Abstract
Lysins are novel class of anti-infectives which are derived from bacteriophage. In the present study, the potential of previously characterised phage borne endolysin MR-10 in eradicating methicillin-resistant Staphylococcus aureus (MRSA) biofilm was evaluated. Scanning electron microscopic examination showed that both ica-positive and ica-negative MRSA formed equally potent mature biofilm. Different approaches were employed to eradicate the young as well as older biofilm formed by both types of MRSA strains. Our results showed a significant decrease (p < 0.01) in biofilm count on sequentially treating the MRSA biofilm with minocycline (4 μg/ml) for 3 h followed by treatment with endolysin MR-10. Since endolysin can act effectively irrespective of the metabolic status of the cells hence, they are capable of killing the rapidly growing cells (log phase cells) as well as non-dividing (stationary phase) cells. As a result they are effective in eradicating the younger and older biofilm. On staining the ica-positive MRSA biofilm with wheat germ agglutinin (WGA)-Alexa Flour 350, reduction in poly-intercellular adhesion (PIA) content was observed in comparison to control biofilm. In addition, a significant decrease (p < 0.01) in extracellular DNA (eDNA) content of ica-negative MRSA biofilm was also observed. Further, Live/Dead Baclight™ staining also showed presence of higher population of dead cells after treatment with minocycline and endolysin MR-10. Hence, our results showed that using minocycline sequentially with endolysin, MR-10 can effectively eradicate both young as well as older biofilm formed by ica-positive and ica-negative MRSA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus aureus and methicillin-resistant S. aureus infections pose a serious threat to hospital patients. The major risk factor for these nosocomial infections is the extensive use of implanted prosthetic biomaterials for diagnostic and therapeutic purposes, which can be easily colonised by staphylococci giving rise to device-related infections (DVIs) involving biofilm (Pozzi et al. 2012). In addition to its resistance to β-lactam antibiotics such as oxacillin, current chemotherapeutics (involving daptomycin, linezolid) for DVIs have limited effectiveness against biofilm bacteria.
The existence of multiple biofilm forming mechanisms in both S. aureus and methicillin-resistant S. aureus (MRSA) is a major challenge in developing new therapeutics (Beenken et al. 2004; Fitzpatrick et al. 2005; O’Neill et al. 2007). Hence, although the production of PIA or polymeric N-actelyglucosamine (PNAG) synthesised and exported proteins encoded by icaADBC genes is common in majority of clinical isolates, it is evident that MRSA can form biofilm even in the absence of ica-locus as well (Hennig et al. 2007; O’Neill et al. 2008). This mode of biofilm formation depends upon the role of major autolysin (Atl), which helps bacteria in the initial attachment to the substrate, that, in turn, involves fibronectin proteins (FnBPs) promoting subsequent intercellular accumulation and biofilm maturation (O’Neill et al. 2008; Houston et al. 2011). Once formed, biofilm becomes 1000 times more resistant to antibiotics than planktonic cells (Ceri et al. 2001). Hence, along with an urgent requirement for novel antimicrobials, there is an increasing need to look for effective antimicrobial agents which can prevent or eradicate the biofilm formed by the resistant S. aureus strains.
Phage and phage products have emerged as a promising therapeutic candidate in recent years (Lo´pez et al. 2004; Chhibber et al. 2008). Phage lysins, which are produced by dsDNA lytic bacteriophage, have various advantages over antibiotics, such as (1) its rapid killing ability, (2) low probability of development of resistance and (3) lower chance to disrupt normal micro flora due to its host specificity (Schuch et al. 2002; Loessner 2005; Fischetti 2005; Pastagia et al. 2011). Our group previously has reported the efficacy of phage MR-10 in treating diabetic foot infection in mice (Chhibber et al. 2013). However, use of endolysins has various advantages over using whole bacteriophage. In case of usage of whole phage, resistance arising from adsorption, restriction modification or abortive infection has been reported in various genera (Schuch et al. 2013). Bacteriophages have coevolved with their hosts over millions of years, and this equilibrium has been maintained by developing resistance and counter resistance. On the contrary, there have been no reports of development of resistance in bacteria even after growth in the presence of sub-lethal doses of endolysin and after repeated exposures (Schuch et al. 2002). In addition, the risk of horizontal gene transfer can be avoided by using endolysin instead of whole bacteriophage. Also, phage preparations may contain endotoxins or exotoxins produced by their bacterial hosts that may prove to be detrimental for the host. To date, a number of phage lysins have been described which demonstrate activity against staphylococci including LysK (O’Flaherty et al. 2005), LysWMY (Yokoi et al. 2005), Φ11 lysin (Sass and Bierbaum 2007), MV-L (Rashel et al. 2007), LysH5 (Obeso et al. 2008, LysGH15 (Gu et al. 2011), PlyV12 (Yoong et al. 2004), SAP-2 (Son et al. 2010) and SAL-1 (Jun et al. 2011). This is the first report on phage borne endolysin where it has been used to eradicate mature biofilm produced by MRSA. Hence, in the present, the efficacy of phage borne endolysin (derived from previously characterised MR-10 phage) was evaluated in eradicating young and old biofilm produced by both types of MRSA (ica-positive and ica-negative), alone or in conjunction with antibiotic.
Materials and methods
Bacterial strains
Methicillin-resistant S. aureus ATCC 33591 and ATCC 43300 (an MRSA strain) procured from American Type Culture Collection Centre, Manassas, Virginia, USA and available in our laboratory were used in the present study. All the strains were preserved in semi-solid agar stabs at 4 °C and in brain heart infusion broth with 15 % glycerol at −70 °C until further use.
Antimicrobial agents
Minocycline, a broad range tetracycline was procured from Sigma-Aldrich, St. Louis, MO, USA. Endolysin MR-10 was purified from previously characterised phage MR-10 (Chhibber et al. 2013). Firstly, the endolysin was extracted from the phage following the method described by Adams and Park (1956) and further purified by using ion exchange chromatography (DEAE-Sepharose) and gel chromatography. Briefly, the crude enzyme was applied to column packed with Tris–HCl (0.2 M, pH 7.2) equilibrated DEAE-Sepharose. The bound enzyme was eluted using a gradient (0.1–1 M NaCl). The fractions showing lytic activity were pooled, concentrated and then applied onto Sephadex G-100 for further purification. Thereafter, the elution was done using Tris–HCl (0.2 M, pH 7.2). Enzyme purification was confirmed by SDS-PAGE analysis at each step.
Phage MR-10 is available in our laboratory, and corresponding author can be contacted, if required.
Biofilm development
MRSA biofilm was grown in 96-well microtitre plate according to the modified method of Bedi et al. (2009). Briefly, wells of microtitre plate were inoculated with 50 μl of brain heart infusion (BHI) [beef heart (5 g/l), calf brains (12.5 g/l), disodium hydrogen sulphate (2.5 g/l), D (+) glucose (2 g/l), peptone (10 g/l), NaCl (5 g/l)] broth and 50 μl of bacterial culture (OD600 = 0.3) equivalent to 108 CFU ml−1 of bacteria and incubated at 37 °C overnight. In each test, control wells containing sterile broth were included as plate sterility control. After incubation, planktonic cells in the fluid were removed and wells were washed thoroughly three times with normal saline (NS; 0.85 % NaCl). The biofilm matrix was then scraped with a sterile pipette tip, suspended in NS and vortexed for 3 min. Microbial load of biofilm was enumerated by viable cell counting.
For the establishment of 7-day-old biofilm, spent medium was replaced with fresh sterile BHI in the rest of the wells and plate was reincubated at 37 °C overnight. Media in each well was replaced every 24 h until the seventh day of the experiment. Microbial load of the biofilm was enumerated daily by viable cell count method till 7 days.
Biofilm was also developed on glass coverslips (18 mm × 18 mm; 0.08–0.12 mm; Corning Glass, Corning, NY, USA). Biofilm on glass coverslips was grown by the tip box batch culture method of Hughes et al. (1998). Biofilms were allowed to grow at air–liquid interface. Tip box mounted coverslips and the nutrient broth were sterilised separately. A 100 ml bacterial culture (108 CFU ml−1) was added to the broth, which was then poured into the tip box. The whole setup was incubated at 37 °C. The desired number of coverslips were removed and used. Spent growth medium in the culture box was replaced every 24 h.
Scanning electron microscopy
The morphological characteristics of mature biofilm formed by both ica-negative as well as ica-positive MRSA were observed by scanning electron microscopy. The mature biofilm grown on coverslips were fixed with 2.5 % gluteraldehyde (pH 7.2) at room temperature overnight. This was followed by three washings using phosphate-buffered saline (PBS, 0.1 M, pH 7.2) for 15 min each followed by series of ethanol solutions (50 %, 10 min; 70 %, 10 min; 80 %, 15 min; 90 %, 15 min; and 100 %, 20 min). The specimens were then critical point dried, coated with gold and observed under scanning electron microscopy (SEM; Jeol JSM-6100, JEOL Ltd., Tokyo, Japan).
Optimum endolysin concentration for treating MRSA biofilm
The maximum activity of endolysin MR-10 in eradicating both the MRSA biofilm was assessed. Briefly, biofilm were established for 7 days as described above. On each day, 100 μl of endolysin MR-10 (final concentration of 9, 18 and 36 μg/ml, respectively) was added in separate wells. At regular intervals of time (3, 6 and 24 h), the contents in well were removed and adequately washed. After washing, biofilm was scrapped using sterile micropipette tip. The withdrawn samples were vortexed for 3 min and cell count enumerated by viable cell count method.
Treatment of preformed MRSA biofilms
The MRSA biofilms were treated with endolysin MR-10 and minocycline in the following ways:
-
(a) Concomitant treatment with endolysin and antibiotic:
The biofilm were grown for 7 days as described above. On each subsequent day, equal volume (100 μl) of minocycline and endolysin MR-10 was added to the well, which was to be tested. (For example on day 1, combination of antibiotic and endolysin was added to well having 1-day-old biofilm; on day 2, antibiotic was added to well having 2-day-old biofilm and so on). For ica-negative MRSA biofilm, the final concentration of 18 μg/ml and for ica-positive MRSA biofilm the final concentration of 36 μg/ml of endolysin were used for treatment. Minocycline was added at its serum achievable concentration, i.e., 4 μg/ml. After overnight treatment, viable count was enumerated using drop plate method (Miles et al. 1938). Experiments were performed in duplicate.
-
(b) Sequential treatment 1 with endolysin and minocycline:
7-day biofilm was grown as described above. The sequential treatment to the biofilm on each day was given with endolysin MR-10 and minocycline. Each day, the biofilm was first treated for 6 h with 100 μl of endolysin MR-10 (final concentration of 18 μg/ml for ica-negative MRSA biofilms and 36 μg/ml for ica-positive MRSA biofilms). After 6 h of exposure, endolysin was aspirated from well followed by three washings with normal saline. Thereafter, 100 μl of minocycline (final concentration of 4 μg/ml) was added to the wells and incubated at 37 °C overnight. On the following day, the antibiotic was aspirated from the wells followed by three washings with normal saline. The remaining adhered biofilm was scrapped using sterile micropipette. The samples withdrawn were vortexed for 3 min. The viable biofilm cell count was enumerated using drop plate method (Miles et al. 1938).
-
(c) Sequential treatment 2 with minocycline and endolysin:
As described above, the biofilm was grown for 7 days. All the conditions were similar as described under sequential treatment above except that in this experiment, each day, 100 μl of minocycline was first added to the wells for 3 h followed by 100 μl of endolysin MR-10 to the wells after appropriate washings and incubated overnight at 37 °C. On the following day, the endolysin was aspirated from the wells followed by three washings with normal saline. The remaining adhered biofilm was scrapped using sterile micropipette. The number of viable bacteria in the withdrawn samples was determined by drop plate method (Miles et al. 1938).
Detection of PIA in ica-positive MRSA biofilm
The presence of PIA in control as well as treated ica-positive MRSA biofilm was detected by using fluorescence microscopy. The biofilm was grown on coverslips as described above. The test coverslips were treated according to the method explained above in sequential treatment 2. Thereafter, both control and treated coverslips were stained with wheat germ agglutinin (WGA) conjugated to Alexa Fluor 350 [Molecular probes, Eugene, OR, USA] (WGA-Alexa Fluor 350, 0.1 mg/ml) for 15 min in the dark, washed twice with PBS (0.1 M, pH 7.2) and viewed under an Olympus BX51 [Olympus America Inc., Melville, NY, USA] fluorescence microscope using a 40× objective lens (Singh et al. 2010). Experiments were performed in duplicate, and four randomly chosen spots were analysed per sample.
Quantitation of eDNA in ica-negative MRSA biofilm
The amount of eDNA was quantified in ica-negative MRSA biofilm by the method of Vilain et al. (2009). Briefly, biofilm was established in microtitre plates as described above. Each day, the wells were washed three times with NS. The biofilm cells were scraped from control and treated wells and centrifuged at 10,000 rpm for 10 min at 4 °C. The supernatant was filtered using 0.45-mm syringe filter [EMD Millipore, Billerica, MA, USA] to remove all the bacterial cells. The amount of eDNA present in the supernatant was assessed by measuring O.D260 using UV Nanodrop 1000 [Thermo Fisher Scientific Inc., Waltham, MA, USA].
Fluorescence microscopy of MRSA biofilm using Live/DeadTM BacLight kit
Both ica-positive and ica-negative MRSA biofilm were grown on coverslips as described above. Both control and treated coverslips were stained using Live/DeadTM Baclight kit [Molecular Probes, Eugene, OR, USA]. Briefly, both Syto9 and propidium iodide were mixed in a ratio 1:1 in PBS (0.1 M, pH 7.2). The coverslips were stained with 50 μl of mixed dye for 15 min in the dark followed by two washings with PBS (0.1 M, pH 7.2) and viewed under an Olympus BX51 [Olympus America Inc., Melville, NY, USA] fluorescence microscope.
Statistical analysis
The data is expressed as mean ± standard deviation of replicated values where indicated. The bacterial count was converted to log10. The effect of different treatments on biofilm eradication was evaluated by two-way analysis of variance (ANOVA) and Student’s t test using Microsoft Excel Programme 2011. p values less than 0.01 were considered statistically significant.
Results
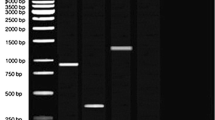
Morphological characteristics of biofilm
The biofilm developed on coverslips were observed under electron microscope (SEM) for direct visualisation of mature biofilm formed. The ica-positive MRSA biofilm was observed on the third day (i.e., peak day) and ica-negative MRSA biofilm on the fifth day of incubation. Upon SEM analysis, both MRSA biofilms showed all the three indicators of a mature biofilm, including presence of extracellular matrix, 3days structure as well as possible water channels. As it is evident from Fig. 1a, both ica-negative MRSA as well as ica-positive MRSA biofilms were equally dense and showed all the indicators of a mature biofilm (Fig. 1b).
Endolysin activity on MRSA biofilm
Various concentrations of endolysin were used for biofilm treatment. When, ica-negative MRSA biofilm of different days were treated with 9 μg/ml of enzyme, after 3 h of treatment, an insignificant reduction (p > 0.01) of 0.41 ± 0.09 was observed in bacterial count on different days (Table 1). Similarly, on increasing the duration of treatment, no significant reduction (p > 0.01) in bacterial count was observed. Further, increase in enzyme concentration to 18 μg/ml, an exposure of 6 h showed a significant reduction of ~1.1 logs (p < 0.01). However, no significant decrease (p > 0.01) in bacterial count was observed on further increasing the enzyme concentration and duration of treatment. On the other hand, treatment of ica-positive MRSA biofilm with 36 μg/ml of enzyme for 6 h showed significant decrease (p < 0.01) in bacterial count up to ~1.18 logs on different days (Table 2). No significant change in bacterial count (p > 0.01) was observed on increasing the exposure time to 24 h.
Combined treatment with endolysin MR-10 and minocycline
Both the biofilms were treated concomitantly with equal volumes of endolysin MR-10 and minocycline. As shown in Fig. 2a, a significant decrease (p < 0.01) in biofilm cells was observed from day 1 to day 3 (1.17 logs, 1.31 logs and 1.77 logs). However, no significant decrease (p > 0.01) in the biofilm cells was observed from day 4 onwards. Similarly, on treating ica-positive MRSA biofilm (Fig. 2b) with endolysin and minocycline, no significant decrease (p > 0.01) in the biofilm cell number was observed (i.e., a log reduction of 0.99 logs, 0.6 logs and 0.62 logs on day 5, 6 and 7, respectively).
Sequential treatment of MRSA biofilm
MRSA biofilm was subjected to sequential treatment with endolysin MR-10 and minocycline. In the first case, both the biofilms were exposed to endolysin for 6 h, and thereafter, they were treated overnight with minocycline (sequential treatment 1 (S.T.-1)). In the second case, the biofilm were first treated with minocycline and thereafter exposed to endolysin MR-10 overnight. For ica-negative MRSA biofilm, endolysin MR-10 was added at a final concentration of 18 μg/ml. As shown in Fig. 3a, sequential treatment 2 (S.T.-2) treatment as compared to control showed a significant decrease (p < 0.01) of 2.22 logs on the peak day (fifth day). In comparison to S.T.-1, S.T.-2 showed a significant decrease (p < 0.01) of 2.33 and 1.98 logs on days 6 and 7. These results confirmed that maximum decrease in mature biofilm count was seen with treatment 2 (S.T.-2) as compared to treatment 1 (S.T.-1).
a Sequential treatment of ica-negative MRSA biofilms. S.T.-1 depicts endolysin (18 μg/ml) treatment followed by minocycline (4 μg/ml); S.T.-2: minocycline (4 μg/ml) followed by endolysin MR-10 (18 μg/ml). b Sequential treatment of ica-positive MRSA biofilms. S.T.-1 depicts endolysin (36 μg/ml) treatment followed by minocycline (4 μg/ml); S.T.-2: minocycline (4 μg/ml) followed by endolysin MR-10 (36 μg/ml)
For the treatment of ica-positive MRSA biofilm, endolysin MR-10 was added at a final concentration of 36 μg/ml. In S.T.-2, a significant decrease (p < 0.01) of 2.11 logs was observed on peak day (the third day) whereas in S.T.-1, a significant decrease (p < 0.01) of 1.75 logs was observed on the peak day (Fig. 3b). In comparison to control, S.T.-2 showed a significant decrease (p < 0.01) of 2.14, 2.02 and 1.75 logs on days 5, 6 and 7. However, no significant decrease (p > 0.01) was observed on day 6 and day 7 in case of S.T.-1.
Live dead staining of MRSA biofilm
Both MRSA biofilms were stained using Live/Dead Baclight kit in order to observe live and dead cells. As shown in Fig. 4(a) and (b), majority of the cells in both the biofilm were observed to be live (stained green) before treatment. However, majority of biofilm cells were found to be dead (stained red) following sequential treatment with minocycline and endolysin (S.T.-2). The biofilm formed by ica-positive MRSA was observed to be denser in comparison to ica-negative MRSA, but there was no difference in overall distribution of live and dead cells. The biofilm treated on day 7 showed both live as well as dead cells evenly distributed in the biofilm.
Microscopic analysis of PIA in treated and untreated ica-positive MRSA biofilm
PIA is a major constituent of the biofilm matrix in ica-positive MRSA. Hence, the effect of sequential treatment (S.T.-2) on PIA content of the biofilm was evaluated. The biofilm were stained with WGA-conjugated to Alexa Flour 350 and observed under fluorescence microscope. As shown in Fig. 5, the amount of PIA in treated biofilm was found to be less in comparison to untreated biofilm. The treated biofilm showed much less amount of PIA on all days following treatment. Compared to this, untreated biofilm showed dense PIA up to day 7.
Quantitation of eDNA in treated ica-negative MRSA biofilm
eDNA is the major constituent of ica-negative MRSA biofilm matrix. The amount of eDNA release from ica-negative MRSA biofilm was quantitated for 7 days after the sequential treatment (S.T.-2). Our results showed a significant decrease (p < 0.01) in eDNA content in the treated biofilm in comparison to control from day 1. A significant decrease (p < 0.01) of 79.9 and 62.87 units was observed on days 1 and 5 (peak day) respectively (Table 3). In comparison to control, a significant decrease (p < 0.01) of 41.63 and 34.10 units, respectively, was observed on days 6 and 7.
Discussion
Biofilm are multi-layered communities of sessile cells protected by extracellular matrix, which often adhere to damaged tissue or indwelling medical devices (Archer et al. 2011). These biofilms are difficult to eradicate using the conventional as well as newer antibiotics due to its altered metabolic activity as well as presence of extracellular matrix, which is difficult to penetrate (Rani et al. 2007; Brady et al. 2007). In the present study, an attempt was made to eradicate the biofilm formed by MRSA, possessing or lacking ica-locus. Though previous researchers have attempted to eradicate 1-day-old biofilm formed by various pathogenic organisms such as S. aureus, Staphylococcus epidermidis and Staphylococcus pneumonia (Loeffler et al. 2001; Daniel et al. 2010), no literature is available in which the efficacy of endolysin alone or in conjunction with antibiotics has been evaluated in eradicating 7-day-old biofilm. It is evident from the previous literature that biofilm age is a major decisive factor in determining the effectiveness of any antibiofilm agent (Sedlacek and Walker 2007; Ito et al. 2009). Previously, in our laboratory, we have reported that young biofilm formed by ica-negative and ica-positive MRSA can be eradicated by using minocycline alone at its highest clinically achievable concentration. However, as the biofilm grows older, this serum achievable concentration becomes ineffective in eradicating the biofilm (Chopra et al. 2014).
Scanning electron microscopy was done to elucidate the structure of the biofilm formed by both the strains. The mature biofilm formed by the MRSA strains were more or less similar in structure. They were equally dense and contained the apt morphology of the mature biofilm such as 3-D structure, possible water channels and dense matrix. Previous researchers have shown that lack of ica-locus results in the formation of weak biofilm by ica-negative MRSA strains (Leriche et al. 2000). But, the results of this study confirm that the biofilm formed by both the strains were similar in morphology as well as in resistance to antibiotics. However, ica-negative MRSA achieved its peak on the fifth day whereas ica-positive MRSA achieved its peak on the third day (Chopra et al. 2014).
The optimum concentration for eradicating ica-negative MRSA biofilm was found to be 18 μg/ml whereas for ica-positive MRSA biofilm was 36 μg/ml. The above-mentioned concentrations were quite effective in eradicating the young biofilm formed by both the strains. However, none of the used concentration was effective in eradicating the mature biofilm. Hence, minocycline was selected for use at its highest clinically achievable concentration in conjunction with endolysin MR-10 in order to eradicate both young as well as mature biofilm.
In this context, first of all, the combination treatment was tested. In this case, both the MRSA biofilms were treated overnight with equal ratios of endolysin MR-10 and minocycline (4 μg/ml). No significant decrease was observed in the cell count of old biofilm. Possibly, it could be because both minocycline as well as endolysin MR-10 acted simultaneously on the upper layers of biofilm without reaching the interior. It is evident from previous literature that antibiotics cannot penetrate deep into a biofilm due to complex biofilm matrix structure. However, according to Loessner et al. (2002), endolysins are ‘one use’ enzymes, i.e., they bind irreversibly to its substrate and cannot disengage themselves once they bind to peptidoglycan. Hence, it is likely that both minocycline as well as endolysin MR-10 acted on the same repertoire of cells but on different domains at the same time resulting in less activity when used in combination.
The biofilm were also exposed sequentially to endolysin MR-10 and minocycline (4 μg/ml). In sequential treatment 1, the biofilm were first exposed to endolysin MR-10 for 6 h and further treated overnight with minocycline. The results showed that in comparison to concomitant treatment, a significant decrease in the cell count of young biofilm was observed in the MRSA biofilm. In addition, a decrease in count of mature biofilm was also observed to some extent. Endolysin MR-10 could effectively kill the bacterial cells on application, but the action of minocycline was limited because these tetracyclines (minocycline) are known to inhibit protein synthesis in bacterial cells (Cerca 2005). It is likely that use of minocycline after endolysin treatment failed due to lack of metabolically active cells in mature biofilm.
On the contrary, in the sequential treatment 2, the biofilm was first exposed to minocycline for 3 h and thereafter treated with endolysin MR-10 overnight. This strategy showed significant decrease in the cell count of young as well as mature biofilm. The reason for the success of this strategy probably is due to the fact that minocycline was able to effectively eradicate metabolically active cells. According to information available in literature, biofilm cells present in the upper layers are metabolically active in comparison to biofilm cells present in deeper layers. Hence, the biofilm cells present in the upper layers were effectively eradicated by minocycline due to its ability to inhibit the protein synthesis machinery of the cells (Cerca 2005). On the other hand, endolysins can act effectively irrespective of metabolic status of cells, killing both rapidly growing cells (log phase cells) as well as non-dividing (stationary phase) cells. Moreover, since endolysins are low molecular weight enzymes, they can penetrate more effectively into deeper layers of biofilm as compared to antibiotics. Their penetration into the deeper layers is probably facilitated due to the presence of different binding and catalytic domains. This has been reported previously, that endolysin catalytic domains can help it in its penetration into the biofilm (Shen et al. 2013). To further confirm our findings, MRSA treated and untreated biofilm were stained using fluorescent dyes. Syto9 evidently stains the live cells whereas propidium iodide stains the dead cells on the basis of altered cell permeability. The staining results also confirmed that majority of mature cells were killed on using the sequential treatment with minocycline for 3 h followed by endolysin MR-10 overnight.
The extracellular matrix imparts resistance to the biofilm against various environmental factors including antibiotics (Otto 2008). As described by previous researchers, PIA forms the extracellular matrix of ica-positive MRSA biofilm whereas eDNA is the major constituent of extracellular matrix of ica-negative MRSA biofilm (Arciola et al. 2012; Fischer et al. 2014). Hence, our interest was to investigate the effect of this sequential treatment on the amount of PIA and eDNA. On staining the ica-positive MRSA biofilm (treated/untreated) with WGA-conjugated to Alexa Flour 350, we observed less amount of PIA present in the treated biofilm in comparison to untreated biofilm. Although endolysin could not act on PIA directly, it is known that PIA is covalently linked to the cell wall of S. aureus (Vergara-Irigaray et al. 2008). Hence, due to rapid degradation of cell wall by the action of endolysin, PIA could not bind to peptidoglycan resulting in the presence of fewer matrixes in the treated biofilm. Similarly, on quantitating the amount of eDNA in ica-negative MRSA biofilm, a significant decrease in the eDNA content was also observed. The eDNA is produced by the autolytic activity of the cell wall associated enzymes in S. aureus. The bacterial cell undergoes automated cell death due to the action of these autolytic enzymes present in the cell wall resulting in the release of DNA from the cells. This, in turn, imparts matrix to ica-negative MRSA biofilm and termed as eDNA (Yamada et al. 2001; Ledala et al. 2006). Hence, absence of bacterial cells and decrease in cell wall-associated enzymes resulted in the decrease of eDNA content in treated biofilm.
The present study highlights the potential of endolysin MR-10 as highly potent antimicrobial agent in eradicating not only the young biofilm but older biofilm as well. Its mode of action, which is unlike antibiotics, does not requires the metabolic machinery of the cell as it targets the peptidoglycan, which is an integral part of the bacteria. Further, its high specificity and rapid killing efficacy prove it to be a promising candidate in eradicating biofilm, which often become difficult to treat after certain time. Thus, on the basis of our study, it can be speculated that endolysin MR-10 in conjunction with minocycline can effectively eradicate biofilm formed by both types of MRSA strains.
References
Adams MH, Park BH (1956) An enzyme produced by a phage -host cell system. II. the properties of polysachharide depolymerase. Virol 2:719–736
Archer NK, Mazaitis MJ, Costerton WJ, Leid JG, Powers ME, Shirtliff ME (2011) Staphylococcus aureus biofilms: properties, regulation and roles in human disease. Virulence 2(5):445–459
Arciola CR, Campoccia D, Speziale P, Costerton JW, Montanaro L (2012) Biofilm formation in Staphylococcus implants infections. a review of molecular mechanisms and implications for biofilm-resistant materials. Biomaterials 33:5967–5982
Bedi MS, Verma V, Chhibber S (2009) Amoxicillin and specific bacteriophage can be used together for eradication of biofilm of Klebsiella pneumoniae B5055. World J Microbiol Biotechnol 25:1145–1151
Beenken KE, Dunman PM, McAleese F, Macapagal D, Murphy E, Projan SJ, Blevins JS, Smeltzer MS (2004) Global gene expression in Staphylococcus aureus biofilms. J Bacteriol 186:4665–4684
Brady RA, Leid JG, Kofonow J, Costerton JW, Shirtliff ME (2007) Immunoglobulins to surface-associated biofilm immunogens provide a novel means of visualization of methicillin-resistant Staphylococcus aureus biofilms. Appl Environ Microbiol 73:6612–6619
Cerca N (2005) Comparative assessment of antibiotic susceptibility of coagulase negative staphylococci in biofilm versus planktonic culture as assessed by bacterial enumeration nor rapid XTT colorimetry. J Antimicrob Chemother 56:331–336
Ceri H, Olson M, Morck D, Storey D, Read R, Buret A, Olson B (2001) The MBEC assay system: multiple equivalent biofilms for antibiotic and biocide susceptibility testing. Methods Enzymol 337:377–385
Chhibber S, Kaur T, Kaur S (2013) Co-therapy using lytic bacteriophage and linezolid: effective treatment in eliminating methicillin resistant Staphylococcus aureus (MRSA) from diabetic foot infections. PLoS ONE 8(2):e56022
Chopra S, Harjai K, Chhibber S (2014) Antibiotic susceptibility of ica-positive and ica-negative MRSA biofilms in different phases of biofilm growth. J Antibiot doi:10.1038/ja.2014.96
Daniel A, Euler C, Collin M, Chahales P, Gorelick KJ, Fischetti VA (2010) Synergism between a novel chimeric lysin and oxacillin protects against infection by methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 54:1603–1612
Fischer A, Kambara K, Meyer H, Stenz L, Bonetti EJ, Girard M, Lalk M, Francois P, Schrenzel J (2014) GdpS contributes to Staphylococcus aureus biofilm formation by regulation of eDNA release. Int J Med Microbiol 304:284–299
Fischetti VA (2005) Bacteriophage lytic enzymes: novel anti infectives. Trends Microbiol 13(10):491–496
Fitzpatrick F, Humphreys H, O’Gara JP (2005) Evidence for icaADBC independent biofilm development mechanism in methicillin-resistant Staphylococcus aureus clinical isolates. J Clin Microbiol 43:1973–1976
Gu J, Xu W, Lei L, Huang J, Feng X, Sun C, Du C, Zuo J, Li Y, Du T, Li L, Han W (2011) LysGH15, a novel bacteriophage lysin, protects a murine bacteremia model efficiently against lethal methicillin-resistant Staphylococcus aureus infection. J Clin Microbiol 49(1):111–117
Hennig S, NyuntWai S, Ziebuhr W (2007) Spontaneous switch to PIA independent biofilm formation in an ica-positive Staphylococcus epidermidis isolate. Int J Med Microbiol 297:117–122
Houston P, Rowe SE, Pozzi C, Waters EM, O’Gara JP (2011) Essential role for the major autolysin in the fibronectin-binding protein-mediated Staphylococcus aureus biofilm phenotype. Infect Immun 79:1153–1165
Hughes KA, Sutherland IW, Clark J, Jones MV (1998) Biofilm susceptibility to bacteriophage attack: the role of phage-borne polysaccharide depolymerase. Microbiology 144:3039–3047
Ito A, Taniuchi A, May T, Kawata K, Okabe S (2009) Increased antibiotic resistance of Escherichia coli in mature biofilms. Appl Environ Microbiol 75:4093–4100
Jun SY, Jung GM, Son JS, Yoon SJ, Choi YJ, Kang SH (2011) Comparison of the antibacterial properties of phage endolysins SAL-1 and LysK. Antimicrob Agents Chemother 55(4):1764–1767
Ledala N, Wilkinson BJ, Jayaswal RK (2006) Effects of oxacillin and tetracycline on autolysis, autolysin processing and atl transcription in Staphylococcus aureus. Int J Antimicrob Agents 27:518–524
Leriche V, Sibille P, Carpentier B (2000) Use of an enzyme linked lectinosorbent assay to monitor the shift in polysachharide composition in bacterial biofilms. Appl Environ Microbiol 66:1851–1856
Loeffler JM, Nelson D, Fischetti VA (2001) Rapid killing of Streptococcus pneumoniae with a bacteriophage cell wall hydrolase. Science 294:2170–2172
Loessner MJ (2005) Bacteriophage endolysins—current state of research and applications. Curr Opin Microbiol 8(4):480–487
Loessner MJ, Kramer K, Ebel F, Scherer S (2002) C-terminal domains of Listeria monocytogenes bacteriophage murein hydrolases determine specific recognition and high-affinity binding to bacterial cell wall carbohydrates. Mol Microbiol 44:335–349
Lopez R, Garcıa E, Garcıa P (2004) Enzymes for anti-infective therapy: phage lysins. Drug Discov Today Ther Strateg 1(4):469–474
Miles AA, Misra SS, Irwin JO (1938) The estimation of the bactericidal power of the blood. J Hyg (Lond) 38:732–749
O’Flaherty S, Coffey A, Meaney W, Fitzgerald GF, Ross RP (2005) The recombinant phage lysinLysK has a broad spectrum of lytic activity against clinically relevant staphylococci, including methicillin-resistant Staphylococcus aureus. J Bacteriol 187:7161–7164
O’Neill E, Pozzi C, Houston P, Smyth D, Humphreys H, Robinson A, O’Gara JP (2007) Association between methicillin susceptibility and biofilm regulation in Staphylococcus aureus isolates from device-related infections. J Clin Microbiol 45:1379–1388
O’Neill E, Pozzi C, Houston P, Humphreys H, Robinson DA, Loughman A, Foster TJ, O’Gara JP (2008) A novel Staphylococcus aureus biofilm phenotype mediated by the fibronectin-binding proteins, FnBPA and FnBPB. J Bacteriol 190:3835–3850
Obeso JM, Martınez B, Rodrıguez A, Garcıa P (2008) Lytic activity of the recombinant staphylococcal bacteriophage phiH5 endolysin active against Staphylococcus aureus in milk. Int J Food Microbiol 128(2):211–218
Otto M (2008) Staphylococcal biofilms. Curr Top Microbiol Immunol 322:207–228
Pastagia M, Euler C, Chahales P, Fuentes-Duculan KJG, Fischetti VA (2011) A novel chimeric lysin shows superiority to mupirocin for skin decolonization of methicillin resistant and -sensitive Staphylococcus aureus strains. Antimicrob Agents Chemother 55(2):738–744
Pozzi C, Waters EM, Rudkin JK, Schaeffer CR, Lohan AJ, Tong P, Loftus BJ, Pier GB, Fey PD, Massey RC, O’Gara JP (2012) Methicillin resistance alters the biofilm phenotype and attenuates virulence in Staphylococcus aureus device-associated infections. PLoS Pathog 8(4):e1002626
Rani SA, Pitts B, Beyenal H, Veluchamy RA, Lewandowski Z, Davison WM, Buckingham-Meyer K, Stewart PS (2007) Spatial patterns of DNA replication, protein synthesis and oxygen concentration within bacterial biofilms reveal diverse physiological states. J Bacteriol 189:4223–4233
Rashel M, Uchiyama J, Ujihara T, Uehara Y, Kuramoto S, Sugihara S, Yagyu K, Muraoka A, Sugoi M, Hiramatsu K, Honke K, Matsuzaki S (2007) Efficient elimination of multidrug resistant Staphylococcus aureus by cloned lysin derived from bacteriophage ΦMR11. J Infect Dis 196:1237–1247
Sass P, Bierbaum G (2007) Lytic activity of recombinant bacteriophage phi11 and phi12 endolysins on whole cells and biofilms of Staphylococcus aureus. Appl Environ Microbiol 73:347–352
Schuch R, Nelson D, Fischetti VA (2002) A bacteriolytic agent that detects and kills Bacillus anthracis. Nature 418:884–889
Schuch R, Pelzek AJ, Raz A, Euler CW, Ryan PA, Winer BY, Farnsworth A, Bhaskaran SS, Stebblins CE, Xu Y, Clifford A, Bearss DJ, Vankayalapati H, Goldberg AR, Fischetti VA (2013) Use of a bacteriophage lysin to identify a novel target for antimicrobial development. PLoS ONE 8(4):e60754
Sedlacek MJ, Walker C (2007) Antibiotic resistance in an in vitro subgingival biofilm model. Oral Microbiol Immunol 22:333–339
Shen Y, Ko¨ller T, Kreikemeyer B, Nelson DC (2013) Rapid degradation of Streptococcus pyogenes biofilms by PlyC, a bacteriophage-encoded endolysin. J Antimicrob Chemother 68(8):1818–1824
Singh R, Ray P, Das A, Sharma M (2010) Enhanced production of exopolysaccharide matrix and biofilm by a menadione-auxotrophic Staphylococcus aureus small-colony variant. J Med Microbiol 59:521–527
Son JS, Lee SJ, Jun SY, Yoon SJ, Kang SH, Paik HR, Kang JO, Choi YJ (2010) Antibacterial and biofilm removal activity of a podoviridae Staphylococcus aureus bacteriophage SAP-2 and a derived recombinant cell-wall-degrading enzyme. Appl Microbiol Biotechnol 86(5):1439–1449
Vergara-Irigaray M, Maira-Litra´n T, Merino N, Pier GB, JR P´ s, Lasa I (2008) Wall teichoic acids are dispensable for anchoring the PNAG exopolysaccharide to the Staphylococcus aureus cell surface. Microbiology 154:865–877
Vilain S, Pretorius JM, Theron J, Broz¨el VS (2009) DNA as an adhesin: Bacillus cereus requires extracellular DNA to form biofilms. Appl Environ Microbiol 75:2861–2868
Yamada S, Sugai M, Komatsuzawa H, Matsumato A (2001) Suppressed localisation of a major autolysin on Staphylococcus aureus treated with tetracycline. J Electron Microsc 50:359–364
Yokoi KJ, Kawahigashi N, Uchida M, Sugahara K, Shinohara M, Kawasaki KI (2005) The two-component cell lysis genes holWMY and lysWMY of the Staphylococcus warneri M phage WMY: cloning, sequencing, expression and mutational analysis in Escherichia coli. Gene 351:97–108
Yoong P, Schuch R, Nelson D, Fischetti VA (2004) Identification of a broadly active phage lytic enzyme with lethal activity against antibiotic-resistant Enterococcus faecalis and Enterococcus faecium. J Bacteriol 186(14):4808–4812
Conflict of interest
No conflict of interest associated with the present manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chopra, S., Harjai, K. & Chhibber, S. Potential of sequential treatment with minocycline and S. aureus specific phage lysin in eradication of MRSA biofilms: an in vitro study. Appl Microbiol Biotechnol 99, 3201–3210 (2015). https://doi.org/10.1007/s00253-015-6460-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-015-6460-1