Abstract
Fungal metabolites (mycotoxins) that pose a health hazard to humans and animals have long been known to be associated with mold-contaminated food and feed. In recent times, concerns have been raised about exposures to mycotoxin-producing fungi in indoor environments, e.g., damp homes and buildings. The principal mycotoxins that contaminate food and feed (alfatoxins, fumonisins, ochratoxin A, deoxynivalenol, zearalenone) are rarely if ever found in indoor environments, but their toxicological properties provide an insight into the difficulties of assessing the health effects of related mycotoxins produced by indoor molds. Although the Penicillium and Aspergillus genera of fungi are major contaminants of both food and feed products and damp buildings, the particular species and hence the array of mycotoxins are quite different in these environments. The mycotoxins of these indoor species and less common mycotoxins from Stachybotrys and Chaetomium fungi are discussed in terms of their health effects and the need for relevant biomarkers and long-term chronic exposure studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mycotoxins are low molecular weight (generally <1 kDa) natural products (secondary metabolites) produced by filamentous fungi or molds. Although such fungi produce an enormous array of secondary metabolites, including antibiotics and other pharmaceuticals, the term mycotoxin is restricted to those secondary metabolites that pose a potential health risk to animals and humans exposed to these natural products, through contamination of our feed and food (Bennett and Klich 2003). Inhalation exposure to spore and hyphal fragments and whole spores may cause allergic, infectious, toxic disease depending on the nature of the fungi, the extent of exposure the health status of the animal or person (National Academy of Sciences 2004). Allergic responses (asthma, allergic rhinitis, hypersensitivity pneumonitis) are the most common medical problems associated with inhalation exposure to fungi.
Exposure to mycotoxins may result in a variety of illnesses that fall under the heading of mycotoxicosis from ingestion , in occupational circumstances, from dermal and inhalation exposure. Mycotoxins may be categorized in a variety of ways depending upon whether you are a chemist (structure-based classifications), a biologist (taxonomy of the producing fungi) or a toxicologist/physician (tissue, cellular responses, disease condition). There are literally thousands of compounds that have been isolated from cultures of thousands of fungal taxa that are toxic in some assay, usually a cell bioassay (Cole and Cox 1981; Cole et al. 2003). However, it is important to keep in mind that the vast majority of these compounds have not been implicated directly in animal or human toxicoses and that their “toxic” properties have been illuminated only through in vitro cell bioassays.
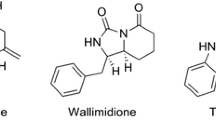
In agriculture, where most of our knowledge and experience with mycotoxins are derived, there are five important mycotoxins: alfatoxins, ochratoxin A, fumonisins, deoxynivalenol, and zearalenone (Fig. 1; Miller 1999). These toxins are stable during food production and are potently toxic. The fungi that produce these mycotoxins are various species of Aspergillus, Penicillium, and Fusarium, but mycotoxin production is restricted to only a few species within these genera.
The World Health Organization/Food and Agricultural Organization of the United Nations have produced tolerable daily intakes for the first four of these mycotoxins (JECFA 2002) that are valid for international trade. This reflects the very large toxicological database on these mycotoxins derived from experiments with laboratory animals, from case studies (animals and humans), and from epidemiological data for people exposed to these compounds in their diet. Table 1 lists the five most important mycotoxins from an agricultural prospective and provides information about their sources and health effects in animals and humans. Material exposure to these five toxins from indoor sources under normal circumstances is either impossible (deoxynivalenol, fumonisins, aflatoxins, zearlalenone) or exceptional (ochratoxin A).
In order to gain a perspective of the difficulties in making risk assessments for exposure to indoor molds, it is useful to examine the agriculturally important toxins for the lessons learned, with a view to framing research questions for exposures to toxins from building-associated fungi. From the outset, the complexity of the relationship between mycotoxin exposure and health outcome needs be understood. The health effects noted in Table 1 are the result of high exposure to the toxins involved (above the effect level). This is important because, even for aflatoxin, there is a no effect level for carcinogenicity. The p450 enzyme that converts aflatoxin B1 to the exo-8,9 expoxide (the proximate carcinogen) in vivo has a lower affinity for aflatoxin B1 than does the enzyme that converts aflatoxin B1 to the less dangerous endo-8,9 expoxide. The latter is then converted to a considerably less toxic forms and excreted (Guengerich et al. 1998). Thus, serum concentrations inadequate for the formation of the exo-8,9 expoxide are not associated with cancer. In addition, there are other complicating factors:
-
For at least one toxin (fumonisin B1) there is a variation in the acute and chronic health effects with different animal species (Table 1).
-
Laboratory studies using experimental animals (particular strains of mice, rats) or domestic species (pigs, chickens, horses, cows) involve studies with multiple doses of a single pure mycotoxin, usually after studies with naturally contaminated feed. Especially in developing countries, people can be exposed to more than one of the important toxins for a lifetime.
-
Poor nutrition is a major determinant in the population health effects of mycotoxins. In addition, there are other important factors that can increase or decrease the relative risk of mycotoxin-induced injury, including infections, age, sex and racial differences.
-
Epidemiological studies are an attempt to explore possible candidate agents for a particular disease endpoint. Their potential is greatest when there is a clear exposure measure. For example, determining that aflatoxin B1 was the most potent human chemical carcinogen known was not possible until some 20 years after the first such studies were reported and large epidemiology studies were done, using serum protein aflatoxin adducts as the exposure measure.
-
For aflatoxin B1 there is an array of excellent biomarkers of exposure in the strict sense (i.e., systemic exposure) and direct effect (see the following sections), for ochratoxin there is a good exposure measure (JECFA 2002), for deoxynivalenol there is an expensive measure of short-term exposure (Meky et al. 2002), for fumonisin B1 there is a weak indirect measure of exposure (JECFA 2002), and for zearalenone there is nothing. For the toxins for which there are biomarkers, this research cost many tens of millions of dollars. For the toxins from building-associated fungi there is nothing.
Inhalation exposure to fungi outside occupational circumstances involves two broad categories of fungi: fungi common in outdoor air and building-associated fungi that occur on damp or wet building materials. Except during snow cover and in deserts, there is always a high concentration of fungal elements (whole spores, spore and hyphal fragments) in outdoor air. The majority of fungi in outdoor air comprise two species of one genus, Cladosporium, along with other phylloplane species, mushroom spores, and various plant disease pathogens. Soil fungi such as Aspergillus and Penicillium are much less common in outdoor air in temperate climates. These are detected as a result of wind-blown soil particles and during the autumn season after leaf-fall (10-year integrated data are given by Nolard 1997). As a generalization, the species of genera that occur in outdoor air are not associated with human or animal toxicoses. Inhalation exposure to the fungi in outdoor air results in a moderate burden of allergic respiratory disease, especially hay fever symptoms (Horner et al. 1995).
Building-associated fungi comprise a narrow group of species that grow on the nutrients present in building materials and contents and occur in clusters of species that are adapted to particular amounts of available water. Many of these species are associated with uncommon agricultural toxicoses (Flannigan and Miller 2001). These include species such as Stachybotrys chartarum sensu lato (Miller et al. 2003), P. aurantiogriseum sensu lato and related species (Frisvad and Samson 1991; Miller 1995), and A. versicolor that is often encountered in damp buildings (Flannigan and Miller 2001). Strains of A. versicolor from building materials typically produce sterigmatocystin, a class 2B carcinogen (IARC 1993) and the penultimate precursor of the aflatoxins in aflatoxin-producing fungi (Yabe and Nakajima 2004). Sterigmatocystin has not been clearly related to animal disease, although it does occur in grain samples (Wilson et al. 2002). A. versicolor produces sterigmatocystin in both the built environment and when grown on building materials in the laboratory, although production is seen only under conditions of high water activity (aw>0.9; Engelhart et al. 2002; Nielsen 2002, 2003).
Although other species of the fungi listed in Table 2 are known to produce toxic compounds, few of their metabolites have been shown to be produced in natural indoor environments. On building materials in laboratory experiments, many of these fungi produce these compounds, but often in very limited amounts (Nielsen 2003; Nielsen et al. 2004).
Recent evaluations of the associations of fungi in damp homes indicate that building-associated molds are associated with the exacerbation of asthma in mold-sensitive asthmatics and increases in upper respiratory disease (National Academy of Sciences 2004; Health Canada 2004). Large-scale surveys of homes in North America have shown that 10–30% of these homes have sufficient mold damage to permit the detection of an increased relative risk of respiratory disease outcomes (e.g., Brunekreef et al. 1989; Dales et al. 1991; Spengler et al. 1994), with the true number probably closer to the lower figure.
The current concern with “toxic” molds was precipitated in the mid-1990s by the report of an unusual cluster of bleeding in the lungs of infants (idiopathic pulmonary hemosiderosis, IPH) in Cleveland, Ohio (Dearborn et al. 1999). The infants’ home environment was damp with significant mold growth; and one fungus in particular (S. chartarum) was cited as being strongly associated with IPH (Montana et al. 1997). Many in the public have come to view this fungus as a serious health risk to those exposed. Reviews by the National Academy of Sciences (2004) and Health Canada (2004) indicated it was not possible to exclude the hypothesis that very high exposures to S. chartarum sensu lato resulted in this disease. At the outset, it should be recognized that this species is not commonly associated with mold damage in homes in the United States and Canada (Flannigan and Miller 2001, Sheldon et al. 2002). The other point to emphasize is the degree of exposure. A postage stamp-sized growth of S. chartarum poses no material hazard, but a wall covered with this mold may well be another matter altogether (Miller et al. 2003).
As noted above, from an agricultural perspective, S. chartarum is a minor toxigenic fungus. The majority of reported mycotoxicoses associated with this fungus are in livestock (principally horses that have eaten moldy hay) from Central and Eastern Europe (Forgacs 1972). Interestingly, the first putative case of stachybotryotoxicosis in North America was reported by Croft et al. (1986) and did not involve farm animals but rather residents of a home in Chicago. This home had suffered extensive (and unattended) water damage that resulted in a heavy growth of S. chartarum, particularly in the air ducts. Some of the health symptoms of the residents were consistent with those seen from occupational exposures to S. chartarum.
Potent mycotoxic macrocyclic trichothecenes (e.g., satratoxin H, verrucarin J; see Fig. 2) were found in substantial quantity in the building material from the home (Croft et al. 1986). Similar health symptoms were experienced by workers clearing a heavily Stachybotrys-contaminated sub-basement in a New York library (Johanning 1995).
S. chartarum produces a variety of mycotoxins, the most potent of which are the macrocyclic trichothecenes, such as satratoxin H (see Fig. 2). However, only about 40% of S. chartarum isolates produce macrocyclic trichothecenes (Andersen et al. 2003) and these isolates are considerably more cytotoxic than are those isolates that do not produce these mycotoxins (Jarvis et al. 1998). The remaining 60% of the S. chartarum isolates produce atranones and two simple (but considerably less toxic) trichothecenes (trichodermol, trichodermin). However, all S. chartarum isolates produce the immunosuppressant spirocyclic drimanes (Fig. 2; Jarvis et al. 1998; Andersen et al. 2002). Both the chemistry (Jarvis 2003) and toxicology (Miller et al. 2003) of S. chartarum have been reviewed recently.
Biomarkers of exposure to building-associated fungi
Fungal spores contain beta 1,3-d glucan and antigenic proteins and can contain toxins that represent candidates for assessing exposure. Two of these classes of compounds are toxic rather than resulting in the production of antibodies. There is little known about the antigens from building-associated fungi, compared with those from the fungi common in outdoor air (Miller and Day 1997; Miller et al. 2003). The presence of antibodies in human sera to fungal antigens indicates exposure at some time in the past. The response lasts for a variable period but, if positive for particular toxin-producing fungi, it might serve as a proxy for toxin exposure.
Inhalation exposure to fungal glucan results in a number of effects, including changes in neutrophils, macrophages, complement, and eosinophils and changes in the blood levels of inflammatory markers in both humans and animals (Rylander and Lin 2000; Thorn et al. 2001). A human macrophage beta-glucan receptor has been identified that binds to T-lymphocytes (Willment et al. 2001). It is possible that methods could be devised to detect changes in the activation of the glucan receptor indicative of exposure to this toxin.
Measures to assess toxin exposure come in two categories: direct and indirect. Direct measures include the presence of serum adducts. These are available for both ochratoxin A and aflatoxin B1. There are several methods now available for assessing exposure to aflatoxin B1. The measurement of the metabolic product, aflatoxin M1, and another metabolite on the detoxification pathway, aflatoxin B1-mercapturic acid, in urine are indicators of recent exposure. The measurement of aflatoxin B1 albumin adducts in serum is a measure of chronic exposure. The excretion of aflatoxin B1-N7-guanine in urine is an indicator of actual genetic damage resulting from aflatoxin B1 exposure. Finally, in liver tumor cells, the measurement of transverse mutations at codon 249 of the p53 gene on (human) chromosome 17 is direct evidence that aflatoxin caused the tumor (IARC 2002). This illustrates the range of measures that are possible for the direct assessment of fungal toxin exposure, but also the cost and difficulty in obtaining such measures.
It is also possible, although much less useful, to use indirect measures of toxin exposure. The best example of this is the toxin fumonisin B1. Fumonisin exposure in animals results in disruption of sphingolipid biosynthesis. The most easily measured change that can be measured in tissues is a change in the ratio of sphinganine to sphingasine. This happens in animals when there is an adequate threshold dose (IARC 2002). This method is not particularly sensitive to small changes and has not yet been reliably demonstrated in humans.
Conclusions
There is consensus that inhalation exposure to molds can result in human health problems, but that there are a number of factors, most of which cannot be quantified, that affect the outcome of these exposures. There are good epidemiological data available that show that atopic people (those genetically predisposed to allergies and asthma) are sensitive to mold spores and that molds contribute to upper respiratory health problems in children. Case studies suggest that those exposed to what appear to be high levels of indoor molds experience health problems, but without any direct measure of exposure to mold (and mold metabolites) for those individuals through biomarkers, it is very difficult to assess the role played by exposures to molds by those individuals.
It is likely that the toxins, including both glucan and low molecular weight compounds from building-associated fungi, play some role in the pattern of disease from building exposures. The earliest epidemiology data for the increases in upper respiratory disease observed in many studies indicated that this effect occurs equally in atopic and non-atopic individuals. This would not be expected if allergy alone explained the pattern of disease observed. The contribution that low molecular weight toxins play is likely to be indirect, as a consequence of effects on various lung cells (Miller et al. 2003). The studies needed to illuminate this question will require a better understanding of the identities and amounts of toxin metabolites that occur in housing and improved assays of their impact on lung biology.
References
Andersen B, Nielsen KF, Jarvis BB (2002) Characterisation of morphologically, chemically and physiologically different Stachybotrys species from water-damaged buildings. Mycologia 94:392–403
Andersen B, Nielsen KF, Thrane U, Cruse M, Taylor J, Jarvis BB (2003) Stachybotrys chlorohalonata, a new species from water-damaged buildings. Mycologia 95:1228–1237
Beardall JM, Miller JD (1989) Disease in humans with mycotoxins as possible causes. In: Miller JD, Trenholm HL (eds) Mycotoxin in grains. Compounds other than aflatoxins. Eagan, St Paul, pp 487–539
Bennett JW, Klich M (2003) Mycotoxins. Clin Microbiol Rev 16:497–516
Brunekreef B, Dockery DW, Speizer FE, Ware JH, Spengler JD, Ferris BH (1989) Home dampness and respiratory morbidity in children. Am Rev Respir Dis 140:1363–1367
Bucci T, Hansen DK, LaBorde JB (1996) Leucoencephalomalacia and hemorrhage in the brain of rabbits gavaged with mycotoxin fumonosin B1. Nat Toxins 4:51–52
Cole RJ, Cox RH (1981) Handbook of toxic fungal metabolites. Academic, New York
Cole RJ, Schweikert MA, Jarvis BB (2003) Handbook of secondary fungal metabolites (3 vols). Academic, New York
Croft WA, Jarvis BB, Yatawara CS (1986) Airborne outbreak of trichothecene toxicosis. Atmos Environ 20:449–552
Dales RE, Zwanenburg H, Burnett R, Franklin CA (1991) Respiratory health effects of home dampness and molds among children. Am J Epidemiol 134:196–293
Dearborn DG, Yike I, Sorenson WG, Miller MJ, Etzel RA (1999) Overview of investigation into pulmonary hemorrhage among infants in Cleveland, Ohio. Environ Health Perspect 107[Suppl 3]:495–499
Engelhart S, Loock A, Skutlarek D, Sagunski H, Lommel A, Farber H, Exner M (2002) Occurrence of toxigenic Aspergillus versicolor isolates and sterigmatocystin in carpet dust from damp indoor environments. Appl Environ Microbiol 68:3886–3890
Flannigan B, Miller JD (2001) Microorganisms on building materials. In: Flannigan B, Samson R, Miller JD (eds) Microorganisms and indoor work environments. Taylor & Francis, London, pp 35–68
Forgacs J (1972) Stachybotryotoxicosis. In: Kadis S, Ceigler A, Ajl SJ (eds) Microbial toxins, vol 8. Academic, New York, pp 95–128
Frisvad, JC, Samson, RA (1991) Mycotoxins produced by species of Penicillium and Aspergillus occurring in cereals. Dev Food Sci 26:441–476
Gelderblom WCA, Jaskiewicz K, Marasas WFO, Thiel PG (1991) Toxicity and carcinogenicity of the Fusarium moniliforme metabolite, fumonosin B1 in rats. Carcinogenesis 12:1247–1251
Guengerich FP, Johnson WW, Shimida T, Ueng YF, Yamazaki H, Langouet S (1998) Activation and detoxification of aflatoxin B1. Mutat Res 42:121–128
Harrison LR, Colvin BM, Greene JT, Newman LE, Cole JR Jr (1990) Pulmonary edema and hydrothorax in swine produced byfumonison B1 a toxic metabolite of Fusarium moniliforme. J Vet Diagn Invest 2:217–221
Health Canada (2004) Fungal contamination in public buildings: health effects and investigation methods. Health Canada, Ottawa
Horner WE, Helbling A, Salvaggio JE, Lehrer SH (1995) Fungal allergens. Clin Microbiol Rev 8:161–179
IARC (1993) Some naturally occurring substances: food items and constituents, heterocyclic amines, and mycotoxins. IARC Monogr 56:489–520
IARC (2002) Traditional herbal meds, mycotoxins, naphthalene, and styrene. (IARC Monogr 82) International Agency for Research on Cancer, Paris
Jarvis BB (2003) Stachybotrys chartarum: a fungus for our time. Phytochemistry 64:53–60
Jarvis BB, Sorenson WG, Hintikka E-L, Nikulin M, Zhou Y, Jiang J, Wang S, Hinkley S, Etzel RA, Dearborn D (1998) Study of toxin production by isolates of Stachybotrys chartarum and Memnoniella echinata isolated during a study of pulmonary hemosiderosis in infants. Appl Environ Microbiol 64:3620–3625
JECFA (2002) Evaluation of certain mycotoxins in food. (Joint FAO/WHO expert committee on food additives report 56) WHO Tech Rep 906
Johanning E (1995) Health problems related to fungal exposue—the example of toxigenic Stachybotrys chartarum (atra). In: Johanning E, Yang CS (eds) Fungi and bacteria in indoor air environments. Eastern New York Occupational Health Program, Latham, pp 169–182
Kuiper-Goodman T, Scott PM (1989) Risk assessment of the mycotoxin ochratoxin A. Biomed Environ Sci 2:179–228
Kurtz HJ, Mirocha J (1978) Zearalenone (F2)induced estrogenic syndrome in swine. In: Wyllie TD, Morehouse LG (eds) Mycotoxic fungi, mycotoxins, mycotoxicoses, vol 2. Dekker, New York, pp 1256–1264
Marasas WFO, Kellerman TS, Gelderblom WCA, Coetzer JAW, Thiel PG, Van Der Lugt JJ (1988) Leucoencephalomalacia in hose induced by fumonosin B1 isolated from Fusarium moniliforme. Onderstepoort J Vet Res 55:197–203
Meky FA, Turner PC, Ashcroft AE, Miller JD, Qiao YL, Roth ML, Wild CP (2002) Development of a urinary biomarker of human exposure to deoxynivalenol. Food Chem Toxicol 41:265–273
Miller JD (1995) Fungi and mycotoxins in grain: implications for stored product research. J Stored Prod Res 31:1–6
Miller JD (1999) Mycotoxins. In: Francis FJ (ed) Encyclopedia of food science and technology. Wiley, New York, pp 1698–1706
Miller JD, Day JD (1997) Indoor mold exposure: epidemiology, consequences and immunothapy. Can J Allergy Clin Immunol 2:25–32
Miller JD, Jarvis BB, Rand TG (2003) Stachybotrys chartarum: cause of human disease or media darling? Med Mycol 41:271–291
Montana E, Etzel R, Allan T, Horgan T, Dearborn D (1997) Environmental risk factors associated with pediatric idiopathic pulmonary hemorrhage and hemosiderosis in a Cleveland community. Pediatrics 99:e5, http://pediatrics.aapublications.org/cgi/content/full/99/1/e5
National Academy of Sciences (2004) Damp indoor spaces and health. National Academies, Washington, D.C., http://www.nap.edu
Nielsen KF (2002) Mold growth on building materials. Secondary metabolites, mycotoxins and biomarkers. PhD thesis, Technical University of Denmark, BioCentrum-DTU, http://www.biocentrum.dtu.dk/mycology/publications/phd-kfn.pdf
Nielsen KF (2003) Mycotoxin production by indoor molds. Fungal Genet Biol 39:103–198
Nielsen KF, Holm G, Uttrup LP, Nielsen PA (2004) Mould growth on building materials under low water activities. Influence of humidity and temperature on fungal growth and secondary metabolism. Internat Biodeter Biodegrad (in press)
Nolard N (1997) Moulds and respiratory allergies. Expressions 5:7–9
Ross RK, Yuan JM, Yu MC, Wogan GN, Qian GS, Tu JT, Groopman J, Gao YT, Henderson BE (1992) Urinary aflatoxin biomarkers and risk of heptocellular carcinoma. Lancet 339:1413–1414
Rotter BA, Prelusky DB, Pestka JJ (1996) J Toxicol Environ Health 48:1–34
Rylander R, Lin RH (2000) (1-3)-β-d-Glucan—relationship to indoor air-related symptoms, allergy and asthma. Toxicology 152:47–52
Samson RA (1999) Ecology, detection and identification problems of moulds in indoor environments. In: Johanning E, Yang CS (eds) Bioaerosols, fungi, and mycotoxins: health effects, assessment, prevention, and control. Boyd, Albany, pp 33–37
Sheldon BG, Kirkland KH, Flanders WD, Morris GK (2002) Profiles of airborne fungi in buildings and outdoor environments in the United States. Appl Environ Microbiol 68:1743–1753
Spengler JD, Neas L, Nakai S, Dockery D, Speizer F, Ware J, Raizenne M (1994) Respiratory symptoms and housing characteristics. Indoor Air 4:72–82
Sydenham EW, Shephard GS, Thiel PG, Marasas, WFO, Stockenstrom S (1991) Fumonision contamination of commercial corn-based human foodstuffs. J Agric Food Chem 39:2014–2018
Thorn J, Beijer L, Rylander R (2001) Effects after inhalation of (1-3)-β-d-glucan in healthy humans. Mediators Inflamm 10:173–178
Turner PC, Nikiema P, Wild CP (1999) Fumonisin contamination of food: progress in development of biomarkers to better assess human health risks. Mutat Res 443:81–93
Willment JA, Gordon S, Brown GD (2001) Characterization of the human beta-glucan receptor and its alternatively spliced isoforms. J Biol Chem 276:43818–43823
Wilson DM, Mubatanhema W, Jurjevic Z (2002) Biology and ecology of mycotoxigenic Aspergillus species as related to economic and health concerns. Adv Exp Med Biol 504:3–17
Yabe K, Nakajima H (2004) Enzyme reactions and genes in aflatoxin biosynthesis. Appl Microbiol Biotechol 64:745–755
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jarvis, B.B., Miller, J.D. Mycotoxins as harmful indoor air contaminants. Appl Microbiol Biotechnol 66, 367–372 (2005). https://doi.org/10.1007/s00253-004-1753-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-004-1753-9