Abstract
The sequence of bacterial events that occurs during the colonization of the gastrointestinal tract may affect the future health of the host. A clear understanding of the colonization process of the human neonatal gut in developing countries is lacking because the few available studies were mostly performed using culture techniques. Using molecular approaches, this study analyzed the fecal microbiota of children of low socioeconomic status in São Paulo, Brazil, during their first year of life. We collected fecal samples of healthy children at 3, 6, and 12 months of life. Total DNA was extracted directly from feces, and the bacteria-specific primers 27F-1492R were used to construct 16S rRNA libraries. Clones were randomly selected and partially sequenced. The main phylogenetic groups identified at 3 months were Streptococcus, unidentified bacteria, and Escherichia. At 6 months, Escherichia remained predominant, while the unidentified bacterial population increased significantly. At 12 months, a more complex composition of fecal microbiota was observed, represented by unidentified bacteria and microorganisms found at low rates at earlier ages. The genus Escherichia remained the most abundant microorganism (34 % relative abundance and 75 % prevalence). Principal component analysis (PCA) revealed changes in the composition of the microbiota at 6 months and an increase of diversity at 12 months of life. Bifidobacterium was identified by quantitative PCR (qPCR) and showed a high incidence in the microbiota at 3 months. The present results corroborate the global observation of inter-individual variability with an early establishment of microbial complexity at the end of the first year of life and highlight the presence of the Escherichia as abundant in microbiota composition of this group of children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human intestinal microbiota is a complex bacterial environment that closely interacts with host cells and nutrients [8]. Specific members of the intestinal microbiota are associated with beneficial effects, such as immunological modulation and colonization resistance; the microbiota also contributes to nutrition and metabolism [17, 47].
The microbiota, which is acquired during birth and throughout the first months of life, reaches its maturation at the end of the first year of life [35, 40]. During this colonization period, the intestinal bacterial content is influenced by the interaction of internal and mostly external factors that modulate its composition and function [43]. Principal among these factors are the mode of delivery [10], breast or formula feeding [4, 8], introduction of solid foods [41], bacterial load in the environment, diet [9, 14], and the use of antibiotics [45]. These factors will determine individual microbial profiles, which in turn could influence the future health of the individual [50].
The geographic region in which a child is born appeared to be more important on the gut microbial composition than any other parameter [14], in a way that seems to differ between children living in developed and developing countries. One explanation is the high levels of environmental contamination to which children in developing countries are exposed early in life [2, 4, 25, 27, 49], in contrast to the low bacterial exposure of children subjected to strict hygiene habits in developed countries. According to the hygiene hypothesis, stringent hygiene practices in developed countries can modify the initial microbial exposure and hence the pattern of the intestinal microbiota of infants, negatively impacting immune regulation and possibly leading to the increased incidence of allergic and autoimmune diseases observed in developed countries [36].
The study of intestinal microbiota gained importance a few decades ago, when molecular approaches provided sequence information from different ecosystems [28, 46]. In particular, analysis of the 16S ribosomal RNA gene provided an immensely powerful tool by which to determine the evolutionary interrelationships of microorganisms [6].
Although it is an expensive and labor-intensive methodology [44], phylogenetic analysis based on 16S rRNA library construction has been widely used to characterize human fecal microbiota over the last two decades [22, 28, 31]. The 16S rRNA library construction may result in a less sensitive assessment of bacterial diversity [24]; however, it gives a good phylogenetic/taxomonic assignments, revealing significant differences between members of the intestinal microbiota and permits the characterization of the most abundant organisms, which may be better adapted to their niche [39, 50].
Given the increasing number of studies comparing the microbiota composition of children from different countries, the present work was undertaken to determine, using library construction methodology and qPCR, the microbiota composition of group of children living in a low socioeconomic environment in São Paulo, Brazil, considering the supply of breast milk, diet, and intercurrent clinical factors. A few studies using culture methodology have already been conducted in Brazil [30, 33]; however, using molecular approaches, our group was the first to describe the fecal microbiota composition of Brazilian neonates [7].
Methods
Sample Collection
Ten children were enrolled in this study and were selected as previously described [7]. The results of the 16S rRNA library construction from this group at the first month of life have already been described [7]. In this paper, the microbial compositions at 3, 6, and 12 months of age were analyzed. Fecal samples were collected from each child, at each time point. A medical appointment was also scheduled at each collection time. Information about breastfeeding, type of food consumed, eventual illness, and social or economic disorders were obtained monthly for each child by a pediatrician. The mothers were instructed to collect the fecal sample immediately after elimination with a standardized sterile spoon, place it in a sterile plastic container, and keep it in a freezer (−20 °C) until the appointment some hours later. Samples were transported all the way to the laboratory in an ice-filled polystyrene container.
Clinical Information
The babies enrolled in this study were vaginally delivered at the University Hospital of the University of São Paulo (HU-USP). They had uneventful births, had no associated morbidities, were full-term, and had adequate birth weights. The families belonged to low socioeconomic communities. In general, the parents had little schooling and low incomes; families lived in multi-habitation homes, and some of them lived in slums. These communities had electricity and running water, although access to water in each home varied. The sewer system was inadequate. Six of the ten babies were exclusively breastfed from birth until 5 months of age; the other four babies were fed either breast milk and formula or only formula starting at the second or third month, with the introduction of soft foods such as yogurt and baby food (with vegetables and meat) at 3 or 4 months (Table 1). After 6 months, all the children had a diverse solid diet that included meat, grains (rice, beans, peas, and lentils), wheat flour, fiber (greens), fruits, milk (formula and/or breast milk) and yogurt. Five of the six children who were breastfed until 5 months of age received oral antibiotics once or twice during the first year of life. Among the children who were not exclusively breastfed before 5 months of age, one received oral antibiotics during the first year of life (Table 1). The antibiotics were prescribed to treat respiratory infections, such as bronchiolitis, pneumonia, sinusitis, and otitis, for 7 or 10 days (Table 1).
DNA Extraction and 16S rRNA Amplification
DNA was extracted from stools using the QIAamp DNA Stool Mini-Kit (Qiagen, Canada) according to the manufacturer’s instructions. Two bacteria-specific primers, 27F (5′AGA GTT TGA TCC TGG CTC AG 3′) and 1492R (5' GGT TAC CTT GTT ACG ACT T 3′), were used to amplify the 16S rRNA gene coding region [20]. Amplification reactions were performed as described previously [20], and optimized in a total volume of 100 μL containing 180 ng of DNA extracted from each fecal sample, using a Platinum Taq DNA Polimerase (Invitrogen). The PCR amplifications were performed using the following program: 94 °C for 5 min, followed by 35 cycles of 94 °C for 45 s, 62 °C for 1 min, 68 °C for 2 min, and a final extension period of 68 °C for 10 min. The amplified 16S rRNA was purified with an UltraClean PCR kit (Invitrogen, USA).
Cloning the 16S rRNA Library
The purified PCR products were ligated into a pCR®2.1 TOPO plasmid vector and transformed into competent DH5α Escherichia coli cells using an Original TA Cloning Kit (Invitrogen, USA). 16S rRNA libraries were constructed for each time point (3, 6, and 12 months). After bacterial transformation, approximately 90 clones from each child at each time point were selected, and their lysates were used as the template in an amplification reaction using the M13 primers supplied in the cloning kit.
DNA Sequencing and Phylogenetic Analysis
The amplicons obtained as described above were purified with an UltraClean PCR kit (Invitrogen, USA). The products were analyzed using an automated MegaBACE 1000 DNA Analysis System (GE Healthcare, USA) and Cimarron 3.12 Base Caller (Cimarron Software Inc., USA), and sequencing reactions were performed using the T7 primer supplied in the cloning kit. Sequencing quality was analyzed using an online version of Phred software (http://asparagin.cenargen.embrapa.br/phph/), and nucleotides with a Phred score lower than 10 were discarded. Qualified sequences were manually edited with BioEdit software, v7.0.5.3 [19], to remove the vector and primer sequences. Chimeric artifacts were checked by the Chimera Slayer algorithm on Mothur v1.13.0 [42] using a Silva-based alignment database as a reference. The phylogenetic affiliations of the resulting sequences (approximately 450 bp and larger) were determined using the Classifier program of the Ribosomal Database Project (RDP) [48] and were confirmed by BLASTn comparison using the NCBI GenBank database.
The Mothur program was also used to estimate the microbial diversity by Operational Taxonomic Unit (OTU)-based approaches (ACE and Chao1 richness estimators, Shannon and Simpson diversity indices) and hypothesis-based approaches (Libshuff statistics and UniFrac distance comparison) [42]. The sequences were aligned using the Silva 102 SSU Reference database as a template [37], and a Phylip distance matrix file was generated to cluster the sequences into OTUs. The diversity analysis at the genera level was based on an OTU definition of at least 95 % sequence similarity. A Venn diagram was drawn to show the number of shared and unique OTUs in each sample. Phylogenetic trees were constructed using ARB software [26] with the neighbor-joining method and Felsenstein correction. A phylogenetic tree of only the non-chimeric clone sequences was subjected to weighted and unweighted UniFrac statistics, which tested the hypothesis that a group of sequences (that is, branches of a phylogenetic tree) may be unique to any sample. Bonferroni correction was used to adjust the p value for Libshuff and UniFrac tests, and therefore a p < 0.0167 (0.05 divided by the number of pair-wise comparisons) was considered significant. Principal components analysis (PCA) was performed with the software Canoco 4.56 (Microcomputer Power, Ithaca, NY, US) to test correlations between samples (child) and bacterial diversity (abundance of identified genera). In order to analyze specific child–bacteria correlations, PCA was conducted separately with 3-, 6-, or 12-month samples. In addition, samples from each time point were pooled and tested as an age vs. genera PCA (e.g., the sequences of all children at 3 months were mixed and considered as a unique sample).
Data Presentation
The relative abundance was calculated as the percentage of sequences obtained for a specific bacterial genus in relation to the total number of sequences recovered at each time point. The distribution of the abundances of each genus was graphically presented. The prevalence was calculated as the percentage of neonates in the group that harbored a specific bacterial genus.
Real-Time PCR
Bifidobacterium was not detected in the fecal samples using the 16S rRNA library technique. Therefore, real-time PCR was used to detect the presence of Bifidobacterium spp. in fecal samples. The primers and probe were the same as those validated by Furret et al. [16]. The amplification reaction was conducted in a total volume of 50 μL containing 1x TaqMan Universal PCR Master Mix (Applied Biosystems, Foster City, CA), 300 nmol/L of both primers, 150 nmol/L TaqMan probe, and 0.2 ng of the purified target DNA. The amplification reactions were performed using the following program: 50 °C for 2 min, 95 °C for 10 min and 42 cycles of 95 °C for 15 s and 60 °C for 1 min. The reactions were conducted in an Applied Biosystems Prism 7000 sequence detection system (Applied Biosystems, Foster City, CA). To quantify the copy number of Bifidobacterium 16S rRNA (rrn) in the fecal samples, standard curves were determined by correlation of the rrn gene copy number and threshold cycle (Ct) values for a 10-fold serial dilution of Bifidobacterium animalis subsp. lactis HN019. The data quantification was expressed as the mean and range of the values encountered in the group.
Nucleotide Sequence Accession Numbers
The nucleotide sequences reported in this paper appear in the DDBJ, EMBL, and GenBank nucleotide sequence databases with the following accession numbers: 3 months—JX136918 to JX136953, 6 months—JX136869 to JX136917, and 12 months—JX548099 to JX548220.
Ethical Considerations
The research was approved by the Ethics Committee of the HU-USP (under registration number 574/05). All mothers enrolled in the research signed an informed consent form.
Results
16S rRNA Library Construction
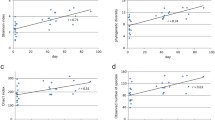
Approximately 2,572 clones were obtained for the constructed 16S rRNA library. After excluding low-quality and chimeric sequences, 2,225 sequences were gathered, each of which encompassed approximately 450 bp from the 5′ end of the 16S rRNA; these sequences were used to analyze the prevalence and relative abundance of microbes at each time point (Table 2, Fig. 1). Diversity indices were estimated using only the forward-aligned sequences (1,165 sequences, Table 3). Six phyla were identified in the phylogenetic analysis: Bacteroidetes, Firmicutes, Fusobacteria, Proteobacteria, Actinobacteria, and Verrucomicrobia. Sequences were identified up to genera by comparing to type-strain sequences in the RDP (Ribosomal Database Project) and Genbank reference databases. A total of 70 type-strain reference sequences were used to assign taxonomy of the sequences from the 3- to 12-month samples. Sequences similar to the genus Escherichia were the most abundant, with 401 clones for the 3- to 12-month period (Fig. 1). Some OTUs aligned with maximum identity and coverage to sequences designed as “uncultured bacteria” at GeneBank, which the identities had not, or could not be established by the time of analysis. In this work, these sequences were denominated as “unidentified bacteria”. Their phylogenetic identities are represented from multiple branches of the phylogenetic tree (Fig. 4)
Bacterial profile of the 16S rRNA library constructed using fecal samples from a group of 10 children. The sequences were grouped into genera. The data shown were pooled for each time point. 1: analysis point at 3 months of life; 2: analysis point at 6 months of life; 3: analysis point at the 12 months of life
Sample Data
The obtained sequences were pooled for a monthly age analysis, with a number of different samples in each pool. At 3 months, a total of 614 sequences were obtained from fecal samples from the 10 children. The genus Escherichia was predominant (30 % relative abundance and 86 % prevalence), followed by Streptococcus (22 % relative abundance and 86 % prevalence) (Table 2, Fig. 1). The strict anaerobes Bacteroides and Clostridium were detected at low rates of abundance (2 and 10 % relative abundance), despite the fact that Bacteroides were found in almost half of the study group (43 % prevalence). The same phenomenon was observed for Lactobacillus (5 % relative abundance and 71 % prevalence), which exhibited low rates of abundance but high prevalence among the children. The group of the “unidentified bacteria” was detected in 86 % of the samples (Fig. 1, Table 2). At 6 months, the predominance of Escherichia was still observed, with 40 % relative abundance and 100 % prevalence. Compared to the profile observed at 3 months of life, there was a high increase in unidentified bacteria (29 % relative abundance and 100 % prevalence); however, there was a decrease in the genus Streptococcus (5 and 67 %). The profiles of Klebsiella (6 and 67 %), Lactobacillus (6 and 44 %), Veillonella (4 and 56 %), and Bacteroides (2 and 44 %) at 6 months were similar to those at 3 months. At 12 months of age (Fig. 1, Table 2), we observed increased complexity in the fecal microbial composition, as evidenced by high colonization of unidentified bacteria (38 and 100 %) and microorganisms classified as “other” (7 and 89 %), such as Akkermansia, Citrobacter, and Ruminococcus, which were found at low rates at earlier ages. At 1 year of age, the genus Lactobacillus showed a marked reduction, with a frequency of colonization of 1 % and a relative abundance of 11 %. As at all-time points, the genus Escherichia remained the most abundant microorganism (33 and 78 %).
Microbial Profile According to the Supply of Breast Milk
The data from the libraries were classified into two groups: those from children who were exclusively breastfed until 5 months of age (group 1) and those from children who received artificial formula, and/or other types of food before 5 months of age (group 2) (Table 1). The microbial profile of group 1 was predominantly composed of Escherichia and unidentified bacteria, with fluctuations over the months but without changes in the frequency of colonization or abundance. Children from group 2 exhibited a diverse fecal microbial profile that was distinct from that of group 1, suggesting the interference power of early weaning for the establishment of microbiota in the first months of life. Based on the results described above, we constructed one table with information for each time point about the prevalence of the major bacterial genera identified in this study (Table 3). In group 1, the genera Bacteroides, Veillonella, and Lactobacillus were prevalent at 3, 6, and 12 months. In group 2, Clostridium and Streptococcus were prevalent, but Lactobacillus was absent. The data at 6 months revealed differences between the two groups, suggesting the impact of breast milk on microbial composition at this age; however, there was no difference between these two groups at 12 months of age.
Real-Time PCR of Bifidobacteria
Real-time PCR for Bifidobacterium detection was conducted because the 16S rRNA primers used in the cloning library were not able to amplify Bifidobacterium sequences. Using this approach, Bifidobacterium was detected at every studied time point. However, just one child (no. 17) did not show counts of Bifidobacterium, only at the sixth month of life, after 10 days treatment with amoxicillin (Table 1). At the 12th month, Bifidobacterium count in that child was found at 1.3 × 1011 copies per milligram of DNA. Quantification yielded counts that ranged from 1.0 × 1010 to 1.15 × 1013 copies per milligram of DNA at 3 months (median value of 2.5 × 1012 copies per milligram of DNA), from zero to 3.97 × 1011 copies per milligram of DNA at 6 months (median value of 1.93 × 1011 copies per milligram of DNA) and 2.68 × 108 to 4.29 × 1011 copies per milligram of DNA at 12 months (median value of 2.62 × 1011 copies per milligram of DNA).
Multivariate Analysis of Clone Libraries
The changes in childhood fecal communities over time (3 through 12 months) were analyzed by PCA using the abundance data (number of sequences) for each child. At 3 months, the fecal microbial profile was composed of a main, central group of four children (children 2, 3, 14, and 15) who exhibited a pattern influenced by the presence of highly abundant genera (such as Veillonella, Lactobacillus, Prevotella, Bacteroides, and Enterobacter) and most of the low-abundance or rare genera (Fig. 2a). Nevertheless, three children did not belong to this main group because their profiles were influenced by a high abundance of specific genera, such as Clostridium (child 1), Streptococcus (child 6), and Escherichia (child 12). Pediatric reports for these three children indicated poor hygiene practices and child care, the use of a pacifier or antibiotics (child 12—Table 1). At 6 months, each child presented a different microbial community, which resulted in a broader spread of the samples along the PCA axes (Fig. 2b). The PCA analysis of these 6-month-old children suggests a transition profile in the composition of fecal microbiota at this age. Finally, at the end of the first year of life, the microbial profile revealed a main group comprising all but two of the children (children 6 and 12) (Fig. 2c); pediatric reports indicated the use of antibiotics at the seventh (child 6) and ninth (child 12) months (Table 1). Based on the PCA analysis of age vs. genera (Fig. 2d), the microbiota at 3 months is mainly composed of Clostridium, Streptococcus, and some rare genera. At 6 months, this profile changes to high abundances of Enterobacteria, anaerobic bacteria, and different rare genera. Later, at the end of the first year of life, this pattern changes again and includes a predominance of unidentified bacteria, Escherichia, Veillonella, and other genera, demonstrating a succession of microbial communities in the human intestine during this time.
α and β Diversity of Fecal Microbiota
We analyzed the richness and diversity of the microbiota by comparing groups at the three time points. The α diversity indices, which estimate the richness (Ace and Chao1) and diversity (Simpson and Shannon) [42] of a single sample, were calculated for each time point. The coverage rates of the 16S rRNA libraries were higher than 90 % for genera (95 % similarity cutoff), which is considered the minimum coverage necessary to analyze OTUs with confidence [23]. Richness and diversity estimates were higher at 12 months than at 3 or 6 months (Table 4). Interestingly, richness and diversity were lower in the 6-month group than in the 3-month group. Venn diagrams were constructed to better represent the results of shared richness between samples, which, according to a detailed analysis, represent the number of observed OTUs at each analysis point and the number of OTUs shared between groups (Fig. 3). The 12-month group had the most unique sequences (33 OTUs), followed by the 6-month (19 OTUs) and 3-month (14 OTUs) groups. Thirteen OTUs were shared among the three groups. Tests of hypotheses (β diversity) were performed with the groups to determine the probability of two or more communities sharing the same structure. The Libshuff test revealed that the community composition at each time point was significantly different (p < 0.001 for each pair-wise comparison), showing that no community was a subsample of another. In agreement with the Libshuff test, the UniFrac method (weighted and unweighted), which is based on phylogenetic information, demonstrated that each time point contains microbial communities with different structures (p < 0.001 for each pair-wise comparison). To assess the overall composition of the library, a phylogenetic tree was built with a representative sequence from each OTU (using 95 % similarity cutoff for genus) and the corresponding reference sequence from the RDP (Fig. 4). Overall, sequences were divided into six major phyla: Bacteroidetes, Firmicutes, Fusobacteria, Proteobacteria, Actinobacteria, and Verrucomicrobia. Although the highest number of genera (number of different OTUs) were from the phylum Firmicutes, the relative abundance (number of clones within each OTU) was much greater for the phylum Proteobacteria, most of which was represented by the genus Escherichia. An analysis of sequences most similar to unidentified bacteria revealed that 82 % of the clones were similar to bacteria within the phylum Firmicutes, 14 % were similar to the phylum Bacteroidetes and 4 % were similar to Proteobacteria.
Phylogenetic relationships among the OTUs detected in fecal samples from children. Black branches represent 3-month samples, gray branches represent 6-month samples, and white branches represent 12-month samples. Reference sequences are indicated by their taxonomic names, and unidentified clones are followed by their GenBank accession numbers
Discussion
The colonization of the gastrointestinal tract in children is a remarkable episode in the human life cycle. After birth, a rich and dynamic ecosystem develops within a most probably sterile environment. The evolution and symbiosis among the first microorganisms to colonize the intestinal mucosa and form a resident microbiota undoubtedly involve several interactions between the microbiota and the host, with important consequences for human health [35]. Indeed, understanding the infant intestinal microbiota may provide insights for the prevention of important diseases [8].
It has already been established that the human intestinal microbiota is dominated by the phyla Bacteroides and Firmicutes, whereas Proteobacteria, Verrucomicrobia, Actinobacteria, Fusobacteria, and Cyanobacteria are present in lower proportions [12]. In the present study, phylogenetic analysis of sequence data identified six phyla: Bacteroidetes, Firmicutes, Fusobacteria, Proteobacteria, Actinobacteria, and Verrucomicrobia. The phylum Firmicutes was found to have higher richness, in accord with other human intestinal microbiota studies [11, 29], but higher abundance was found for the phylum Proteobacteria, represented by the genus Escherichia.
The result of the Venn diagram indicates that 13 OTUs belonging to the genera Escherichia, Bacteroides, Streptococcus, Lactobacillus, Enterococcus, Veillonella, Enterobacter, Klebsiella, to the family Ruminococcaceae and Lachnospiraceae and to the phyla Bacteroidetes, Firmicutes, and Proteobacteria were common among the microbiota at 3, 6, and 12 months, suggesting that these microorganisms have a role in the development of the microbial profile. These data revealed an increase in microbial richness along with age, as evidenced by the number of OTUs at each time point analyzed. The 12-month group had the largest number of unique OTU, followed by the 6 and 3-month groups, suggesting that the succession of microorganisms during the development of the microbiota is a dynamic process involving the entry and replacement of microorganisms over time. Although using different molecular approaches, Favier et al. [15] and Roger and McCartney [40] observed similar data.
PCA analysis yielded corresponding results. At 3 months, the microbiota was composed mostly of environmental genera, such as Clostridium, members of the Enterobacteriaceae and Enterococcus [1]. At 6 months, all of the children were already eating solid foods and drinking infant formula with or without breast milk. Besides breast milk, solid food also introduces different microorganisms and is a more variable source of nutrients, which may causes disturbances in the established microbial community. At this time, the microbiota exhibited a transitional profile. Although each child presented a unique microbial pattern and variable colonization, at 12 months, the fecal microbiota exhibited a higher shared richness, suggesting a tendency to stabilization [15, 35]. According to Palmer et al. [35], the microbiota of children at approximately 1 year of age is different from that of infants but is very similar to that of adults.
The first intestinal colonizers are often facultative aerobic organisms such as Staphylococcus, Streptococcus, and enterobacteria. Subsequent colonizers tend to be strict anaerobes such as Eubacterium and Clostridium [35]. We previously described the microbial profile of newborns from a developing country [7] and demonstrated that the highest relative abundance identified in neonatal samples belonged to phylogenetic groups Escherichia and Clostridium, while Staphylococcus and Bacteroides were identified at low rates. From the third to the twelfth month of age, the abundance of Escherichia remained high, Staphylococcus was absent, and Bacteroides was identified at low rates. This pattern of colonization is in contrast to that observed in children living in developed countries [3, 5].
There was a significant and gradual increase in the abundance of unidentified bacteria during the first year of life; ranging from 21 % at the 3rd month to approximately 40 % of the microbiota in children at the 12th month of life. Throughout the first year, unidentified bacteria exhibited higher richness and diversity and were predominantly composed of bacteria from the phylum Firmicutes, indicating the evolution of complexity in the fecal microbiota.
E. coli is one of the first colonizers of the infant gut and is acquired from the mother’s fecal microbiota during delivery [4, 34]. E. coli colonizes the large intestine for prolonged periods because it expresses P fimbriae, and can adhere to colonic cells [34]. Notably, Escherichia was the predominant genus at each time point studied. The presence of Escherichia in the infant intestinal microbiota has been demonstrated previously [13], but here we report its presence in a higher abundance in a group of children living in a low socioeconomic environment in São Paulo, Brazil. A combination of external factors such as environmental contamination, found in their neighborhood and public childcares, and diversity of diet seems to facilitate the persistence and high abundance of Escherichia in Brazilian children throughout the first year of life.
As discussed previously [7], since the primers used in this study were not able to amplify Bifidobacterium DNA [7, 20, 21], qPCR was conducted in order to quantify this genera in children. The highest counts of Bifidobacterium were found in 3-month-old children, reflecting the role of breast milk in early microbial composition. The relation between the milk carbohydrates, such as lactose and other oligosaccharides, and the increase of health-promoting bacteria such as Bifidobacterium and Lactobacillus in intestinal microbiota is well established [18, 41]. As discussed above, the transitional profile of the microbiota at 6 months was also apparent in the Bifidobacterium counts, which reached their lowest values at this time. Bifidobacterium group are described as far as the predominant group detected in children feces [4, 14, 36, 38], mainly in pre-weaned infants, and the decreasing count of Bifidobacterium at later ages was already described [49], indicating that this group of Brazilian children has the same evolution of this genera in microbiota composition like elsewhere.
By contrast, Clostridium was identified with higher abundance during the first year of life in children who were weaned early, and it was already established that this genus is most prevalent in infants who are fed milk formula [1]. Previous study has reported that Clostridium species are related to the regulation of some host metabolic pathways [32], and it is abundant in gut microbiota of healthy adults [20, 21]. Since the diversity analysis was done at the genera level, we could not associate diet and environment factors to specific pathogenic Clostridium species, as Clostridium difficile and Clostridium perfringes. However, in this cohort of babies, Clostridium presence might implicate a transition towards an adult-like gut microbiota.
The effect of the antibiotic on fecal microbiota composition of this group of children did not show a unique pattern over the months studied. We can observe changing in the microbiota profile in some children in relation to the group in the same period, as evidenced in children 6, 12, and 17. According to some authors, antibiotic treatment causes disturbance in the expected patterns of Bifidobacterium species and an overgrowth of enterobacteria could be seen [14, 45]. Our findings suggest that the effect of the antibiotic may also be subjected to individual variability of the intestinal microbiota.
The use of library construction and of qPCR methodology allowed the preliminary identification of fecal microbiota from Brazilian children. The present results corroborate the global observation of inter-individual variability with an early establishment of microbial complexity at the end of the first year of life, and highlight the presence of the Escherichia as abundant in microbiota composition of this group of children. These data may contribute to the worldwide understanding of how the geographic region and its environmental contamination influence the intestinal microbiota establishment.
References
Adlerberth I (2009) Factors influencing the establishment intestinal microbiota in infancy. In: Bier DM, German JB, Lönnerdal B (eds) Personalized nutrition for the diverse needs of infants and children. Nestlé Nutrition Workshop Series 63:13–33
Adlerberth I, Jalil F, Carlsson B, Mellander L, Hanson LA, Larsson P, Khalil K, Wold AE (1998) High turnover rate of Escherichia coli strains in the intestinal flora of infants in Pakistan. Epidemiol Infect 121:587–598
Adlerberth I, Lindberg E, Aberg N, Hesselmar B, Saalman R, Strannegård IL, Wold AE (2006) Reduced enterobacterial and increased staphylococcal colonization of the infantile bowel: an effect of hygienic lifestyle? Pediatr Res 59(1):96–101
Adlerberth I, Wold AE (2009) Establishment of the gut microbiota in Western infants. Acta Paediatr 98:229–238
Azad MB, Konya T, Maughan H, Guttman DS, Field CJ, Chari RS, Sears MR, Becker AB, Scott JA, Kozyrskyj AL, CHILD Study Investigators (2013) Gut microbiota of healthy Canadian infants: profiles by mode of delivery and infant diet at 4 months. CMAJ 185(5):385–394. doi:10.1503/cmaj.121189
Blaut M, Collins MD, Welling GW, Dore J, Van Loo J, De Vos W (2002) Molecular biological methods for studying the gut microbiota: the EU human gut flora project. Br J Nutr 87(2):S203–S211
Brandt K, Taddei CR, Takagi EH, Oliveira FF, Duarte RT, Irino I, Martinez MB, Carneiro-Sampaio M (2012) Establishment of the bacterial fecal community during the first month of life in Brazilian newborns. Clinics 67:113–123
Caicedo RA, Schanler RJ, Li N, Neu J (2005) The developing intestinal ecosystem: implications for the neonate. Pediatr Res 58:625–628
De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S, Collini S, Pieraccini G, Lionetti P (2010) Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. PNAS 107:14691–14696
Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N, Knight R (2010) Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habits in newborn. PNAS 107:11971–11975
Durban A, Abellan JJ, Jimenez-Hernandez N, Ponce M, Ponce J, Sala T, D’auria G, Latorre A, Moya A (2011) Assessing gut microbial diversity from feces and rectal mucosa. Microb Ecol 61:123–133
Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, Gill SR, Nelson KE, Relman DA (2005) Diversity of the human intestinal microbial flora. Science 308:1635–1638
Edwards CA, Parret AM (2002) Intestinal flora during the first months of life: new perspectives. Br J Nutr 88(1):S11–S18
Fallani M, Amarri S, Uusijarvi A, Adam R, Khanna S, Aguilera M, Gil A, Vieites JM, Norin E, Young D, Scott JA, Dore´ J, Edwards C, the INFABIO team (2011) Determinants of the human infant intestinal microbiota after the introduction of first complementary foods in infant samples from five European centres. Microbiology 157:1385–1392
Favier CF, Vaughan EE, de Vos WM, Akkermans ADL (2002) Molecular monitoring of succession of bacterial communities in human neonates. Appl Environ Microbiol 68(1):219–226
Furet JP, Firmesse O, Gourmelon M, Bridonneau C, Tap J, Mondot S, Doré J, Corthier G (2009) Comparative assessment of human and farm animal faecal microbiota using real-time quantitative PCR. FEMS Microbiol Ecol 68:351–362
Garrett WS, Gordon JI, Glimcher LH (2010) Homeostasis and inflammation in the intestine. Cell 140:859–870
Gibson GR, Roberfroid MB (1995) Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. J Nutr 125:1401–1412
Hall TA (1999) BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symp Ser 41:95–98
Hayashi H, Sakamoto M, Benno Y (2002) Phylogenetic analysis of the human gut microbiota using 16S rDNA clone libraries and strictly anaerobic culture methods. Microbiol Immunol 46:535–548
Hayashi H, Sakamoto M, Kitahara M, Benno Y (2003) Molecular analysis of fecal microbiota in elderly individuals using 16S r DNA library and T-RFLP. Microbiol Immunol 47:557–570
Hayashi H, Takahashi R, Nishi T, Sakamoto M, Benno Y (2005) Molecular analysis of jejunal, ileal, caecal and recto-sigmoidal human colonic microbiota using 16S rRNA gene libraries and terminal restriction fragment length polymorphism. J Med Microbiol 54:1093–1101
Lemos LN, Fulthorpe RR, Roesch LF (2012) Low sequencing efforts bias analyses of shared taxa in microbial communities. Folia Microbiol 57:409–413
Li L, Hsiao WW, Nandakumar R, Barbuto SM, Mongodin EF, Paster BJ, Fraser-Liggett CM, Fouad AF (2010) Analyzing endodontic infections by deep association with clinical and histopathologic findings. J Endod 36:1277–1288
Lindberg E, Adlerberth I, Hesselmar B, Saalman R, Strannegard IL, Aberg N, Wold AE (2004) High rate of transfer of Staphylococcus aureus from parental skin to infant gut flora. J Clin Microbiol 42(2):530–534
Ludwig W, Strunk O, Westram R, Richter L, Meier H, Yadhukumar, Buchner A, Lai T, Steppi S, Jobb G, Forster W, Brettske I, Gerber S, Ginhart AW, Gross O, Grumann S, Hermann S, Jost R, Konig A, Liss T, Lussmann R, May M, Nonhoff B, Reichel B, Strehlow R, Stamatakis A, Stuckmann N, Vilbig A, Lenke M, Ludwig T, Bode A, Schleifer KH (2004) ARB: a software environment for sequence data. Nucleic Acids Res 32:1363–1371
Lundequist B, Nord CE, Winberg J (1985) The composition of faecal microflora in breastfed and bottle fed infants from birth to eight weeks. Acta Paediatr Scand 74:45–51
Marchesi JR, Sato T, Weightman AJ, Martin TA, Fry JC, Hiom SJ, Wade WG (1998) Design and evaluation of useful bacterium-specific PCR primers that amplify genes coding for bacterial 16S r RNA. Appl Environ Microbiol 64:795–799
Mariat D, Firmesse O, Levenez F, Guimaraes V, Sokol H, Dore J, Corthier G, Furet JP (2009) The Firmicutes/Bacteroidetes ratio of the human microbiota changes with age. BMC Microbiol 9:123
Mello RM, Morais MB, Tahan S, Melli LC, Rodrigues MS, Mello CS, Scaletsky IC (2009) Lactobacilli and bifidobacteria in the feces of schoolchildren of two different socioeconomic groups: children from a favela and children from a private school. J Pediatr 85:307–314
Montesi A, Albiach RG, Pozuelo MJ, Pintado C, Goñi I, Rotger R (2005) Molecular and microbiological analysis of caecal microbiota in rats fed with diets supplemented either with prebiotics or probiotics. Int J Food Microbiol 98:281–289
Nicholson JK, Holmes E, Kinross J, Burcelin R, Gibson G, Jia W, Pettersson S (2012) Host-gut microbiota metabolic interactions. Science 336:1262–1267
Novak FR, Almeida JA, Vieira GO, Borba LM (2001) Colostro humano: fonte natural de probióticos? J Pediatr 77:265–270
Nowrouzian F, Hesselmar B, Saalman R, Strannegar IL, Aberg N, Wold AE, Adlerberth I (2003) Escherichia coli in infants’ intestinal microflora: colonization rate, strain turnover, and virulence gene carriage. Pediatr Res 54(1):8–14
Palmer C, Bik EM, Digiulio DB, Relman DA, Brown PO (2007) Development of the human infant intestinal microbiota. PLoS Biol 5:e177
Penders J, Thijs C, Vink C, Stelma FF, Snijders B, Kummeling I, Van Den Brandt PA, Stobberingh EE (2006) Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics 118:511–521
Pruesse E, Quast C, Knittel K, Fuchs BM, Ludwig W, Peplies J, Glockner FO (2007) SILVA: a comprehensive online resource for quality checked and aligned ribosomal RNA sequence data compatible with ARB. Nucleic Acids Res 35:7188–7196
Rastall RA (2004) Bacteria in the gut: friends and foes and how to alter the balance. J Nutr 134:2022S–2026S
Ricucci D, Siqueira JF Jr (2010) Biofilms and apical periodontitis: study of prevalence and coverage pyrosequencing. J Dent Res 89:980–984
Roger LC, Mccartney AL (2010) Longitudinal investigation of the faecal microbiota of healthy full-term infants using fluorescence in situ hybridization and denaturing gradient gel electrophoresis. Microbiology 156:3317–3328
Salminen SJ, Gueimonde M (2005) In: O. Hernell, J. Schmitz (eds) Feeding during late infancy and early childhood: impact on Health. Vevey/S. Karger AG, Basel. Nestlé Nutr Workshop Ser Pediatr Program 56:43–56
Schloss PD, Westcott SL, Ryabin T, Hall JR, Hartmann M, Hollister EB, Lesniewski RA, Oakley BB, Parks DH, Robinson CJ, Sahl JW, Stres B, Thallinger GG, Van Horn DJ, Weber CF (2009) Introducing mothur: open-source, platform-independent, community-supported software for describing and comparing microbial communities. Appl Environ Microbiol 75:7537–7541
Sekirov I, Russell SL, Antunes LC, Finlay BB (2010) Gut microbiota in health and disease. Physiol Res 90:859–904
Strausberg RL, Levy S, Rogers YH (2008) Emerging DNA sequencing technologies for human genomic medicine. Drug Discov Today 13:569–577
Tanaka S, Kobayashi T, Songjinda P, Tateyama A, Tsubouchi M, Kiyohara C, Shirakawa T, Sonomoto K, Nakayama J (2009) Influence of antibiotic exposure in the early postnatal period on the development of intestinal microbiota. FEMS Immunol Med Microbiol 56:80–87
Tannock GW (2001) Molecular assessment of intestinal microflora. Am J Clin Nutr 73:410S–414S
Vrieze A, Holleman F, Zoetendal EG, De Vos WM, Hoekstra JB, Nieuwdorp M (2010) The environment within: how gut microbiota may influence metabolism and body composition. Diabetologia 53:606–613
Wang Q, Garrity GM, Tiedje JM, Cole JR (2007) Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol 73:5261–5267
Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, Magris M, Hidalgo G, Baldassano RN, Anokhin AP, Heath AC, Warner B, Reeder J, Kuczynski J, Caporaso JG, Lozupone CA, Lauber C, Clemente JC, Knights D, Knight R, Gordon JI (2012) Human gut microbiome viewed across age and geography. Nature 486:222–227
Zoetendal EG, Collier CT, Koike S, Mackie RI, Gaskins HR (2004) Molecular ecological analysis of the gastrointestinal microbiota: a review. J Nutr 134:465–472
Acknowledgements
Financial support—FAPESP 08/53959-5 and 2011/51196-7 (Fundação de Amparo à Pesquisa do Estado de São Paulo) to CRT.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taddei, C.R., Oliveira, F.F., Duarte, R.T.D. et al. High Abundance of Escherichia During the Establishment of Fecal Microbiota in Brazilian Children. Microb Ecol 67, 624–634 (2014). https://doi.org/10.1007/s00248-014-0381-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00248-014-0381-x