Abstract
Alpha-mangostin (α-MG) has been reported to be an effective antibacterial agent against planktonic cells of many Gram-positive bacteria. However, the antibiofilm potency of α-MG remains unexplored till date. In this study, the antibiofilm and mature biofilm eradication ability of α-MG against Staphylococcus epidermidis RP62A (ATCC 35984) biofilms were evaluated. The minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) of α-MG against S. epidermidis RP62A were found to be 1.25 and 5 μg/mL, respectively. α-MG exhibited a phenomenal concentration dependent rapid bactericidal activity (>4-log reduction within 5 min). In a multi-passage resistance analysis using S. epidermidis, no development of resistance to α-MG as well as antibiotics was observed in its habituation. α-MG at its 1/2 MIC effectively inhibited the initial biofilm formation of S. epidermidis, which was further confirmed through scanning electron microscopic (SEM) analysis that portrayed a lucid reduction in the aggregation and the spread of biofilm. The crystal violet staining and viable cell quantification results confirmed the eradication of preformed immature and mature biofilms of S. epidermidis by α-MG in a concentration dependent manner. Besides, the biofilm eradication ability was also confirmed through SEM and live/dead BacLight staining using confocal laser scanning microscopy (CLSM). Thus, the present study exemplifies that α-MG could plausibly assist to eliminate biofilm infections associated with multidrug-resistance staphylococci.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus epidermidis beyond its local homoeostasis characteristics on human skin as a commensal flora, it has been well recognized for the most frequent cause of health care-associated bloodstream infections and biomaterial-associated infections (Otto 2012; Ziebuhr et al. 2006). S. epidermidis are the utmost notable member of coagulase-negative staphylococcal group (CoNS), as nearly 80% of CoNS isolates were S. epidermidis. It is ranked first and third in causing native valve infective endocarditis (NVIE) and prosthetic valve infective endocarditis (PVIE), respectively. Despite its lesser virulence, it has been well adapted to colonize and establish highly structured, multilayered robust biofilms on any implanted biomaterial surfaces such as vascular catheters, prosthetic joints, and artificial heart valves (Qin et al. 2007).
In S. epidermidis, biofilm formation is the most imperative virulence trait making this commensal inhabitant as hazardous to implanted medical device usage. In the intricate architecture of biofilm, bacterial cells encase themselves and escape from host defense mechanisms as well as antimicrobial agents, which eventually leads to chronic and refractory infections (Lefebvre et al. 2016; Nilsson et al. 2016; Falsetta et al. 2012). Besides, S. epidermidis infections associated with biofilms persist until the removal or subsequent replacement of implantable medical devices, resulting in further distress and cost (Donlan and Costerton 2002). Furthermore, this primary pathogenic trait-the biofilm formation has also been envisaged for the increased emergence of antibiotic resistance in several strains of clinical settings.
In the prevailing antimicrobial therapy, S. epidermidis in particular methicillin-resistant S. epidermidis (MRSE) are being treated with the last resort of antibiotics viz., vancomycin, daptomycin, and linezolid, which affect the planktonic cells rather than targeting the sessile cells of biofilm architecture (Roper et al. 2000; Parra-Ruiz et al. 2012; Reiter et al. 2014). This has hastened and widened the quest for the discovery of novel antimicrobial agents from natural sources with proficiency to penetrate biofilm and target sessile cells of such recalcitrant biofilm-forming dreadful pathogen.
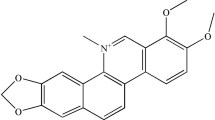
Alpha-mangostin (α-MG), a natural xanthanoid found predominantly as secondary metabolite in pericarps of Mangosteen (Garcinia mangostana Linn) also referred as “queen of fruits” (Ibrahim et al. 2016). Hitherto, plethora of reports on α-MG have well demonstrated its broad spectrum pharmaceutical significance including anti-inflammatory, anti-tumor, cardioprotective, anti-diabetic, antibacterial, antifungal, antiparasitic, antioxidant, antiobesity and antibacterial activities (Ibrahim et al. 2016). Although, the mechanism of bactericidal action of α-MG on planktonic cells of Staphylococcus aureus has been extensively investigated by Koh et al. (2013) and studies related to antibiofilm and biofilm eradicating efficacy of α-MG on bacterial pathogens are scarce. Therefore, the current study was aimed to uncover the in vitro bactericidal efficacy of α-MG on both planktonic and sessile cells of methicillin-resistant S. epidermidis (RP62A; ATCC 35984).
Materials and methods
Bacterial strain, culture media, and conditions
S. epidermidis RP62A (ATCC 35984) was purchased from the American Type Culture Collection (ATCC, Manassas, USA) and was maintained in tryptic soy broth (TSB; Himedia, India) at −80 °C with 30% glycerol. For biofilm assay, TSB was supplemented with 0.25% glucose (TSBG) and incubated at 37 °C.
Determination of minimum inhibitory concentration and minimum bactericidal concentration
The minimum inhibitory concentration (MIC) was determined by microdilution method in Mueller Hinton broth (MHB, HiMedia, India) (CLSI 2006). Vancomycin (HiMedia, India) and α-MG (Sigma, St. Louis, MO, USA) was diluted in a 24-well microtitre plate (MTP) to obtain final concentrations ranging from 40 to 0.156 and 10–0.156 μg/mL, respectively. An aliquot of the bacterial suspension (10 μl, 1 × 106 CFU/mL) was used to inoculate and incubated at 37 °C for overnight. The MIC was recorded as the lowest concentration of α-MG that inhibits the visible growth of bacteria. For minimum bactericidal concentration (MBC), 100 μL from MIC assay MTP wells with no visible bacterial growth were spread on Mueller Hinton agar (MHA) plates and incubated at 37 °C for 24 h. MBC was recorded as the lowest concentration of α-MG which allowed to grow less than five colonies on each plate.
Kinetics of killing planktonic cells
A 1: 200 dilution (1 × 106 CFU/mL) of the overnight culture of S. epidermidis was used to inoculate 20 mL of fresh MHB. Concentrations of α-MG from 0.3125 μg/mL (1/4 MIC) to 10 μg/mL (8 × MIC) were added to MHB and incubated for 12 h at 37 °C with shaking (160 rpm). For every 5 min of time interval, 100 μL of the culture from each tube was serially diluted, spread on MHA plates and incubated at 37 °C for 24 h. After incubation, the viable bacterial cells (colony forming unit—CFU) were counted and the rate of killing was determined by plotting CFU/mL against time (D’Arezzo et al. 2012; Liu et al. 2014).
α-MG habituation of S. epidermidis cells
TSBG (10 mL) supplemented with α-MG (0.156 μg/mL) were inoculated with 100 μL of standardized cell suspension (1 × 107 CFU/mL) and incubated at 37 °C for 24 h. In parallel, the non-habituated cells (bacteria were grown in TSBG without α-MG) were maintained as control. After incubation, non-habituated and α-MG habituated cells were recovered by centrifugation (8000×g for 10 min), washed twice with phosphate buffer saline (PBS; pH 7.4), and resuspended in PBS to form standardized cell suspension as above. The non-habituated and α-MG habituated cells were sub-cultured daily for 4 days in fresh TSBG with and without α-MG at same concentration. At each successive passage, the bacterial growth was evaluated by absorbance at 600 nm. After four sequential passages at same concentration of α-MG, cells were transferred to TSBG at one fold increasing concentration of α-MG (0.3125 μg/mL). This process was repeated until the α-MG habituated cells stops growing (Apolonio et al. 2014).
Penetration of antibiotics through α-MG habituated and non-habituated biofilms
A 20 μL drop of standardized cell suspension (0.5, 107 CFU/mL) of control and α-MG habituated cultures were used to seed on black, polycarbonate membranes (PCM) (13 mm diameter; 0.4 mm pore size (Merck Millipore Ltd., India)) and placed on MHA plates. The plates were incubated upturned at 37 °C for 48 h. For every 24 h of incubation, the membrane-carried biofilms (MCBs) were transferred to fresh TSA plates. The MCBs were then washed with PBS by shaking at 160 rpm for 1 min to eliminate non-adherent cells. The MCBs were transferred to MHA plates swabbed with control and α-MG habituated S. epidermidis to McFarland standard 0.5, where it gives a confluent lawn of growth following incubation. The nitrocellulose membrane (6 mm diameter; 0.4 mm pore size) was placed over the surface of each MCBs along with pre-moistened antibiotic disc (amikacin, 30 μg; tetracycline, 30 μg and vancomycin, 30 μg). In parallel, the control assemblies were made with sterile membranes and antibiotic discs. The plates were incubated at 37 °C for 24 h and zones of growth inhibition were documented. The clear zones of control assemblies were considered as 100% penetration (retardation) which is used to find out the percentage of antibiotics penetration through biofilms (Singh et al. 2010). Experiments were performed in duplicate.
Assessment of biofilm biomass
The α-MG at 1/16, 1/8, 1/4, 1/2, and 1 × MIC was added to TSBG containing bacterial suspension of 106 CFU/mL and incubated for 24 h at 37 °C. After incubation, growth OD was measured at 600 nm. The free floating planktonic cells in the MTP wells were discarded and the plates were washed thrice with sterile PBS. The adhered sessile cells were stained with 0.4% (w/v) crystal violet (CV). Subsequently, the excess stain was washed thrice with sterile distilled water. One milliliter of 20% glacial acetic acid was added to solubilize stained biofilm cells and it was measured spectrophotometrically at 570 nm using multilabel reader (Molecular devices, SpectraMax M3, USA) (Cramton et al. 1999; Packiavathy et al. 2013).
Assessment of bacterial viability using XTT assay
The cellular viability was quantified using the tetrazolium sodium 3′-{1-[(phenylamino)-carbonyl]-3–4-tetrazolium}-bis(4-methoxy-6-nitro)-benzene sulfonic acid hydrate (XTT) reduction assay described by Gowrishankar et al. (2014). The sodium salt of XTT was dissolved in sterile PBS (1 mg/mL) and menadione was dissolved in acetone (1 mM). XTT/menadione solution was prepared freshly prior to each experiment at the ratio of 12.5:1 of XTT and menadione, respectively. After incubation, both planktonic and biofilm cells were removed from the vehicle control (VC) and treated (α-MG and vancomycin) wells. The bacterial cells were washed thrice with sterile PBS and resuspended in 175 μl of the same buffer. Twenty-five microliters of XTT/menadione solution was added to this cell suspensions and incubated dark at 37 °C for 8 h. Cellular viability was measured spectrophotometrically through the reduction of XTT into orange colored formazan at 490 nm.
Impact of α-MG against immature and mature biofilm
The effect of α-MG on immature (6 h old) and mature (24 h old) biofilms of S. epidermidis was assessed (Stepanovic et al. 2007). Overnight cell suspension (10 μL, 106 CFU/mL) was used to inoculate 1 mL of TSBG in MTP wells and incubated statically at 37 °C for 6 h (immature) and 24 h (mature). After incubation, the medium containing non-adherent bacterial cells was removed and 1 mL of fresh TSBG with α-MG and vancomycin at the concentrations of 16 ×, 8 ×, 4 ×, 2 × and 1 × MIC were added to separate wells and incubated further for 16 h at 37 °C. After incubation, biofilm biomass and metabolic activity of viable cells were quantified as per the above mentioned protocols.
Scanning electron microscopic analysis of immature biofilms
S. epidermidis was statically incubated for 6 h in the wells of MTP with 1 × 1 cm glass slides at 37 °C, then α-MG and vancomycin were added at the concentration of 16× MIC in fresh TSB medium and incubated for another 16 h at 37 °C. After incubation, non-adherent cells were removed and sessile cells in the glass slides were subjected to scanning electron microscopic (SEM) analysis. The biofilms on glass slides were flooded with 2.5% glutaraldehyde for 12 h and washed in 0.1 M sodium acetate buffer (pH 7.3). Biofilms were dehydrated in a graded ethanol series from 30, 50, 60, 70, 90, and 95% for 10 min each, followed by rinsing thrice with 100% ethanol. Specimens were dried and immediately sputter coated with metal. Biofilms were visualized by using a Hitachi S-3000H scanning electron microscope (Hitachi, Japan) (Liu et al. 2015).
Observation of S. epidermidis biofilms by confocal laser scanning microscopy
The effect of α-MG and vancomycin on bacterial viability in mature (24 h old) biofilms of S. epidermidis ATCC 35984 was evaluated by confocal laser scanning microscopy (CLSM) (Sivaranjani et al. 2016). After incubation, VC and treated biofilms were stained with SYTO9 and propidium iodide (PI) (Live/Dead staining, Molecular Probe) and visualized by CLSM (Model: LSM 710, Carl Zeiss, Germany).
Statistical analysis
All experiments were performed in triplicate. Data were expressed as arithmetic mean ± standard deviation and analyzed with Dunnett-ANOVA test. Data regarding the penetration of antibiotics through biofilms was alone analyzed using two-tailed, paired t test using statistical software package (SPSS Chicago, IL, USA). P values of ˂0.05 were considered statistically significant.
Results
Effect of α-MG on growth of S. epidermidis planktonic cells
The MIC of α-MG and vancomycin against S. epidermidis was found to be 1.25 and 10 μg/mL, respectively. The MBC of α-MG and vancomycin for S. epidermidis was 5 and 20 μg/mL, respectively.
The rapid killing efficacy of α-MG on planktonic cells of S. epidermidis was investigated by performing time kill curve assay. As anticipated, α-MG displayed rapid concentration-dependent killing of S. epidermidis cells at concentrations above 4× MIC (5 μg/mL) and 2× MIC (2.5 μg/mL) of α-MG, achieving 6 log and 4 log reduction of viable count within 5 min of exposure time, respectively. A less than 2 log reduction of viable counts was achieved while treating with 1× MIC (1.25 μg/mL) of α-MG (Fig. 1a). On the other hand, vancomycin displayed no significant reduction in viable cells even after 6 h of incubation with vancomycin at 2×, 4× and 8× MIC (Fig. 1b).
Impact of α-MG habituation on development of resistance
Antibiotic resistance was defined as >4-fold increase from its original MIC value (Farrell et al. 2011). In order to evaluate the acquisition of resistance to α-MG on S. epidermidis, subsequent passage was performed. The S. epidermidis cells grown at the concentrations of α-MG from 0.156 to 1.25 μg/mL, no obvious growth inhibition was observed up to 16° passage. While the α-MG concentration was increased to 2.5 μg/mL, the bacterial cell growth was inhibited gradually in 17° and 18° passage and complete visible growth inhibition was observed at 19° passage. Through this experiment, it was concluded that even the continuous exposure of α-MG did not develop any resistance in S. epidermidis, in which 1-fold increase of MIC was observed for α-MG (i.e., MIC at 1° passage 1.25 μg/mL and MIC at 19° passage 2.5 μg/mL) (Fig. 2). Besides, the influence of α-MG habituation on the susceptibility of S. epidermidis planktonic cells to antibiotics such as ampicillin, amikacin, tetracycline, rifampicin, gentamycin, vancomycin, and erythromycin was evaluated. The α-MG habituated planktonic cells did not induce resistance to the tested antibiotics (Table S1).
Concomitantly, the impact of α-MG habituated S. epidermidis biofilms was also assessed using biofilm penetration assay. The penetration of glycopeptide antibiotic-vancomycin was significantly reduced through α-MG habituated and non-habituated biofilms in comparison with control assemblies. In contrast, no significant difference was observed in the penetration of tetracycline and amikacin through α-MG habituated and non-habituated biofilms (Fig. 3). The diameter of the zone of inhibition in α-MG habituated and non-habituated biofilms was similar when compared with their respective control assemblies (Table 1). Hence, it is appropriate to state that α-MG habituation does not induce the resistance in planktonic as well as biofilm cells of S. epidermidis.
A Picto-graphical depiction of the antibiotics penetration through control assemblies (a), non-habituated (b), and α-MG habituated (c) S. epidermidis biofilms as determined on MHA plates by the zone of bacterial growth inhibition. B Schematic representation of the experimental setup used to analyze the antibiotics penetration through the biofilms. (a) MHA plates, (b) 13-mm black polycarbonate membrane, (c) α-MG habituated/non-habituated S. epidermidis biofilms grown on black polycarbonate membrane, (d) 6-mm nitrocellulose membrane, and (e) 6-mm antibiotic discs—tetracycline, vancomycin, and amikacin
Effect of α-MG on S. epidermidis biofilm formation
A visible growth reduction was observed at 1 × MIC of α-MG. At 1/2 MIC, the growth was decreased up to 40% and biofilm was inhibited up to 80%. A less pronounced inhibitory effect on growth and biofilm formation (30–40%) was observed at 1/4 to 1/16 MIC treatment of α-MG (Fig. 4). Furthermore, SEM micrograph clearly revealed the structurally complex and dynamic multilayered matrix architecture of S. epidermidis biofilm in VC, whereas the α-MG (1/2 MIC) treated micrographs absolutely lacks such depiction of matrix structures (Fig. 5).
Effect of α-MG and vancomycin on immature biofilms
As a prelude to assess the inhibition of biofilm formation of S. epidermidis, the ability of α-MG at MIC to disrupt the immature biofilm was examined. Outcome of this assay demonstrated that α-MG at 1× and 2 × MIC was not sufficient enough to disrupt the immature biofilm. The same observation was also found with vancomycin (1× and 2 × MIC) treated bacterial biofilms. Thus, the compound at increasing concentrations was used to assess its biofilm disrupting efficacy. The increasing concentrations of α-MG from 4×, 8× and 16 × MIC significantly eradicated the immature biofilms accordingly by 55, 73, and 93%. On the other hand, vancomycin at 4×, 8×, and 16 × MIC disrupted the biofilm only to the level of 10, 26, and 36%, respectively. The XTT assay also confirmed the results of immature biofilm disruption assay, as α-MG significantly killed the sessile cells of S. epidermidis in a dose dependent manner. α-MG at 4×, 8×, and 16 × MIC effectively reduced the viability of preformed biofilm cells by 40, 71, and 97%, whereas vancomycin showed 20, 32, and 38%, respectively (Table 2). The SEM micrograph of VC and vancomycin treated at 16 × MIC clearly depicted highly structured, multilayered, and robust biofilm matrix formation by exopolysaccharides. In contrast, the micrographs of α-MG (4×, 8×, and 16× MIC) treatment portrayed concentration-dependent disruption in the preformed immature biofilms. The results of the SEM analysis clearly depicts that concentration dependent bactericidal activity was observed when the immature biofilms were treated with α-MG at 4×, 8×, and 16× MIC respectively (Fig. 6). At 4× MIC of α-MG, the bacterial cells were killed effectively and the three dimensional structure of biofilm was also reduced. However, live cells with intact cell membrane were often observed at 4× MIC of α-MG treated biofilm cells. Furthermore, biofilms treated at 8× and 16× MIC of α-MG evidently decreased the viable bacterial load as well as the aggregation in the matrix structure while this was not found in vancomycin treated biofilms even at 16× MIC.
Effect of α-MG and vancomycin on mature S. epidermidis biofilms
At the tested concentrations (8× and 16× MIC), α-MG was proficient enough to disrupt the preformed biofilms and effectively killed the biofilm embedded cells. In contrast, vancomycin was found ineffective in killing the sessile bacterial cells of the mature biofilm (Table 3). On the other hand, the bactericidal effect of α-MG on 6 h old biofilms was very high when compare to 24 h old biofilms. The bactericidal activity of α-MG on mature (24 h old) biofilms was also assessed by CLSM with Live/Dead staining. CLSM micrographs of α-MG treated with increasing concentration displayed an elevated level of PI intensity and low intensity of green fluorophore due to SYTO9, which clearly validated the phenomenal concentration dependent killing efficacy of α-MG on mature biofilms. Nevertheless, vancomycin even at 16× MIC was inefficient in killing the sessile cells of S. epidermidis RP62A (Fig. 7).
Discussion
Since 1980s, plethora of scientific reports have envisaged α-MG as a potent antimicrobial agent with rapid killing efficacy even at very low MIC values (Sakagami et al. 2005; Koh et al. 2013) against various Gram-positive pathogens, particularly methicillin-resistant S. aureus (MRSA; MIC value of 1.95 μg/mL) (Chin and Kinghorn 2008) and vancomycin resistant Enterococci (VRE; MIC value of 6.25 μg/mL) (Sakagami et al. 2005). The present study also demonstrates a rapid bactericidal activity of α-MG against the planktonic cells of S. epidermidis RP62A with a very low MIC and MBC values of 1.25 and 5 μg/mL, respectively. A phenomenal rapid bactericidal efficacy of α-MG was certain, as it readily killed the planktonic cells of S. epidermidis at 2× MIC of α-MG to the level of 4-log10 reduction with in 5 min. This is in par with the findings of Koh et al. (2013), wherein they reported that α-MG exhibits a rapid bactericidal efficacy (3-log10 reduction within 5 min) in methicillin-resistant Staphylococcus aureus (MRSA) via disrupting the integrity of cytoplasmic membrane leading to the loss of intracellular components. Earlier reports on antibacterial activity of α-MG against Bacillus cereus (Koh et al. 2013), Streptococcus pneumonia (Coyle and Rybak 2001) and Streptococcus mutans (Nguyen and Marquis 2011) have also demonstrated a similar fashion of killing action. Therefore, it is envisaged that α-MG could plausibly target the cytosolic membrane of S. epidermidis to cause rapid death.
Nevertheless, the action of vancomycin even after 6 h of incubation was in vain to achieve 4-log10 reduction in viable bacteria count. A similar kind of observation was also reported by Coyle and Rybak (2001), who signifies that even after 300 min of vancomycin exposure at higher concentration, a 3-log10 reduction in viable S. pneumoniae was unachievable. It has also been broadly accepted that vancomycin exhibits an inherently slower mechanism of action by binding to the peptidoglycan component, D-Ala- D-Ala terminus and inhibits the crosslinking of peptidoglycan through transpeptidation reaction (Beauregard et al. 1995).
α-MG is also believed to pose lower risk for selective pressure, as it mimics the chemical structure of meta-phenylene ethynylene (mPE), a membrane targeting cationic antimicrobial peptide that exhibit rapid bactericidal activity and shows a lesser possibility toward rising resistance to Gram-positive bacteria (Tew et al. 2006). Our result signifies that α-MG elicit rapid bactericidal activity as it targets the bacterial membrane (Koh et al. 2013) and hence, resistance is prevented in both planktonic and biofilm cells by averting the mutational possibility of membrane structure.
In addition, α-MG also exhibits a significant biofilm inhibitory efficacy at sub-MICs. SEM result also elucidates that 1/2 MIC of α-MG treatment effectively reduced the three dimensional structure of biofilm in comparison to untreated control. The bacterial growth OD and CV quantification of biofilm confirmed that the biofilm inhibitory potential of α-MG is directly proportional to the inhibition of bacterial growth. This could be explained by “inoculum effect,” which means the effect of any bactericidal agents turn to be less effective when the bacterial cell density is higher than the amount of bactericidal agent available per bacterial cells (Udekwu et al. 2009). Besides, several studies suggested that sub-inhibitory concentrations of various antibiotics, including nafcillin, tetracycline, and vancomycin increase the biofilm formation of staphylococci (Frank et al. 2007; Hsu et al. 2011; Kuehl et al. 2009). Hence, α-MG with its initial biofilm inhibitory efficacy against S. epidermidis at sub-inhibitory concentrations, it would not fall into the above said class of antibiotics.
Even though the planktonic cells are highly sensitive to most of the known antibacterial agents, cells residing inside the biofilms are extremely robust to eradicate. As reported by Claessens et al. (2015), the routine practice of determining bacterial antibiotic susceptibility for planktonic cells is not a better insight for the response of sessile communities. Hence, in the current study, CV and XTT quantification methods are used to assess the effects of α-MG and vancomycin on in vitro preformed biofilms of S. epidermidis (Claessens et al. 2015). The CV and XTT quantification assay results revealed that α-MG showed profound killing and eradicating potential against immature biofilms of S. epidermidis. The SEM micrographs of immature biofilms treated with α-MG have also depicted the better killing efficacy with morphological disruption of sessile cells; however, no such effect was observed in micrographs of vancomycin treated samples. All these results confirmed the low killing efficacy of vancomycin toward sessile cells of S. epidermidis unlike the planktonic cells which were sensitive to vancomycin. This result falls in line with the findings of Tenover et al. (2001), indicating that vancomycin failed to disrupt the mature biofilm of S. epidermidis even at the highest concentration. Moreover, the conventional antibiotic regimens of vancomycin treatment are not sufficient to diminish biofilms associated infections. It is a well-known fact that mature biofilms are extremely robust to all kinds of antibiotics. Therefore, in this study, the potential of α-MG in disrupting and killing the mature biofilm embedded cells was evaluated. Although α-MG is an effective bactericidal agent for inhibiting the onset of biofilm formation and immature biofilms, the killing activity on mature (24 h old) biofilms was comparatively low which proved that the bactericidal activity on biofilms solely depend on the age of biofilms. Furthermore, current treatment strategies also relies on the combinatorial therapy as one of the effective treatment strategies in which Chusri et al. (2016) reported that α-MG exhibited minimal antibacterial and antibiofilm activity when compared to that of polyherbal formula (Curcuma longa, Areca catechu, Oryza sativa and G. mangostana) viz., Ya-SaMarn-Phlae (YSMP). Hence, this earlier study puts forth an idea that the α-MG reported in the present study can be further evaluated for its antibacterial and antibiofilm activity with other well-known phytochemicals to maximize its activity.
There are several reports available on the phyto-compounds in inhibiting the staphylococcal biofilms. The phyto-compounds such as berberine, carvacrol, oregano, thymol, black pepper, cananga, myrrh oils, demethylfruticuline A, and fruticuline A have been frequently reported for their bactericidal and antibiofilm activity on staphylococcal biofilms (Lee et al. 2014; Nostro et al. 2007; Schito et al. 2011; Wang et al. 2009). In addition, tea tree oil (1%) was reported to inhibit the metabolism of S. aureus biofilm (Kwiecinski et al. 2009). Although tea tree oil is an effective bactericidal agent against wide range of bacteria, administration of sub-lethal concentration of tea tree oil lead to the development of resistance against many of the antibiotics (McMahon et al. 2007). Nevertheless, the treatment of α-MG does not pose any risk of resistance development in both planktonic and biofilms cells of S. epidermidis which is evident through in vitro analysis. Further, in vivo analysis using animal models such as rats/mouse on the effect of α-MG for its bactericidal activity on both planktonic and sessile cells of S. epidermidis RP62A is the need of the hour. However, plethora of reports are available on the in vivo potential of α-MG that potentiate the multifarious activity of α-MG such as reno-protective activity against cisplatin induced nephrotoxicity via inhibiting the catalase production, nitrosative/oxidative stress, renal dysfunction, structural damage and increase in mRNA levels of tumor necrosis factor in rat animal model (Perez-Rojas et al. 2009). In another study, Sampath and Vijayaraghavan (2007) reported that α-MG has a protective effect against lipid-peroxidation and antioxidant defense system during isoproterenol-induced myocardial infarction in rats. Gopalakrishnan et al. (1980) reported the efficiency of α-MG in inhibiting the immunocytoadherence and systemic anaphylaxis in rats and guinea pigs. The intraperitoneal and oral routes administration of α-MG showed significant anti-inflammatory response in both normal and bilaterally adrenalectonized rats (Shankaranarayan et al. 1979). α-MG has also been reported for its cytotoxic effect on head and neck squamous carcinoma (HNSCC) cell lines, human melanoma SK-MEL-28 cell line, epidermoid carcinoma of the mouth (KB) cells, breast cancer (BC-1) cells, human leukemia cell line HL60 and other leukemia cell lines (K562, NB4 and U937) (Suksamrarn et al. 2006; Kaomongkolgit et al. 2011; Wang et al. 2011; Matsumoto et al. 2003). Similarly, Shih et al. (2010) reported that α-MG have anti-metastatic effect on phorbol 12-myristate 13-acetate induced matrix metalloproteinases (MMP-2/MMP-9) expression in human lung adenocarcinoma A549 cells. Kosem et al. (2013) have studied the non-toxic nature of α-MG (4000 μg/mL) in human gingival fibroblast and recognized as safe to treat oral candidiasis due to its strong fungicidal and non-toxic nature.
To sum up, the present study demonstrates α-MG as an effective antibacterial agent against both planktonic and sessile cells of S. epidermidis RP62A without posing any risk for the development of resistance. Further, in vivo investigation using eukaryotic model system together with translational studies is needed to understand the underlying molecular mechanism of action of α-MG against sessile population as well as their efficacy to treat biofilm-mediated infections.
References
Apolonio J, Faleiro ML, Miguel MG, Neto L (2014) No induction of antimicrobial resistance in Staphylococcus aureus and Listeria monocytogenes during continuous exposure to eugenol and citral. FEMS Microbiol Lett 354:92–101
Beauregard DA, Williams DH, Gwynn MN, Knowles DJ (1995) Dimerization and membrane anchors in extracellular targeting of vancomycin group antibiotics. Antimicrob Agents Chemother 39:781–785
Chin YW, Kinghorn AD (2008) Structural characterization, biological effects, and synthetic studies on xanthones from mangosteen (Garcinia mangostana), a popular botanical dietary supplement. Mini Rev Org Chem 5:355–364
Chusri S, Tongrod S, Saising J, Mordmuang A, Limsuwan S, Sanpinit S, Voravuthikunchai SP (2016) Antibacterial and anti-biofilm effects of a polyherbal formula and its constituents against coagulase-negative and -positive staphylococci isolated from bovine mastitis. J Appl Anim Res 45:364–372
Claessens J, Roriz M, Merckx R, Baatsen P, Van Mellaert L, Van Eldere J (2015) Inefficacy of vancomycin and teicoplanin in eradicating and killing Staphylococcus epidermidis biofilms in vitro. Int J Antimicrob Agents 45:368–375
Clinical and Laboratory Standards Institute (2006) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard, CLSI document M7-A7, 7th edn. Clinical and Laboratory Standards Institute, Wayne
Coyle EA, Rybak MJ (2001) Activity of oritavancin (LY333328), an investigational glycopeptide, compared to that of vancomycin against multidrug-resistant Streptococcus pneumoniae in an in vitro pharmacodynamic model. Antimicrob Agents Chemother 45:706–709
Cramton SE, Gerke C, Schnell NF, Nichols WW, Götz F (1999) The intercellular adhesion (ica) locus is present in Staphylococcus aureus and is required for biofilm formation. Infect Immun 67:5427–5433
D’Arezzo S, Lanini S, Puro V, Ippolito G, Visca P (2012) High-level tolerance to triclosan may play a role in Pseudomonas aeruginosa antibiotic resistance in immunocompromised hosts: evidence from outbreak investigation. BMC Res Notes 19:43
Donlan RM, Costerton JW (2002) Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 15:167–193
Falsetta ML, Klein MI, Lemos JA, Silva BB, Agidi S, Scott-Anne KK, Koo H (2012) Novel antibiofilm chemotherapy targets exopolysaccharide synthesis and stress tolerance in Streptococcus mutans to modulate virulence expression in vivo. Antimicrob Agents Chemother 56:6201–6211
Farrell DJ, Robbins M, Rhys-Williams W, Love WG (2011) Investigation of the potential for mutational resistance to XF-73, retapamulin, mupirocin, fusidic acid, daptomycin, and vancomycin in methicillin-resistant Staphylococcus aureus isolates during a 55-passage study. Antimicrob Agents Chemother 55:1177–1181
Frank KL, Reichert EJ, Piper KE, Patel R (2007) In vitro effects of antimicrobial agents on planktonic and biofilm forms of Staphylococcus lugdunensis clinical isolates. Antimicrob Agents Chemother 51:888–895
Gopalakrishnan C, Shankaranarayanan D, Kameswaran L, Nazimudeen S (1980) Effect of mangostin, a xanthone from Garcinia mangostana Linn. in immunopathological & inflammatory reactions. Indian J Exper Biol 18:843–846
Gowrishankar S, Poornima B, Pandian SK (2014) Inhibitory efficacy of cyclo (L-leucyl-Lprolyl) from mangrove rhizosphere bacterium-Bacillus amyloliquefaciens (MMS-50) toward cariogenic properties of Streptococcus mutans. Res Microbiol 165:278–289
Hsu CY, Lin MH, Chen CC, Chien SC, Cheng YH, Su IN, Shu JC (2011) Vancomycin promotes the bacterial autolysis, release of extracellular DNA, and biofilm formation in vancomycin-nonsusceptible Staphylococcus aureus. FEMS Immunol Med Microbiol 63:236–247
Ibrahim MY, Hashim NM, Mariod AA, Mohan S, Abdulla MA, Abdelwahab SI, Arbab IA (2016) α-Mangostin from Garcinia mangostana Linn: an updated review of its pharmacological properties. Arab J Chem 9:317–329
Kaomongkolgit R, Chaisomboon N, Pavasant P (2011) Apoptotic effect of alpha-mangostin on head and neck squamous carcinoma cells. Arch Oral Biol 56:483–490
Koh J, Qiu S, Zou H, Lakshminarayanan R, Li J, Zhou X, Tang C, Saraswathi P, Verma C, Tan DTH, Tan AL, Liu S, Beuerman RW (2013) Rapid bactericidal action of alpha-mangostin against MRSA as an outcome of membrane targeting. Biochim Biophys Acta 1828:834–844
Kosem N, Ichikawa K, Utsumi H, Moongkarndi P (2013) In vivo toxicity and antitumor activity of mangosteen extract. J Nat Med 67:255–263
Kuehl R, Al-Bataineh S, Gordon O, Luginbuehl R, Otto M, Textor M, Landmann R (2009) Furanone at subinhibitory concentrations enhances staphylococcal biofilm formation by luxS repression. Antimicrob Agents Chemother 53:4159–4166
Kwiecinski J, Eick S, Wojcik K (2009) Effects of tea tree (Melaleuca alternifolia) oil on Staphylococcus aureus in biofilms and stationary growth phase. Int J Antimicrob Agents 33:343–347
Lee K, Lee JH, Kim SI, Cho MH, Lee J (2014) Anti-biofilm, anti-hemolysis, and anti-virulence activities of black pepper, cananga, myrrh oils and nerolidol against Staphylococcus aureus. Appl Microbiol Biotechnol 98:9447–9457
Lefebvre E, Vighetto C, Martino PD, Garde VL, Seyer D (2016) Synergistic antibiofilm efficacy of various commercial antiseptics, enzymes and EDTA: a study of Pseudomonas aeruginosa and Staphylococcus aureus biofilms. Int J Antimicrob Agents 48:181–188
Liu H, Zhao D, Chang J, Yan L, Zhao F, Wu Y, Xu T, Gong T, Chen L, He N, Wu Y, Han S, Qu D (2014) Efficacy of novel antibacterial compounds targeting histidine kinase YycG protein. Appl Microbiol Biotechnol 98:6003–6013
Liu M, Peng W, Qin R, Yan Z, Cen Y, Zheng X, Pan X, Jiang W, Li B, Li X, Zhou H (2015) The direct anti-MRSA effect of emodin via damaging cell membrane. Appl Microbiol Biotechnol 99:7699–7709
Matsumoto K, Akao Y, Kobayashi E, Ohguchi K, Ito T, Tanaka T, Iinuma M, Nozawa Y (2003) Induction of apoptosis by xanthones from mangosteen in human leukemia cell lines. J Nat Prod 66:1124–1127
McMahon MAS, Blair IS, Moore JE, McDowell DA (2007) Habituation to sub-lethal concentrations of tea tree oil (Melaleuca alternifolia) is associated with reduced susceptibility to antibiotics in human pathogens. J Antimicrob Chemother 59:125–127
Nguyen PTM, Marquis RE (2011) Antimicrobial actions of α-mangostin against oral streptococci. Can J Microbiol 57:217–225
Nilsson M, Rybtke M, Givskov M, Høiby N, Twetman S, Tolker-Nielsen T (2016) The dlt genes play a role in antimicrobial tolerance of Streptococcus mutans biofilms. Int J Antimicrob Agents 48:298–304
Nostro A, Sudano Roccaro A, Bisignano G, Marino A, Cannatelli MA, Pizzimenti FC, Cioni PL, Procopio F, Blanco AR (2007) Effects of oregano, carvacrol and thymol on Staphylococcus aureus and Staphylococcus epidermidis biofilms. J Med Microbiol 56:519–523
Otto M (2012) Molecular basis of Staphylococcus epidermidis infections. Semin Immunopathol 34:201–214
Packiavathy IA, Sasikumar P, Pandian SK, Ravi AV (2013) Prevention of quorum-sensing-mediated biofilm development and virulence factors production in Vibrio spp. by curcumin. Appl Microbiol Biotechnol 97:10177–10187
Parra-Ruiz J, Bravo-Molina A, Pena-Monje A, Hernandez-Quero J (2012) Activity of linezolid and high-dose daptomycin, alone or in combination, in an in vitro model of Staphylococcus aureus biofilm. J Antimicrob Chemother 67:2682–2685
Perez-Rojas JM, Cruz C, Garcia-Lopez P, Sanchez-Gonzalez DJ, Martinez-Martinez CM, Ceballos G, Espinosa M, Melendez-Zajgla J, Pedraza-Chaverri J (2009) Renoprotection by a-mangostin is related to the attenuation in renal oxidative/nitrosative stress induced by cisplatin nephrotoxicity. Free Radic Res 43:1122–1132
Qin Z, Ou Y, Yang L, Zhu Y, Tolker-Nielsen T, Molin S, Qu D (2007) Role of autolysin-mediated DNA release in biofilm formation of Staphylococcus epidermidis. Microbiology 153:2083–2092
Reiter KC, Sant’Anna FH, d’Azevedo PA (2014) Upregulation of icaA, atlE and aap genes by linezolid but not vancomycin in Staphylococcus epidermidis RP62A biofilms. Int J Antimicrob Agents 43:248–253
Roper DI, Huyton T, Vagin A, Dodson G (2000) The molecular basis of vancomycin resistance in clinically relevant enterococci: crystal structure of D-alanyl-D-lactate ligase (VanA). Proc Natl Acad Sci U S A 97:8921–8925
Sakagami Y, Iinuma M, Piyasena KGNP, Dharmaratne HRW (2005) Antibacterial activity of α-mangostin against vancomycin resistant enterococci (VRE) and synergism with antibiotics. Phytomedicine 12:203–208
Sampath PD, Vijayaraghavan K (2007) Cardioprotective effect of a-mangostin, a xanthone derivative from mangosteen on tissue defense system against isoproterenol-induced myocardial infarction in rats. J Biochem Mol Toxicol 21:336–339
Schito AM, Piatti G, Stauder M, Bisio A, Giacomelli E, Romussi G, Pruzzo C (2011) Effects of demethylfruticuline A and fruticuline A from Salvia corrugata Vahl. on biofilm production in vitro by multiresistant strains of Staphylococcus aureus, Staphylococcus epidermidis and Enterococcus faecalis. Int J Antimicrob Agents 37:129–134
Shankaranarayan D, Gopalakrishnan C, Kameswaran L (1979) Pharmacological profile of mangostin and its derivatives. Arch Int Pharmacol Ther 239:257–269
Shih YW, Chien ST, Chen PS, Lee JH, Wu SH, Yin LT (2010) a-Mangostin suppresses phorbol 12-myristate 13-acetateinduced MMP-2/MMP-9 expressions via avb3 integrin/FAK/ERK and NF-jB signaling pathway in human lung adenocarcinoma A549 cells. Cell Biochem Biophys 58:31–44
Singh R, Ray P, Das A, Sharma M (2010) Penetration of antibiotics through Staphylococcus aureus and Staphylococcus epidermidis biofilms. J Antimicrob Chemother 65:1955–1958
Sivaranjani M, Gowrishankar S, Kamaladevi A, Pandian SK, Balamurugan K, Ravi AV (2016) Morin inhibits biofilm production and reduces the virulence of Listeria monocytogenes—an in vitro and in vivo approach. Int J Food Microbiol 237:73–82
Stepanovic S, Vukovic D, Hola V, Di Bonaventura G, Djukic S, Cirkovic I, Ruzicka F (2007) Quantification of biofilm in microtiter plates: overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS 115:891–899
Suksamrarn S, Komutiban O, Ratananukul P, Chimnoi N, Lartpornmatulee N, Suksamrarn A (2006) Cytotoxic prenylated xanthones from the young fruit of Garcinia mangostana. Chem Pharm Bull 54:301–305
Tenover FC, Biddle JW, Lancaster MV (2001) Increasing resistance to vancomycin and other glycopeptides in Staphylococcus aureus. Emerg Infect Dis 7:327–332
Tew GN, Clements D, Tang H, Arnt L, Scott RW (2006) Antimicrobial activity of an abiotic host defense peptide mimic. Biochim Biophys Acta 1758:1387–1392
Udekwu K, Parrish N, Ankomah P, Baquero F, Levin B (2009) Functional relation-ship between bacterial cell density and the efficacy of antibiotics. J Antimicrob Chemother 63:745–757
Wang JJ, Sanderson BJS, Zhang W (2011) Cytotoxic effect of xanthones from pericarp of the tropical fruit mangosteen (Garcinia mangostana Linn.) on human melanoma cells. Food Chem Toxicol 49:2385–2391
Wang X, Yao X, Zhu Z, Tang T, Dai K, Sadovskaya I, Flahaut S, Jabbouri S (2009) Effect of berberine on Staphylococcus epidermidis biofilm formation. Int J Antimicrob Agents 34:60–66
Ziebuhr W, Hennig S, Eckart M, Kranzler H, Batzilla C, Kozitskaya S (2006) Nosocomial infections by Staphylococcus epidermidis: how a commensal bacterium turns into a pathogen. Int J Antimicrob Agents 28:14–20
Acknowledgements
The authors gratefully acknowledge the Computational and Bioinformatics Facilities provided to Alagappa University by the Department of Biotechnology, Government of India (Bioinformatics Infrastructure Facility; Grant No. BT/BI/25/012/2012). This work was also conducted in part with a research grant from the Department of Biotechnology, Government of India [No.: BT/PR4815/AAQ/3/587/2012]. Financial support rendered in the form of DST-INSPIRE Fellowship [No.: DST/INSPIRE Fellowship/2013/461] to M. Sivaranjani by the Department of Science and Technology, New Delhi is thankfully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Table S1
(PDF 101 kb)
Rights and permissions
About this article
Cite this article
Sivaranjani, M., Prakash, M., Gowrishankar, S. et al. In vitro activity of alpha-mangostin in killing and eradicating Staphylococcus epidermidis RP62A biofilms. Appl Microbiol Biotechnol 101, 3349–3359 (2017). https://doi.org/10.1007/s00253-017-8231-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-017-8231-7