tubular bones in children), especially if they are associated with PPP or acne. The diagnosis is much more difficult, however, if the sites of involvement or radiographic findings are atypical, especially if the patients are free of skin disease. However, the questioning of the patient has to be detailed, as a delay of several years can separate cutaneous and skeletal lesions. In such cases, scintigraphy can be very helpful. Indeed, in view of the possible fluctuation of the clinical symptoms, the main contribution of bone scintigraphy is to show activity at unsuspected sites which are clinically silent at the time of scintigraphy, especially at the anterior chest wall [7]. The presence of a "bull's head" configuration of increased activity at the sternoclavicular region is a highly specific manifestation of the SAPHO spectrum [8] (Fig. 12). Detection of multiple lesions can also be helpful for the diagnosis (Fig. 26). In the other cases, biopsy of the bone lesions and follow-up, in some cases over several years, may allow confirmation of the diagnosis.
Multislice CT with reformatted images can accurately define the extent of involvement, particularly of the anterior chest wall. MR imaging is useful for evaluating the degree of activity, particularly in relation to lesions in the anterior chest wall, the spine and long bones. The imaging findings in vertebral involvement in CRMO are distinctly different from those seen in infective spondylodiscitis. These appearances can therefore be of critical importance in the diagnosis of CRMO as tissue culture of these lesions (often difficult to secure) mostly proves to be negative.
Treatment
Non-steroidal anti-inflammatory drugs are usually effective for the relief of pain and remain the principal symptomatic treatment. In cases of severe pain, a low dose of corticosteroids, analgesics such as codeine, or cyclosporine can be prescribed. Local treatments such as intra-articular corticosteroid injections often are effective in relieving pain. Some efficacy with prolonged antimicrobial therapy including tetracyclines, pamidronate and sulfasalazine has been reported by some authors but not by others [14, 34, 41, 42, 43].
References
Windom RE, Sandford JP, Ziff M. Acne conglobata and arthritis. Arthritis Rheum 1961; 4:632–635.
Gideon A, Holthusen W, Masel L. Subacute and chronic symmetrical osteomyelitis. Ann Radiol 1972; 15:329–342.
Bjorksten B, Gustavson KH, Eriksson B et al. Chronic recurrent multifocal osteomyelitis and pustulosis palmoplantaris. J Pediatr 1978; 932:227–231.
Chamot A, Benhamou CL, Kahn MF, et al. Le syndrome acne pustulose hyperostose osteite (SAPHO). Rev Rhum 1987; 54:187–196.
Benhamou CL, Chamot AM, Kahn MF. Synovitis-acne-pustulosis-hyperostosis osteomyelitis syndrome (SAPHO). Clin Exp Rheumatol 1988; 6:109–112.
Grosshans EM. SAPHO the impossible acronym. Dermatology 1993; 186:161–162.
Boutin RD, Resnick D. The SAPHO syndrome: an evolving concept for unifying several idiopathic disorders of bone and skin. AJR Am J Roentgenol 1988; 170:585–591.
Freyschmidt J, Sternberg A. The bull's head sign: scintigraphy pattern of sternoclavicular hyperostosis and pustulotic arthrosclerosis. Eur Radiol 1998; 8:807–812.
Kasperzyk A, Freyschmidt J. Pustolotic arthro-osteitis: spectrum of bone lesions with palmoplantar pustulosis. Radiology 1994; 191:207–211.
Sugimoto H, Tamura K, Fujii T. The SAPHO syndrome: defining the radiological spectrum of disease comprising the syndrome. Eur Radiol 1998; 8:800–806.
Hayem G, Bouchaud-Chabot A, Benali K, et al. SAPHO syndrome: a long term follow up study of 120 cases. Semin Arthritis Rheum 1999; 293:159–171.
Jurik AG. Anterior chest wall involvement in patients with pustulosis palmoplantaris. Skeletal Radiol 1990; 19:271–277.
Reith JD, Bauer TW, Schils JP. Osseous manifestations of SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome. Am J Surg Pathol 1996; 20:1368–1377.
Van Doornum S, Barraclough D, McColl G, Wicks I. SAPHO: Rare or just not recognised? Semin Arthritis Rheum 2000; 30:70–77.
Davies AM, Marins AJ, Evans N, et al. SAPHO syndrome: 20 year follow up. Skeletal Radiol 1999; 28:159–162.
Kahn MF, Khan MA. The SAPHO syndrome. Baillieres Clin Rheumatol 1994; 8:333–362.
Maugars Y, Berthelot JM, Ducloux JM, Prost A. SAPHO syndrome. a follow up study of 19 cases with special emphasis on enthesis involvement. J Rheumatol 1995; 22:2135–2141.
Jurik AG, Egund N. MRI in chronic recurrent multifocal osteomyelitis. Skeletal Radiol 1997; 26:230–238.
Watts RA, Crisp AJ, Hazleman BL, et al. Arthro-osteitis: a clinical spectrum. Br J Rheum 1993; 32:403–407.
Nachtigal A, Cardinal E, Bureau NJ, et al. Vertebral involvement in SAPHO syndrome: MRI findings. Skeletal Radiol 1999; 28:163–168.
Van Holsbeeck M, Martel W, Dequeker J, et al. Soft tissue involvement, mediastinal pseudotumour, and venous thrombosis in pustulotic arthro-osteitis. Skeletal Radiol 1989; 18:1–8.
Toussirot E, Dupond JL, Wendling D. Spondylodiscitis in SAPHO syndrome. A series of eight cases. Ann Rheum Dis 1997; 56:52–58.
Sonozaki H, Azuma O, Okai K, et al. Clinical features of 22 cases with "inter-sterno-costo-clavicular " ossification. A new rheumatic syndrome. Arch Orthop Trauma Surg 1979; 95:13–22.
Ellis BI, Shier CK, Leisen JC, et al. Acne-associated spondyloarthropathy: radiographic features. Radiology 1987; 162:541–545.
Eyrich GKH, Harder C, Sailer HF, et al. Primary chronic osteomyelitis associated with synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO syndrome). J Oral Pathol Med 1999; 28:456–464.
Huaux JP, Maldague B. Malghem J, et al. Pustulotic arthro-osteitis and related disorders in children and adults. JBR-BTR 1986; 69:345–354.
Rosner IA, Richter DE, Huettner TL, et al. Spondyloarthropathy associated with hidradenitis suppurativa and acne conglobata. Ann Intern Med 1982; 97:520–525.
Cotten A. Flipo RM, Mentre A, et al. SAPHO syndrome. Radiographics 1995; 15:1147–1154.
Hatem SF, et al. Case 3: Chronic recurrent multifocal osteomyelitis (CRMO). AJR Roentgen 01 1997; 169:285; 289–291.
Tyrrell PNM, Cassar-Pullicino VN, Eisenstein JF, et al. Back pain in childhood. Ann Rheum Dis 1996; 55:789–793.
Anderson S, et al. Imaging of chronic recurrent multifocal osteomyelitis of childhood first presenting with isolated primary spinal involvement. Skeletal Radiol DOI 10.1007/s00256-002-0602-0
Hellman DB. Spondyloarthropathy with hidradenitis suppurativa. JAMA 1992; 267:2363–2365.
Schwartz B. Infectious agents. Immunity and rheumatic diseases. Arthritis Rheum 1990; 33:457–465.
Kotilainen P, Merilahti-Palo R, Lehtonen OP, et al. Case report. Propionibacterium acnes isolated from sternal osteitis in a patient with SAPHO syndrome. J Rheumatol 1996; 23:1302–1304.
Kooijmans-Coutinho MF, Markusse HM, Dijkmans BAC. Infectious arthritis caused by Propionibacterium acnes: a report of two cases. Ann Rheum Dis 1989; 48:851–852.
Anneli Savolainen H, Von Essen R, Anti J, Jahkola M. Propionibacterium acnes in purulent arthritis: probable cause of iatrogenic infection (letter). J Rheumatol 1988; 15:6.
Sulkowski MS, Abonik IZ, Morris EI, Granger DL. Infectious arthritis due to Propionibacterium acnes in a prosthetic joint. Clin Infect Dis 1994; 19:224–225.
Suter F, Silanos MA, Tabacchi G, Maggiolo F. A case of Propionibacterium acnes spinal osteomyelitis. J Clin Microbiol Infect Dis 1992; 11:196–197.
Honan M, White GW, Eisenberg GM. Spontaneous infectious diseases in adults. Am J Med 1996; 100:85–89.
Wagner AD, Mai U, Hammer M, Zeidler H. Long term antibiotic therapy in patients with SAPHO syndrome (abstract). Arthritis Rheum 1997; 40(Suppl 9):562.
Ballara SC, Siraj QH, Maini RN, Venables PJW. Sustained response to doxycycline therapy in two patients with SAPHO syndrome. Arthritis Rheum 1999; 42:819–821.
Edlund E, Johnsson U, Lidgren L, et al. Palmoplantar pustulosis and sterno-costo-clavicular arthro-osteitis. Ann Rheum Dis 1998; 47:809–815.
Rothschild B, Schils J, Lavelle H. Potential therapeutic approach to SAPHO. Semin Arthritis Rheum 2000; 29:332–334.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Earwaker, J.W.S., Cotten, A. SAPHO: syndrome or concept? Imaging findings. Skeletal Radiol 32, 311–327 (2003). https://doi.org/10.1007/s00256-003-0629-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-003-0629-x