Abstract
Background
Primary lymphoma of bone is an uncommon non-Hodgkin lymphoma. Magnetic resonance imaging (MRI) features of primary lymphoma of bone in children are not well described.
Objective
To identify typical MRI characteristics of pediatric primary lymphoma of bone at diagnosis and following treatment.
Materials and methods
Two pediatric radiologists retrospectively reviewed all imaging studies of 10 patients with biopsy-proven primary lymphoma of bone at presentation and after treatment. Anatomic location, number of sites, location within bone (epiphyseal, metaphyseal, diaphyseal), T1-weighted imaging margins, soft tissue mass, T2-weighted imaging appearance and enhancement pattern (homogeneous, heterogeneous, infarct-like), soft tissue edema, cortical disruption, and regional lymph nodes as seen on MRI as well as radiographic and positron emission tomography (PET) findings were recorded. Pathologic results, treatment plans, and outcomes at follow-up as detailed in the medical record were tabulated.
Results
Of 10 patients, age at diagnosis 8–17 years, median 15 years, 4 (40%) had multifocal disease. MRI revealed 20 total lesions in the 10 patients with femoral lesions most common, being present in 7 (70%) of patients. Eight (80%) patients had at least one lesion around the knee. Eight (80%) patients had 1 or more lesions involving an epiphysis and 5 (50%) had at least 1 lesion confined to the epiphysis. Seven (70%) showed infarct-like appearance on T2-weighted imaging; 7 (88%) of the 8 patients with post-contrast imaging had infarct-like enhancement. Six (60%) had sharp T1 margins, 3 (30%) had cortical disruption, 8 (80%) had at least mild soft tissue edema, and 1 (10%) had soft tissue mass. Three (30%) had at least 1 PET-positive regional lymph node. At follow-up (range 1–108 months, median 4.3 months), all had residual osseous abnormality on MRI with 6 (60%) maintaining an infarct-like or combination of infarct-like and T2 hyperintense appearance.
Conclusion
Our results in this series of pediatric primary lymphoma of bone identified several frequent MR imaging features. Multifocality, epiphyseal involvement (especially about the knee), infarct-like enhancement pattern, sharp T1 margins, and surrounding soft tissue edema should raise suspicion for primary lymphoma of bone. Following treatment, residual osseous abnormality is expected on MRI.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary lymphoma of bone is an uncommon non-Hodgkin lymphoma, usually diffuse large B-cell lymphoma, which accounts for approximately 5% of extranodal lymphomas and 3% of bone tumors in adults [1]. It is even less common in children [2], and has a strong male predominance [3]. This rarity combined with the nonspecific and often indolent clinical presentation may lead to a delay in diagnosis and advancement of disease [4]. PLB must be distinguished from the more common osseous metastatic lymphoma which arises within lymph nodes or solid organs. Unlike the far more common pediatric primary bone tumors, osteosarcoma and Ewing sarcoma, primary lymphoma of bone is not treated surgically but rather with chemotherapy often in combination with radiation therapy, similar to non-Hodgkin lymphoma at other sites, and is usually associated with a good outcome [5]. This distinction requires diagnostic percutaneous biopsy, the accuracy of which is aided by preprocedural suspicion of primary lymphoma of bone. At many institutions, flow cytometry and cytogenetics are performed only when the pathology department is alerted to the concern for lymphoma.
The prognosis for children and adolescents with primary lymphoma of bone is excellent, greater than 90% 5-year overall survival, substantially better than approximately 60% 5 year overall survival for osteosarcoma and Ewing sarcoma, and better than approximately 80% overall 5-year survival for non-osseous non-Hodgkin lymphoma [5]. Imaging assessment for response to therapy and for off-treatment surveillance is controversial. Positron emission tomography computed tomography (PET CT) may help guide biopsy in some cases [6]. Some advocate for local follow-up with radiography or MRI and systemic surveillance with whole-body PET/CT. Others recommend minimal post-treatment imaging because of the low risk of relapse and high rate of residual and incidental findings [7].
Imaging findings of primary lymphoma of bone at diagnosis described in adults typically include osseous destruction, soft tissue mass, metadiaphyseal location, and polyostotic disease in 20% [8, 9]. Reports of the imaging appearance of primary lymphoma of bone in children are few and primarily describe nonspecific bone marrow lesions that may be multifocal. Several studies report cases with lesions about the knee [10,11,12], but the distal radius [13, 14], maxilla [15], and cranial vault [16] have also been described. A large, primarily adult pathologic series of more than 800 patients with “non-Hodgkin lymphoma in bone” identified 20 patients with lower extremity involvement. These patients, compared to those with non-lower extremity osseous sites, were on average younger and had even better prognosis regardless of disease stage. Many of the patients had nonspecific sclerotic changes radiographically, but no magnetic resonance imaging (MRI) findings were reported [12]. One study of six children described MRI as useful only when radiographs are negative and to help guide biopsy [17]. Post-treatment imaging descriptions are even sparser. That study reported persistent MRI signal abnormalities in a few of their patients. A study of 25 adult patients with primary lymphoma of bone, during and after treatment, identified persistent osseous abnormalities for multiple years post-treatment despite disease remission [18]. Since surgical resection is not part of the treatment for local control of primary lymphoma of bone, awareness of the residual osseous features can avoid erroneous interpretation of residual or recurrent disease.
The goal of our investigation was to elucidate common MRI characteristics of primary lymphoma of bone at presentation and after treatment. These imaging features may allow the radiologist to suggest a diagnosis often not previously considered, and one that requires biopsy with appropriate specimen collection and urgent treatment to prevent spread.
Materials and methods
The electronic medical record search function (Citrix, Oracle Cerner, Austin, TX) and radiology report data base (Montage, Nuance Communications, Burlington, MA) of Boston Children’s Hospital, Boston, MA, was searched over a 22-year period (2000- 2022) for patients with biopsy-proven primary lymphoma of bone and MRI prior to diagnosis. Institutional Review Board (IRB) approval for medical record and imaging review was obtained. Patients with solid organ or distant lymph node involvement were excluded for potential osseous metastasis rather than primary lymphoma of bone. Twelve patients with biopsy-proven primary lymphoma of bone were identified, all of whom also had at least one post treatment MRI. All patients underwent bone marrow biopsies which excluded leukemia and widespread lymphoma. Two patients, 1 with non-diagnostic and 1 with minimally abnormal bone marrow biopsy results, were excluded from the study. All patients had PET (or gallium scintigraphy in one patient) to confirm disease localized to the bones and regional lymph nodes.
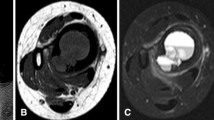
Two radiologists, a fellow (P.D.) with 2 years of pediatric radiology experience and a faculty radiologist (K.E.) with 25 years’ experience retrospectively reviewed the all pretreatment and posttreatment imaging independently. The following MRI characteristics were recorded: number of lesions; each lesion’s location within bone – epiphysis or epiphyseal equivalent exclusively , metaphysis/diaphysis, epiphysis, and metaphysis with transphyseal extension; T1 margins – sharp, ill-defined, combination (Fig. 1); enhancement pattern and appearance on fluid-sensitive images (T2 weighted or inversion recovery); soft tissue mass; soft tissue edema; cortical breakthrough; regional lymphadenopathy (defined as nodes larger than 1 cm in short axis). Multifocality was defined as 2 or more noncontiguous lesions within the same or separate bones. On fluid-sensitive sequences, lesions were classified as generally hyperintense to surrounding marrow and skeletal muscle, infarct-like with differential central and peripheral signal intensity (Fig. 1). The enhancement pattern on post-contrast T1 fat-suppressed images was described as infarct-like when peripheral enhancement surrounded central non-enhancing serpentine or geographic regions with or without a sequestrum (Fig. 2). Discrepancies between the two readers were resolved by consensus. The latest post-treatment MRI exam was reviewed for the same imaging features. Length of imaging follow-up was defined as time from the biopsy diagnosis to the last MRI. The MRI exams over the 22-year study period were performed on varied scanners, all 1.5-T or 3-T field strength.
A 15-year-old boy with left knee pain ultimately diagnosed as primary lymphoma of bone, pathology B cell lymphoblastic lymphoma. a Frontal radiograph of the left knee shows proximal tibial faint sclerosis and cortical thickening. b Coronal T1-weighted MR image demonstrates a lesion in the medial femoral condylar epiphysis and a second lesion in the proximal tibial epiphysis and metaphysis, crossing the physis. Both lesions have sharp margins with the adjacent normal fatty marrow. c Coronal T2 fat-suppressed MR image, the distal femoral epiphyseal lesion is fairly homogenously hyperintense to the surrounding marrow while the proximal tibial lesion is more heterogeneous with serpentine lower signal intensity areas surrounded by hyperintense areas, the infarct-like appearance. d Staging PET/CT coronal maximum intensity projection (MIP) image shows intense FDG avidity in the 2 left knee lesions as well as 2 additional lesions in the right distal femur. e Coronal T1 and (f) coronal T1 with fat suppression following intravenous gadolinium MR images of the contralateral right knee show noncontiguous distal femoral epiphyseal and metaphyseal lesions both with sharp T1 margins and homogeneous enhancement
A 15-year-old girl with left knee pain due to diffuse large B cell lymphoma (DLBCL). a Frontal radiograph of the knee shows a permeative distal femoral lesion with mixed lucent and sclerotic components. b Coronal T1 MR image confirms a large lesion centered on the closed physis with sharp margins. c Sagittal T2-weighted image shows that the lesion is heterogeneous on the with an enlarged lymph node in the popliteal fossa (arrow). d Post-contrast T1 fat-saturated image reveals the infarct-like enhancement pattern. e The PET/CT sagittal maximum intensity projection (MIP) image shows intense FDG avidity in the distal femoral lesion and the popliteal lymph node (arrow). The positive lymph node upstaged the patient and resulted in a more aggressive treatment plan
All patients underwent PET/CT at the time of diagnosis and at the end of treatment with the exception of the cohort’s first patient who had gallium scintigraphy. All images were reviewed for sites of disease and regional, distant nodal F-18 fluorodeoxyglucose (FDG) avidity. Radiographs were assessed for sclerosis, lucency, permeative lesion, or combination.
The patients’ medical records were reviewed for treatment protocols, start and end dates, and for documented response to therapy or disease progression as determined by the treating oncologist with incorporation of subsequent PET/CT results if performed.
Results
The 10 patients with primary lymphoma of bone and no bone marrow or non-osseous involvement had an age range of 8- 17 years at time of first imaging, median 15 years, and 8 (80%) were male. Biopsy results revealed diffuse large B-cell lymphoma (DLBCL) in 9 patients, anaplastic large cell lymphoma in 1 patient, and B-cell lymphoblastic lymphoma in 1 patient. Table 1 summarizes the clinical and imaging details for each of the 10 patients at diagnosis and at final imaging.
All 10 patients had radiographs of the symptomatic site prior to treatment. Three patients had no radiographic abnormality while the others showed sclerosis, lucency, cortical thickening, periosteal reaction, permeative change, and apparent bone infarct, usually with a combination of features. One patient with a proximal humeral lesion had a small lucency which was missed initially. She returned 6 months later with a pathologic fracture through a permeative lesion.
MRI protocols varied by anatomic location but all included long- and short-axis fluid-sensitive images. Pre-treatment post-contrast T1-weighted imaging with fat suppression was available in 8 of the 10 patients. MRI characteristics at presentation and posttreatment features for each patient are detailed in Table 1. The cumulative MRI results for all 10 patients are listed in Table 2. At diagnosis, 4/10 (40%) patients had multifocal osseous disease, 2 (20%) patients had 3 sites, 1 patient (10%) had 4 sites, and 1 patient (10%) had 5 sites of disease. MRI revealed 20 total lesions in the 10 patients (Fig. 3). At least one femoral lesion was present in 7/10 (70%) patients and 8/10 (80%) patients had at least one lesion around the knee (distal femur, proximal tibia, or patella). Eleven of the 20 lesions were located at the knee and only 1 lesion occurred in the upper extremity. Half of the 20 total lesions exclusively involved an epiphysis or epiphyseal equivalent. Eight (80%) patients had 1 or more lesions involving an epiphysis and 5/10 (50%) had at least 1 lesion confined to the epiphysis. Six of the lesions demonstrated transphyseal extension between the epiphysis and metaphysis. Only 3 lesions were confined to the metadiaphysis without epiphyseal extension.
Pretreatment, 7/10 (70%) of patients had lesions with an infarct-like appearance on fluid-sensitive images, while 7 of the 8 (87%) who received contrast had an infarct-like appearance in at least one lesion on post-contrast imaging. Six of ten (60%) had sharp T1 margins, 3/10 (30%) had cortical disruption, and 8/10 (80%) had at least mild soft tissue edema adjacent to the osseous disease. Only 1/10 (10%) had soft tissue mass; 3/10 (30%) had regional adenopathy.
PET/CT staging was performed pretreatment in 9/10 patients. All FDG avid osseous lesions were visible with MRI before or after the PET/CT. There were no FDG avid extra-osseous sites of disease other than in 3 patients with FDG avid regional popliteal lymph nodes, also present at MRI (Fig. 2). The earliest patient in the study had staging with gallium scintigraphy rather than PET/CT and also had no non-osseous disease.
All patients with single-site disease and no FDG avid regional lymph nodes were treated with 3 cycles of CHOP chemotherapy which included cyclophosphamide, doxorubicin, vincristine, and prednisone. Those with higher stage multifocal disease or single-site disease with regional FDG avid lymph nodes were treated with more aggressive regimens which included rituximab immunotherapy and intrathecal methotrexate in addition to systemic chemotherapy.
Post-treatment MRI follow-up ranged from 3 to 98 months (median 5.4 months). All lesions demonstrated residual osseous abnormality with 8 (67%) maintaining an infarct-like appearance on either fluid-sensitive or post-contrast images. No lesions showed increased size or increased soft tissue component, and no new lesions were identified. PET/CT was performed at the end of therapy in all 9 patients with pretreatment PET. All lesions had substantially decreased but not resolved FDG avidity and no new lesions developed. All patients remained disease free at clinical follow-up ranging from 2 to 9 years. No recurrence was seen regardless of unifocal or mutifocal disease.
Discussion
The rarity and nonspecific clinical presentation of primary lymphoma of bone may lead to delay in diagnosis. Our results in this series of MR imaging in children with primary lymphoma of bone reveal several frequently encountered features that may suggest the diagnosis. In a smaller study, Milks [17] described multifocality in up to half of patients, and our data concur. One of our patients had five osseous lesions at presentation. The location of these lesions also seems to be helpful. Metaphyseal and diaphyseal locations are considered more common and epiphyseal involvement is reportedly rare in primary lymphoma of bone [19]. The disease is generally not included in the pediatric epiphyseal lesion differential diagnosis list with chondroblastoma, infection, histiocytosis, and avascular necrosis being most common. A recent review of 49 pediatric long bone epiphyseal lesions included 2 patients with lymphoma, although it was not stated whether these patients had primary lymphoma of bone or osseous metastasis from systemic lymphoma [20]. In total, 80% of our patients had at least one epiphyseal or epiphyseal equivalent lesion (Fig. 4). These were more often sharply marginated without surrounding marrow edema typically seen with chondroblastoma, the most common pediatric epiphyseal tumor.
A 12-year-old boy with left ankle pain due to diffuse large B cell lymphoma (DLBCL). a Sagittal T1 MR image shows the left talar lesion with sharp posterior margins. b Staging PET/CT coronal maximum intensity projection identified additional FDG-avid disease in the contralateral right ankle and left knee. c Subsequent coronal proton density fat-suppressed MR image of the left knee and (d) sagittal T2 fat-saturated of the right ankle confirm the lateral femoral condylar and contralateral talar lesions. This patient has multifocal disease with epiphyseal (distal femur) and epiphyseal equivalent (talus) involvement
In addition to epiphyseal location, our results show a predilection for sites about the knee. More than half of the patients in this study had a lesion within the distal femur, proximal tibia, or patella (an epiphyseal equivalent). This is in contrast to primary lymphoma of bone in adults which involves the skull and spine in 50% of patients and the long bones, especially the femur, in the remaining 50% [9]. Adult long bone disease is reported to occur in the metaphysis and diaphysis, rarely extending to the epiphysis [9]. This distinction may relate to the increased vascularity in the epiphyses and metaphyses of the knee, the most rapidly growing region of the young skeleton.
The patients in our series had no consistent radiographic appearance of their osseous disease at the time of diagnosis. Three patients had no radiographic abnormality. The remaining patients had a combination of lucent, sclerotic, and permeative radiographic changes. While these findings often prompted further evaluation with MRI, they did not offer a specific diagnosis.
The majority of our patients’ lesions showed sharp (7/12) or combined sharp and indistinct margins (3/12) on T1-weighted images. In contrast to the reassuring appearance of sharp margins on radiographs of primary bone lesions, well-defined margins on T1-weighted MRI are ominous [21]. They indicate rapidly growing lesions with little surrounding inflammation. Indistinct T1 margins are typically seen with highly inflammatory, benign lesions such as chondroblastoma, osteoid osteoma, histiocytosis, and infection. Diffusely indistinct margins without any sharp T1 margins with adjacent normal marrow occurred in only 1 of our primary lymphoma of bone patients who also had cortical fracture.
The infarct-like or osteomyelitis-like appearance on post-contrast imaging seen in more than 80% of our patients is particularly interesting and not previously emphasized. In Mengiardi’s study of 25 adults with primary lymphoma of bone, only 7 patients underwent MRI and one was noted to have an infarct-like appearance following chemotherapy [18]. The pattern of peripheral enhancement surrounding serpiginous non-enhancing regions seen in our patients with untreated primary lymphoma of bone is more akin to the appearance seen in marrow infarction or infection than it is to the non-enhancing central necrosis often seen with primary bone tumors such as osteosarcoma or Ewing sarcoma. The reason for this appearance is unclear but may relate to ischemia of compressed marrow sinusoids rather than tumor necrosis.
Medullary ischemia may contribute to the persistent abnormalities seen at follow-up MRI in all our patients, even years after treatment. All of our long-term follow-up patients had no recurrence after therapy but showed residual MRI findings (Fig. 5). This is consistent with results of Borst [7] who reported persistent imaging findings in their pediatric patients with primary lymphoma of bone who were followed for months to years with a variety of imaging protocols including radiography, CT, MRI, and bone scintigraphy. They concluded that frequent imaging follow-up did not improve outcomes and, in fact, led to additional imaging for work-up of incidental findings. PET-CT may be more sensitive for assessment of response to therapy although FDG avidity may persist for months due to osseous remodeling [22]. PET-CT remains essential at diagnosis for the detection of asymptomatic multifocal disease and to exclude the more common nodal-origin non-Hodgkin’s lymphoma with osseous metastases. The more recent patients in our study underwent follow-up MRI and PET/CT at the termination of therapy with additional imaging only if symptoms arose.
A 16-year-old boy with primary lymphoma of bone of the right distal femoral epiphysis at diagnosis and at long-term follow-up. a Coronal T1 MR image at diagnosis shows sharp margins and small focus of medial transphyseal extension into the metaphysis. b Post-contrast T1 fat-suppressed coronal and (c) axial MR images show the infarct-like enhancement pattern. Eight years after treatment, MR imaging was performed for increased knee pain and concern for recurrence. d Sagittal proton density and (e) coronal T2 fat-suppressed MR images show postoperative change from the remote open biopsy, the medial femoral condyle deformity with chronic infarct-like appearance, and an overlying full thickness chondral defect (arrow), likely the cause of pain
At diagnosis, fewer of our patients demonstrated soft tissue mass (10%) and cortical disruption (30%) than reported in studies of adults with primary lymphoma of bone [23]. Surrounding soft tissue edema was also infrequent in our group. Cortical disruption, soft tissue mass, and soft tissue edema all resolved with treatment.
Imaging findings at the time of diagnosis impacted treatment in our patients. Those with one osseous site of disease received standard CHOP chemotherapy. Those with multiple osseous sites or regional lymph node involvement were upstaged and intrathecal chemotherapy as well as rituximab immunotherapy were added to their treatment plan.
Our study is limited by a small number of patients, necessitated by the low incidence of the disease, but remains the largest assessment of MRI features in children with primary lymphoma of bone. Additionally, follow-up imaging frequency and modality varied due to the lack of consensus about response to treatment assessment. Given the long time period considered, clinical follow-up varied. This limits ability to assess for long-term remission and/or cure, but it is reassuring that none had definitively failed treatment, consistent with the published high rate of response to therapy in pediatric primary lymphoma of bone. Lastly, the radiologists retrospectively reviewing the MR images could not be blinded to the diagnosis in this study exclusively focused on primary lymphoma of bone. Review of the images, rather than reliance upon the original MR report, was necessary to insure assessment and categorization of all recorded imaging features. Multiple MRI scanners of varied generations are a limitation for our study, as all studies with a lengthy time course. The 22-year study period was necessary to obtain a sufficient number of patients with this fairly rare subset of lymphoma. As we did not perform any quantitative MR imaging assessments in our study, scanner variation likely has minimal impact upon the qualitative MR appearance of the lesions.
Conclusions
Primary bone lymphoma is an uncommon but highly treatable malignancy in children. The diagnosis should be considered when children and adolescents, especially boys, present with painful intra-osseous lesions which by MR imaging are multifocal, epiphyseal, involve the lower extremity, especially the knee, or demonstrate an infarct-like appearance. Bone marrow abnormalities persist on long-term follow-up imaging. Consequently, follow-up MRI off treatment may be of limited utility.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author upon request.
References
Bhagavathi S, Fu K (2014) Primary lymphoma of bone: a review. Semin Diagn Pathol 31:48–52
Glotzbecker MP, Kersun LS, Choi JK et al (2006) Primary non-Hodgkin’s lymphoma of bone in children. J Bone Joint Surg Am 88:583–94
Huebner-Chan D, Fernandes B, Yang G, Lim MS (2001) An immunophenotypic and molecular study of primary large B-cell lymphoma of bone. Mod Pathol 14:1000–7
Demircay E, Hornicek FJ Jr, Mankin HJ, Degroot H 3rd (2013) Malignant lymphoma of bone: a review of 119 patients. Clin Orthop Relat Res 471:2684–90
Lones MA, Perkins SL, Sposto R et al (2002) Non-Hodgkin’s lymphoma arising in bone in children and adolescents is associated with an excellent outcome: a Children’s Cancer Group report. J Clin Oncol 20:2293–301
Moritani K, Nakano N, Yonezawa S et al (2018) Usefulness of positron emission tomography-CT for diagnosis of primary bone marrow lymphoma in children. Pediatr Hematol Oncol 35:125–130
Borst AJ, States LJ, Reilly AF, Rheingold SR (2013) Determining response and recurrence in pediatric B-cell lymphomas of the bone. Pediatr Blood Cancer 60:1281–6
Mulligan ME, McRae GA, Murphey MD (1999) Imaging features of primary lymphoma of bone. AJR Am J Roentgenol 173:1691–7
Weber MA, Papakonstantinou O, Nikodinovska VV, Vanhoenacker FM (2019) Ewing’s sarcoma and primary osseous lymphoma: spectrum of imaging appearances. Semin Musculoskelet Radiol 23:36–57
Cıraklı A, Elli M, Dabak N et al (2014) Evaluation of primary bone lymphoma and the importance of positron emission tomography. Acta Orthop Traumatol Turc 48:371–8
Suo H, Fu L, Wang Z et al (2020) Primary lymphoma of the tibia in children: Two case reports. Medicine 99:e18807
Subik MK, Herr M, Hutchison RE et al (2014) A highly curable lymphoma occurs preferentially in the proximal tibia of young patients. Mod Pathol 27:1430–1437
Poggio AD, Facchetti L, Ranza A et al (2018) Primary lymphoma of the distal radius of a child: imaging features. Radiol Case Rep 25;13:1279–1284
Huan Y, Qi Y, Zhang W, Chu J (2017) Primary bone lymphoma of radius and tibia: a case report and review of literature. Medicine 96:e6603
Zou H, Yang H, Zou Y et al (2018) Primary diffuse large B-cell lymphoma in the maxilla: a case report. Medicine 97:e10707
Bhatoe HS, Ambastha R (2016) Primary non Hodgkin’s lymphoma of the cranial vault in a child. J Neurooncol 126:209–211
Milks KS, McLean TW, Anthony EY (2016) Imaging of primary pediatric lymphoma of bone. Pediatr Radiol 46:1150–7
Mengiardi B, Honegger H, Hodler J et al (2005) Primary lymphoma of bone: MRI and CT characteristics during and after successful treatment. AJR Am J Roentgenol 184:185–92
Fox MG, Marti JK, Bachmann KR et al (2015) Epiphyseal presentation of non-Hodgkin’s lymphoma of bone in two pediatric patients–one with primary lymphoma of bone. Skeletal Radiol 44:587–95
El-Ali AM, Coblentz A, Degnan AJ (2020) Solitary long-bone epiphyseal lesions in children: radiologic-pathological correlation and epidemiology. Pediatr Radiol 50:1724–1734
Inarejos Clemente EJ, Navarro OM, Navallas M et al (2022) Multiparametric MRI evaluation of bone sarcomas in children. Insights Imaging 13:33
Paul MR, Kuo DJ (2018) Challenges of assessing response to therapy in non-Hodgkin’s lymphoma of the bone. Case Rep 2018:bcr-2017-223538
Heyning FH, Kroon HM, Hogendoorn PC et al (2007) MR imaging characteristics in primary lymphoma of bone with emphasis on non-aggressive appearance. Skeletal Radiol 36:937–44
Author information
Authors and Affiliations
Contributions
KE conceived of the study concept. Both PD and KE interpreted the images, collected and analyzed the data, and drafted and revised the manuscript. Both authors reviewed and approved of the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Duffy, P., Ecklund, K. MR features of primary bone lymphoma in children. Pediatr Radiol 53, 2400–2410 (2023). https://doi.org/10.1007/s00247-023-05772-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05772-w