Abstract
Complement is one of primary defense mechanisms against intravascular microorganisms and could play a role in the immune response to malignancy and hence its clinical behavior. We evaluated if the sole coding polymorphism of C1qA associates with outcome in patients with breast carcinoma. Genotyping for C1qA[276A/G] was performed in 63 breast cancer subjects with localized tumor and compared with that in 38 breast cancer subjects with metastasis. Established risk factors for clinical outcome were considered and evaluated in multivariable analysis. Breast cancer subjects with heterozygous or homozygous C1qA[276G] genotype had a higher rate of metastasis than subjects with the homozygous C1qA[276A] genotype [hazard ratio (HR) 2.4, 95% confidence interval (CI) 1.1–4.1]. This association was stronger when only metastatic sites associated with hematogenous spread, i.e., to the bone, liver, and brain, were considered (HR 3.5, 95% CI 1.4–5.6) and remained statistically significant after adjustment for the number of positive lymph nodes, estrogen receptor status, and progesterone receptor status. There was no statistical difference in the C1qA[276A/G] allelic distribution between all subjects with breast cancer and controls. These results suggest there could be an association of a single nucleotide polymorphism at position 276 of the C1qA component of complement with breast cancer metastasis to sites linked to hematogenous spread of disease. The C1qA polymorphism associated with decreased distant metastasis has also been correlated with an increased incidence of subcutaneous systemic lupus and C1q deficiencies, suggesting that an altered immune response may play a role in the observed association.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antitumor antibodies can impede tumor growth and spreading by inducing complement-mediated lysis (Gelderman et al. 2004; Hakulinen and Meri 1998; Harjunpaa et al. 2000), mediating antibody-dependent cellular cytotoxicity (Eccles 2001), or directly triggering cell cycle arrest and apoptosis of tumor cells (Racila et al. 1995). The complement system is an essential component of the innate immune system (Walport 2001). In vitro and animal model studies suggest that complement factors and complement inhibitors can amend the immune response to tumors and could be important in determining the response to cancer immunotherapy (Caragine et al. 2002; Fishelson et al. 2003; Golay et al. 2000; Jurianz et al. 1999). Complement fractions may also play an indirect role in cell-mediated cytotoxicity by recruiting the effector cells at the site of inflammation, infection, or tumor development (Baldwin et al. 1999; Onoe et al. 2002; Tazawa et al. 2003).
Various neoplasms have been shown to induce production of autoantibodies (Abu-Shakra et al. 2001; Conrad 2000; Posner 2003; Tan 2001; Zeng et al. 2002), which in turn could activate complement. Although the immune response to tumor antigens is rarely accompanied by primary tumor growth eradication (Jager et al. 2001), it has been suggested that patients that are able to build antitumor immunity have a significantly better overall prognosis (Hansen et al. 2001; Pardoll 1999). Whether complement activation plays a role in the potential association between humoral antitumor immunity and prognosis is not known.
C1q, the first subcomponent of the C1 complex, recognizes immune complexes and initiates the classical pathway of complement activation (Reid 1983). Human C1q is a large (460 kDa) and complex molecule composed of six trimers of the chains C1qA, C1qB, and C1qC (Kishore and Reid 2000). The C1qA gene, located on chromosome 1, contains six single nucleotide variations that are currently catalogued in the NCBI database (Fig. 1). Two of these are located in the intron and three in the 3′ untranslated region of the gene. The only coding single nucleotide polymorphism (SNP) is C1qA[276A/G] (rs172378) and is located at the beginning of the second exon. We previously reported that homozygous C1qA[276A] SNP associates with subcutaneous lupus erythematosus in a limited number of patients (Racila et al. 2003).
Recently, an absolute correlation between complete serum C1q deficit and homozygous C1qA[276A] genotype in patients from seven families with different forms of C1q deficiencies has been reported (Petry and Loos 2005). The finding that a deficiency in complement is associated with enhanced autoimmunity would seem to be counterintuitive. One possible explanation is that complement deficiency results in impaired clearance of apoptotic cells or cellular debris, and this leads to an enhanced autoimmune response. Indeed, C1q has been shown to play a critical role in the clearance of apoptotic bodies and limitation of autoimmunity (Korb and Ahearn 1997). Based on these observations, it is conceivable that a weaker complement system might be less effective against circulating microorganisms but, at the same time, lead to a more rigorous cellular immune response. Thus, paradoxically, decreased complement activity could lead to enhanced cellular immunity to intracellular organisms or malignancy.
Hundreds of SNPs suspected to either predispose to cancer or alter clinical outcome have been studied (Erichsen and Chanock 2004; Zhu et al. 2004). Given that complement may play a role in clearing tumor cells, either alive or dead, and polymorphisms in C1qA may change the functionality of the complement system, we evaluated whether polymorphism in the C1qA[276] locus correlate with the development of sites of metastasis in breast cancer associated with hematogenous spreading of disease.
Materials and methods
Breast cancer subjects and sample collection
Subjects were enrolled over a period of 4 months through the Holden Comprehensive Cancer Center, University of Iowa Hospitals and Clinics. Ninety-five percent of the interviewed subjects agreed to participate into this study. Blood samples were collected from 101 subjects with breast carcinoma after proper consent was obtained. The racial composition of the patient population was 93% Caucasian, 5% African-American, and 2% Asian and Hispanic. No subjects were related, and there was no preselection based on time since diagnosis or other factors. Patient records were screened for relevant information regarding age, age at primary diagnosis of breast cancer, pathology and grade, detectable lymphatic, vascular and perineural invasion within the tissue specimens, sentinel and axillary lymph nodes involvement, expression of estrogen and progesterone receptors, HER-2 positivity, and stage based on standard clinical and diagnostic imaging data including MRI, CT scan, and PET analysis when available. Time between diagnosis and identification of metastases or last follow-up was recorded. The majority of cases were ductal carcinoma of either infiltrating (64%) or invasive type (23%). The remainders were lobular carcinoma (8%), ductal carcinoma in situ (4%), and tubular carcinoma (1%). Genomic DNA was extracted from peripheral leukocytes of each subject by means of phenol–chloroform followed by precipitation with ethanol or fiberglass column techniques.
PCR and restriction fragment-length polymorphism analysis
For the PCR amplification of the whole C1qA gene, the following primers were used: forward 5′TGAGTGTGTGAAGATGTGGG and reverse 5′AGGGTAGTGGTTAAACACAGG. A first denaturation step at 94°C for 3 min was followed by 35 cycles of denaturation at 94°C 20 s, annealing at 58°C for 30 s, extension at 68°C for 3 min, and a 10-min final extension step. To ensure accuracy of sequencing data, Platinum Taq High-Fidelity (Invitrogen) was the enzyme of choice. The PCR product was extracted from 1% agarose gels using fiberglass columns and used for direct sequencing. For restriction fragment-length polymorphism (RFLP) analysis, the target template containing the C1qA[276A/G] polymorphism was amplified using forward 5′TAAAGGAGACCAGGGGGAAC and reverse 5′TTGAGGAGGAGACGATGGAC primers with an extension step reduced to 45 s. Prior to restriction digest, the amplicons were purified by extraction with phenol–chloroform and precipitation with ethanol.
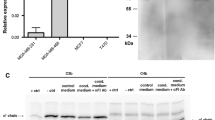
Enzymatic digestion with ApaI restriction endonuclease (New England Biolabs, Beverly, MA, USA) was used to analyze the C1qA[276] polymorphism. Enzymatic digestion with ApaI of the 338-bp PCR product containing the C1qA[276G] allelic sequence results in four fragments of variable length from 7 to 269 bp. The largest of these fragments can be visualized on agarose gels. C1qA[276A] allele lacks the third ApaI restriction site (GGGCC/C) at the codons for Gly92 (GGG) and Ala93 (GCC) and, thus, yields a heavier fragment of 288 bp after ApaI digestion. Separation of restriction digest fragments was done in 2.5% agarose gels (Fig. 2). The first set of 37 specimens was also analyzed for the C1qA polymorphism by sequencing to ensure accuracy between the two methods. DNA sequencing was done using the dye terminator cycle sequencing method with AmpliTaq DNA polymerase and FS enzyme (PE Applied Biosystems, Foster City, CA, USA) and forward 5′GAGTCTCATGGAATCAC sequencing primer. The reactions were run and analyzed with Applied Biosystems Model 373A stretch fluorescent automated sequencer at the University of Iowa DNA Core Laboratory Facility.
RFLP analysis of C1qA[276A/G] polymorphism. The results obtained after digestion of C1qA amplicons from three heterozygous C1qA[276A/G] breast cancer patients (lanes 2, 3, and 5), two homozygous C1qA[276A] patients (lanes 1 and 7), and two homozygous C1qA[276G] breast cancer patients (lanes 4 and 6) are shown. Restriction digest with ApaI endonuclease of the amplicon containing the C1qA[276G] polymorphism yields a fragment 19 bp shorter than the uncut C1qA[276A] product of 288 bp. Digested fragments are separated in a 2.5% agarose gel
Statistical analysis
In addition to C1qA[276A/G] allelic distribution, established risk factors for clinical outcome in breast cancer like age at diagnosis, histology grading, pathology findings regarding lymphatic, vascular, and perineural invasion, tumor involvement of sentinel and axillary lymphatic nodes, and distant organs involved in the metastatic process were considered and evaluated. The Pearson's χ 2 or Fisher's exact tests were used to analyze group differences for categorical variables between the genotypes. Logistic regression was used to estimate the odds ratio (OR) of disease associated with C1qA[276A/G] SNP variation (AG/GG vs AA).
This study was designed as a retrospective cohort study. All breast cancer subjects were enrolled in succession after the informed consent was obtained for the use of genomic samples and the analysis of clinical data in accordance to a protocol approved by the institutional review board of our institution. There was no selection of subjects based on the spread of the disease. The time of entry considered in the statistical analysis was the date of primary diagnosis. Time to metastasis was measured in days from initial diagnosis until diagnosis of metastasis or most recent follow-up in subjects without documented metastasis. Among subjects without metastasis, the median follow-up time was 14 months, ranging from 1 to 234 months. Time to metastasis curves were estimated by the Kaplan–Meier method (Kaplan and Meier 1958). Cox regression was used to estimate the hazard ratio (HR) of metastasis associated with C1qA[276A/G] SNP variation (AG/GG vs AA) and other risk factors (Cox 1972). P values from Cox regression were based on the likelihood ratio test. Ninety-five percent confidence intervals for the ORs and HRs were based on the normal approximation. Due to unavailable data for some patients on the established risk factors of breast cancer, multivariate analyses examining the association between C1qA[276A/G] SNP and time to distant metastases were limited to adjustment for one of the following factors at a time to preserve the sample size: number of positive lymph nodes, positive phenotype for estrogen receptors, or positive phenotype for progesterone receptors. All statistical analyses were performed using SAS version 8.2 (SAS Institute, Cary, NC, 2001). The Kaplan–Meier curves were generated using the GraphPad Prism version 4 software (GraphPad Software Inc., San Diego CA, 2003).
Results
The demographics and general characteristics of subjects enrolled in this study are outlined in Table 1. The average age of the participants at time of primary diagnosis of breast carcinoma was 52 years old, ranging from 31 to 80 years old. Most subjects (54%) were in the group of age 41–55 years old. Fifteen percent of subjects were younger than 40 years old, and 6% of subjects were over 70 years old. The vast majority of primary lesions were ductal carcinoma of infiltrating/invasive type (87%), out of whom 36% developed metastatic disease. In four out of eight subjects with invasive lobular carcinoma, the disease eventually progressed to distant metastasis, while one out of four subjects with ductal carcinoma in situ developed metastasis. As expected, there was a correlation between the Elston–Ellis histological grading of the primary tumor and development of metastatic disease with 17% of the subjects with grade 1, 29% of the subjects with grade 2, and 52% of the subjects with grade 3, eventually developing metastases. Of the microscopic features of the primary tumor, lymphatic and vascular invasions were most predictive of metastasis with 54% of the subjects with lymphatic invasion and 46% of the subjects with vascular invasion developing metastases, as opposed to 21% of cases with no invasion or invasion limited to perineural spaces. Positive phenotype for estrogen and progesterone receptors was found in 77 and 71% of the subjects, respectively, while expression of c-erb/HER2 was found in 39% of the subjects. Negative phenotype for estrogen receptor was accompanied by a 2.8 times increased risk to develop metastatic disease compared to estrogen receptor positive subjects (95% CI interval 1.29–5.88, P=0.009), while subjects with lack of expression of progesterone receptors had a 3.1 times increased hazard to develop metastasis over those with a positive phenotype for progesterone receptor (95% CI interval 1.41–6.66, P=0.005). As expected, there was a good correlation between the extent of regional lymphatic invasion and progression to metastatic disease. Only 19% of subjects with no positive lymphatic nodes developed metastasis. This percentage more than doubled (45%) in subjects with less than five positive nodes and increased even further to 73% in subjects with five or more positive axillary nodes. Subjects with five or more positive lymph nodes for tumor had a 3.5 times higher risk to develop metastasis than subjects with four positive lymph nodes or less (95% CI interval 1.41–8.56, P=0.007). In the limited number of subjects who had undergone sentinel node biopsy (22 out of 101), two out of six subjects with positive sentinel nodes developed metastasis, while one of the remaining subjects with negative sentinel nodes showed clinical signs of tumor spread at the time of last follow-up. Overall, the demographics in this population of breast cancer subjects demonstrate the expected concordance between known prognostic factors and development of metastatic disease.
The NCBI SNP database contains the C1qA[276A/G] (rs172378) genotype of 100 individuals with similar racial composition to the breast cancer population enrolled in this study. In addition, we evaluated 17 female healthy donors and found that they had a similar C1qA[276A/G] allelic distribution to the NCBI SNP database. The frequency of the C1qA[276A] allele among breast cancer subjects was 0.63, while the frequency of the C1qA[276G] allele was 0.37. The analysis of breast cancer subjects as a whole demonstrated that the C1qA[276A/G] allelic distribution is not statistically different from the control NCBI group (χ 2 test, P=0.69). In contrast, comparison of the patients with distant metastasis and controls showed an elevated OR of 2.1 (P=0.11) for AG/GG vs AA genotype. The OR dropped to 0.51 (P=0.05) when the frequencies of the C1qA[276] AG/GG vs AA genotypes were compared between the breast cancer population without metastatic disease and controls.
The frequency of the homozygous C1qA[276A] genotype was significantly lower in subjects with distant metastatic disease compared to heterozygous and homozygous C1qA[276G] genotypes. Thus, breast cancer subjects with heterozygous or homozygous C1qA[276G] genotypes had an increased HR of 2.4 (P=0.03) over those with homozygous C1qA[276A] genotype to develop metastasis (Table 2). The analysis of the patients with distant metastases revealed an association of the C1qA[276G] allele and metastatic disease likely due to hematogenous spread, i.e., metastases to the brain, liver, or bone (Fig. 3). The hazard for developing bone metastasis in heterozygous and homozygous C1qA[276G] breast cancer patients was 3.5 times that for patients carrying the homozygous C1qA[276A] genotype (P=0.005). The hazard for developing either brain, liver, or bone metastasis was estimated to be 3.5 times higher in heterozygous C1qA[276A][276G] or homozygous C1qA[276G] patients compared to homozygous C1qA[276A] patients (P=0.005). The presence of the C1qA[276G] allele was also associated with an increased risk for liver or brain metastasis (HR 6.1, P=0.006). No statistically significant association was found between genotypes and the dissemination to the lymphatics, mediastinum, or lungs without other metastatic disease (Table 2).
Time to metastasis by C1qA[276] genotype based on the Kaplan–Meier method. The product limit method of Kaplan and Meier was used to create time to metastasis curves for all metastases (a) or restricted to bone, brain, or liver metastases (b). The dashed line is for the homozygous C1qA[276A] genotype (N=41), while the solid line depicts the collapsed heterozygous and homozygous C1qA[276G] genotypes (N=60). Vertical tick marks on curves indicate censored observations
Multivariate analyses for time to breast cancer metastasis or time to metastasis limited to the bone, brain, or liver were adjusted for regional lymphatic spread to axillary nodes, positive phenotype for estrogen receptors, or positive phenotype for progesterone receptors (Table 3). After adjustment for positive lymph nodes, the hazard for heterozygous and homozygous C1qA[276G] genotypes was 2.8 times higher than that for the homozygous C1qA[276A] genotype to develop metastasis and 5.8 times higher than that for the homozygous C1qA[276A] genotype in subjects with metastasis limited to the bone, brain, or liver. The estimated HRs were slightly lower after adjustment for positive estrogen receptor phenotype but still elevated, with the heterozygous and homozygous C1qA[276G] subjects having a 2.2 times higher risk to develop metastasis and a 3.4 times increased risk to develop metastases in the bone, brain, or liver compared to subjects with homozygous C1qA[276A] genotype. It is important to note that the vast majority of the patients with a positive phenotype for estrogen receptors were treated with tamoxifen, a specific receptor blocker that considerably improves the clinical outcome but may obscure an association due to a significant delay in onset or prevention of metastasis. Adjustment for progesterone receptor phenotype yielded similar results, with the heterozygous and homozygous C1qA[276G] subjects having a 2.6 higher risk to develop breast cancer metastasis and a four times increased hazard for progression to metastasis involving the bone, brain, or liver than subjects with homozygous C1qA[276A] genotype (Table 3).
Discussion
Significant similarities between autoantibodies in autoimmune diseases and autoantibodies in cancer have been observed (Tan and Shi 2003). Patients with some autoimmune diseases have an increased propensity to develop various types of cancer (Kauppi et al. 1997; Mellemkjaer et al. 1997; Peters-Golden et al. 1985; Sigurgeirsson et al. 1992). A significant association between systemic lupus erythematosus and breast carcinoma has been reported (Ramsey-Goldman et al. 1998). While these data suggest that a relationship may exist between autoimmunity and development of cancer, it remains unclear whether development of an autoimmune response can be induced by cancer, protects against cancer, predisposes to cancer, or influences in other ways the interaction between the host and the cancer. It is possible that although an autoimmune disease may be a risk factor for a primary neoplastic process due to locoregional inflammation, it may paradoxically represent a favorable attribute for clinical outcome due to development of an immune response that could impact on the dissemination of tumor.
In fact, the data presented here provide the first evidence that a polymorphism in complement that may result in a less rigorous complement-mediated response is associated with both an increased chance of developing autoimmunity and an altered pattern of malignant spread. We previously reported that a polymorphism in the C1q component of complement is associated with subcutaneous lupus erythematosus (Racila et al. 2003). Patients with lupus had a higher than expected incidence of homozygous C1qA[276A] SNP. In the current studies, we report the first evidence that the C1qA[276A] genotype is also associated with a metastasis-free prognosis in breast cancer patients.
Little is known with regard to defense mechanisms guarding against hematogenous dissemination and the role of complement system in patients with cancer. It is known that most tumors constantly shed cells into circulation and that the vast majority of these cells soon undergo apoptosis. One possibility is that in breast cancer patients homozygous for C1qA[276A], the removal of the apoptotic tumor cells is impaired, leading to increased exposure of various components of the immune system to tumor antigens and, consequently, to a superior antitumor cellular response. Complement could have other effects on the pattern of breast cancer spread. Distant dissemination of tumor is the result of active molecular mechanisms developed by tumor cells that allow them to traverse endothelial barriers, enter blood or lymphatic vessels, invade into other tissues, and develop their own vascular supply (Balkwill 2004; Boedefeld et al. 2003; Pantel and Brakenhoff 2004; Roodman 2004). In this sequence of events, the circulating tumor cell in the blood, and to a limited extent in the lymphatic vessels, may be susceptible to the action of complement that is fixed on the tumor cells either directly or in the presence of antitumor antibodies. It is possible that heterogeneity in host complement activity might impact on the pattern of metastatic spread by either eliminating malignant cells from the circulation before they have the chance to invade other tissues or by altering the trafficking pattern of the cells, such as increasing their chances of being trapped in the lung on a first-pass effect.
The C1qA[276] G for A substitution is a synonymous SNP of the third base of the codon for Gly92 (Gly70 after removal of the lead peptide). While it was previously thought that such polymorphisms are “silent,” there is now clear evidence that synonymous SNPs can alter the expression or function of a protein. For example, synonymous SNPs within the DRD2 transcript reduce the stability of the mRNA and, consequently, the expression of the dopamine receptor (Duan et al. 2003). Another mechanism that would lead to functional effects from a synonymous SNP is biased codon usage (Carlini et al. 2001). SNPs located within introns, which were similarly considered to have no functional effect, were shown to participate in the activation of alternative splicing mechanisms leading to generation of mRNA isoforms or exon skipping (Emmert et al. 2001; Khan et al. 2002; Modrek et al. 2001; von Ahsen and Oellerich 2004; Webb et al. 2003). We are currently exploring the possibility that the C1qA[276] SNP impacts on proper recognition of the intron/exon boundary. Additional studies aimed at defining prevalent haplotypes along with the end result of in vitro transcription and splicing experiments will directly address this hypothesis.
The results outlined above represent the first evidence that a genetic polymorphism in complement may, in fact, impact on the pattern of metastatic disease in cancer. Thus, systemic metastasis from breast cancer, defined as disease that could only occur by hematogenous spread of malignant cells that had passed through the pulmonary circulation, was statistically less common in patients with the homozygous C1qA[276A] SNP than in patients that were heterozygous or homozygous for C1qA[276G]. This association remained significant after adjusting for number of positive lymph nodes, estrogen receptor status, or progesterone receptor status.
While we have demonstrated a correlation between clinical outcome and this C1qA SNP, we do not yet understand the molecular mechanisms responsible for this observation. Ongoing work is exploring the functional differences between C1qA[276A] and C1qA[276G]. We are also evaluating how complement impacts on activation of the cellular immune system. The interactions between complement and mechanisms involved in the invasive potential of malignant cells, such as expression of adhesion molecules by malignant cells, are complex, and the impact of the C1qA[276] SNP on these mechanisms needs to be studied further. With this in mind, we are currently evaluating whether the number of malignant cells found in the circulation of breast cancer patients correlates with the C1qA polymorphism. Additional progress along various lines of investigation, extending from exploring the impact of this polymorphism on basic complement function through analysis of how this polymorphism impacts on the behavior of malignant cells in vivo, to confirmation of the effect reported here, are all needed before we can understand fully the prognostic and therapeutic significance of the data presented above.
In summary, this study points to a possible association between a polymorphism in C1qA known to be associated with decreased complement activity, and reduced hematogenous spread of breast cancer. This raises the possibility that diminished complement activity results in less effective clearance of apoptotic tumor cells and, consequently, a more effective development of an antitumor immune response. Importantly, this study should be considered hypothesis generating and not hypothesis confirming. The number of subjects was relatively small, the duration of follow-up was limited, and data for the other prognostic factors were not available for all subjects. A larger, prospective study with longer follow-up is needed to verify these findings. If confirmed in these additional studies, the association of C1qA polymorphism and pattern of breast cancer metastasis could have major implications on our understanding of the process of metastasis and be of great prognostic and therapeutic use. For example, confirmation of this finding could impact on identification of patients who would benefit from adjuvant chemotherapy and provide impetus for developing approaches to therapy that enhance immune clearance of circulating malignant cells.
References
Abu-Shakra M, Buskila D, Ehrenfeld M, Conrad K, Shoenfeld Y (2001) Cancer and autoimmunity: autoimmune and rheumatic features in patients with malignancies. Ann Rheum Dis 60:433–441
Baldwin WM III, Qian Z, Wasowska B, Sanfilippo F (1999) Complement causes allograft injury by cell activation rather than lysis. Transplantation 67:1498–1499
Balkwill F (2004) Cancer and the chemokine network. Nat Rev Cancer 4:540–550
Boedefeld WM II, Bland KI, Heslin MJ (2003) Recent insights into angiogenesis, apoptosis, invasion, and metastasis in colorectal carcinoma. Ann Surg Oncol 10:839–851
Caragine TA, Okada N, Frey AB, Tomlinson S (2002) A tumor-expressed inhibitor of the early but not late complement lytic pathway enhances tumor growth in a rat model of human breast cancer. Cancer Res 62:1110–1115
Carlini DB, Chen Y, Stephan W (2001) The relationship between third-codon position nucleotide content, codon bias, mRNA secondary structure and gene expression in the drosophilid alcohol dehydrogenase genes Adh and Adhr. Genetics 159:623–633
Conrad K (2000) Autoantibodies in cancer patients and in persons with a higher risk of cancer development. Elsevier, Amsterdam
Cox DR (1972) Regression models and life tables (with discussion). J R Stat Soc B 34:187–220
Duan J, Wainwright MS, Comeron JM, Saitou N, Sanders AR, Gelernter J, Gejman PV (2003) Synonymous mutations in the human dopamine receptor D2 (DRD2) affect mRNA stability and synthesis of the receptor. Hum Mol Genet 12:205–216
Eccles SA (2001) Monoclonal antibodies targeting cancer: ‘magic bullets’ or just the trigger? Breast Cancer Res 3:86–90
Emmert S, Schneider TD, Khan SG, Kraemer KH (2001) The human XPG gene: gene architecture, alternative splicing and single nucleotide polymorphisms. Nucleic Acids Res 29:1443–1452
Erichsen HC, Chanock SJ (2004) SNPs in cancer research and treatment. Br J Cancer 90:747–751
Fishelson Z, Donin N, Zell S, Schultz S, Kirschfink M (2003) Obstacles to cancer immunotherapy: expression of membrane complement regulatory proteins (mCRPs) in tumors. Mol Immunol 40:109–123
Gelderman KA, Tomlinson S, Ross GD, Gorter A (2004) Complement function in mAb-mediated cancer immunotherapy. Trends Immunol 25:158–164
Golay J, Zaffaroni L, Vaccari T, Lazzari M, Borleri GM, Bernasconi S, Tedesco F, Rambaldi A, Introna M (2000) Biologic response of B lymphoma cells to anti-CD20 monoclonal antibody rituximab in vitro: CD55 and CD59 regulate complement-mediated cell lysis. Blood 95:3900–3908
Hakulinen J, Meri S (1998) Complement-mediated killing of microtumors in vitro. Am J Pathol 153:845–855
Hansen MH, Ostenstad B, Sioud M (2001) Antigen-specific IgG antibodies in stage IV long-time survival breast cancer patients. Mol Med 7:230–239
Harjunpaa A, Junnikkala S, Meri S (2000) Rituximab (anti-CD20) therapy of B-cell lymphomas: direct complement killing is superior to cellular effector mechanisms. Scand J Immunol 51:634–641
Jager D, Jager E, Knuth A (2001) Immune responses to tumour antigens: implications for antigen specific immunotherapy of cancer. J Clin Pathol 54:669–674
Jurianz K, Maslak S, Garcia-Schuler H, Fishelson Z, Kirschfink M (1999) Neutralization of complement regulatory proteins augments lysis of breast carcinoma cells targeted with rhumAb anti-HER2. Immunopharmacology 42:209–218
Kaplan E, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Kauppi M, Pukkala E, Isomaki H (1997) Elevated incidence of hematologic malignancies in patients with Sjogren's syndrome compared with patients with rheumatoid arthritis (Finland). Cancer Causes Control 8:201–204
Khan SG, Muniz-Medina V, Shahlavi T, Baker CC, Inui H, Ueda T, Emmert S, Schneider TD, Kraemer KH (2002) The human XPC DNA repair gene: arrangement, splice site information content and influence of a single nucleotide polymorphism in a splice acceptor site on alternative splicing and function. Nucleic Acids Res 30:3624–3631
Kishore U, Reid KB (2000) C1q: structure, function, and receptors. Immunopharmacology 49:159–170
Korb LC, Ahearn JM (1997) C1q binds directly and specifically to surface blebs of apoptotic human keratinocytes: complement deficiency and systemic lupus erythematosus revisited. J Immunol 158:4525–4528
Mellemkjaer L, Andersen V, Linet MS, Gridley G, Hoover R, Olsen JH (1997) Non-Hodgkin’s lymphoma and other cancers among a cohort of patients with systemic lupus erythematosus. Arthritis Rheum 40:761–768
Modrek B, Resch A, Grasso C, Lee C (2001) Genome-wide detection of alternative splicing in expressed sequences of human genes. Nucleic Acids Res 29:2850–2859
Onoe K, Iwabuchi K, Iwabuchi C, Tone S, Konishi J, Kawakami Y, Nishimura M (2002) Enhanced complement sensitivity of NK-T cells in murine thymus and spleen associated with presence of serum immunoglobulin. Immunobiology 206:377–391
Pantel K, Brakenhoff RH (2004) Dissecting the metastatic cascade. Nat Rev Cancer 4:448–456
Pardoll DM (1999) Inducing autoimmune disease to treat cancer. Proc Natl Acad Sci U S A 96:5340–5342
Peters-Golden M, Wise RA, Hochberg M, Stevens MB, Wigley FM (1985) Incidence of lung cancer in systemic sclerosis. J Rheumatol 12:1136–1139
Petry F, Loos M (2005) Common silent mutations in all types of hereditary complement C1q deficiencies. Immunogenetics 57:566–571
Posner JB (2003) Immunology of paraneoplastic syndromes: overview. Ann N Y Acad Sci 998:178–186
Racila E, Scheuermann RH, Picker LJ, Yefenof E, Tucker T, Chang W, Marches R, Street NE, Vitetta ES, Uhr JW (1995) Tumor dormancy and cell signaling. II. Antibody as an agonist in inducing dormancy of a B cell lymphoma in SCID mice. J Exp Med 181:1539–1550
Racila DM, Sontheimer CJ, Sheffield A, Wisnieski JJ, Racila E, Sontheimer RD (2003) Homozygous single nucleotide polymorphism of the complement C1QA gene is associated with decreased levels of C1q in patients with subacute cutaneous lupus erythematosus. Lupus 12:124–132
Ramsey-Goldman R, Mattai SA, Schilling E, Chiu YL, Alo CJ, Howe HL, Manzi S (1998) Increased risk of malignancy in patients with systemic lupus erythematosus. J Investig Med 46:217–222
Reid KB (1983) Proteins involved in the activation and control of the two pathways of human complement. Biochem Soc Trans 11:1–12
Roodman GD (2004) Mechanisms of bone metastasis. N Engl J Med 350:1655–1664
Sigurgeirsson B, Lindelof B, Edhag O, Allander E (1992) Risk of cancer in patients with dermatomyositis or polymyositis. A population-based study. N Engl J Med 326:363–367
Tan EM (2001) Autoantibodies as reporters identifying aberrant cellular mechanisms in tumorigenesis. J Clin Invest 108:1411–1415
Tan EM, Shi FD (2003) Relative paradigms between autoantibodies in lupus and autoantibodies in cancer. Clin Exp Immunol 134:169–177
Tazawa H, Okada F, Kobayashi T, Tada M, Mori Y, Une Y, Sendo F, Kobayashi M, Hosokawa M (2003) Infiltration of neutrophils is required for acquisition of metastatic phenotype of benign murine fibrosarcoma cells: implication of inflammation-associated carcinogenesis and tumor progression. Am J Pathol 163:2221–2232
von Ahsen N, Oellerich M (2004) The intronic prothrombin 19911A>G polymorphism influences splicing efficiency and modulates effects of the 20210G>A polymorphism on mRNA amount and expression in a stable reporter gene assay system. Blood 103:586–593
Walport MJ (2001) Complement. First of two parts. N Engl J Med 344:1058–1066
Webb KE, Martin JF, Cotton J, Erusalimsky JD, Humphries SE (2003) The 4830C>A polymorphism within intron 5 affects the pattern of alternative splicing occurring within exon 6 of the thrombopoietin gene. Exp Hematol 31:488–494
Zeng G, Li Y, El-Gamil M, Sidney J, Sette A, Wang RF, Rosenberg SA, Robbins PF (2002) Generation of NY-ESO-1-specific CD4+ and CD8+ T cells by a single peptide with dual MHC class I and class II specificities: a new strategy for vaccine design. Cancer Res 62:3630–3635
Zhu Y, Spitz MR, Amos CI, Lin J, Schabath MB, Wu X (2004) An evolutionary perspective on single-nucleotide polymorphism screening in molecular cancer epidemiology. Cancer Res 64:2251–2257
Acknowledgements
We gratefully acknowledge Melinda Andreski for patient consenting and collection and coding of blood specimens. We thank Carol Scott-Conner, Jean Arndt, Mark Karwal and Susan Roman for helping identify potential subjects. Input from all members of our research group, especially Drs. Brian Link and James Wooldridge, is recognized and appreciated.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported in part by National Institute of Health grant R21-CA90822, Friends You Can Count On! grant 1-87093-00, and the Woody and Louise White Cancer Research Fund.
Rights and permissions
About this article
Cite this article
Racila, E., Racila, D.M., Ritchie, J.M. et al. The pattern of clinical breast cancer metastasis correlates with a single nucleotide polymorphism in the C1qA component of complement. Immunogenetics 58, 1–8 (2006). https://doi.org/10.1007/s00251-005-0077-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00251-005-0077-y