Abstract
Background
Contrast-enhanced ultrasound (US) of the bowel wall has been suggested as an alternative imaging modality for the follow-up of children with Crohn disease.
Objective
To evaluate the diagnostic performance of contrast-enhanced US in the estimation of Crohn disease activity in children with histopathology as the reference standard.
Materials and methods
In 24 children with Crohn disease confirmed on histopathology, disease activity was evaluated on 40 bowel segments using US score and subjective and quantitative contrast-enhanced US evaluation. Contrast-enhanced US evaluation included enhancement pattern analysis with a graphic representation of log time-intensity curve and calculation of kinetic parameters with the definition of thresholds for disease activity, as determined by receiver operating characteristics curve analysis. The diagnostic accuracy of US with colour Doppler imaging and subjective and quantitative contrast-enhanced US were calculated.
Results
Moderate or severe inflammation was identified in 18 segments and remission or mild inflammation was identified in 22 segments on histopathology. The quantitative contrast-enhanced US, namely the peak enhancement value, had 72.2% sensitivity (95% confidence interval [CI] 46.5–90.3), 100% specificity (95% CI 84.6–100.0) and 87.5% diagnostic accuracy (95% CI 73.2–95.8) in predicting moderate or severe grade inflammation at histopathology. The sensitivity, specificity and diagnostic accuracy of subjective contrast-enhanced US were 77.8% (95% CI 52.4–93.6), 77.3% (95% CI 54.6–92.2) and 77.5% (95% CI 61.6–89.2), respectively, and of US with colour Doppler imaging were 55.6% (95% CI 30.8–78.5), 86.4% (95% CI 65.1–79.1) and 72.5% (95% CI 56.1–85.4), respectively.
Conclusion
Quantitative contrast-enhanced US has the potential of becoming a complementary method in the evaluation of Crohn disease activity in children. Fibrosis may affect peak enhancement results and underestimate inflammatory activity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Crohn disease is a chronic relapsing inflammatory bowel disease with increasing incidence in children and adolescents. The use of novel therapies requires repetitive imaging to assess disease activity and complications and to monitor therapeutic response [1]. We can assess inflammation of the bowel wall with ultrasound (US) and colour Doppler imaging with accuracy comparable to computed tomography (CT) enterography and magnetic resonance (MR) enterography [2,3,4]. Ultrasound has many advantages. There is no need for bowel preparation, sedation or anaesthesia, and it is a radiation-free method, all of which are of particular importance for the paediatric population. However, despite the use of colour Doppler imaging, its accuracy in detecting slow-moving blood flow in small vessels and vascularity in deep-lying bowel segments is low [2], and therefore the estimation of disease activity is less precise. Contrast-enhanced US uses the intravenous administration of a microbubble contrast agent to enhance the bowel wall and mesentery. The different patterns of contrast enhancement, the creation of time-intensity curves and the calculation of different quantitative parameters yield subjective and objective demonstrations of inflammation [5, 6].
To the best of our knowledge, there are no dedicated contrast-enhanced US studies for the evaluation of Crohn disease activity in children. Previous reports include five studies with mixed populations of children older than 16 years and adults [7] and one case report in a 13-year-old boy [8]. Children have significant physical, hemodynamic and tissue differences in comparison to adults. The influence of blood pressure and tissue attenuation on quantification of perfusion with contrast-enhanced US is well documented but not yet established for children. Lower blood pressure and higher heart rate directly impact the mean size of the microbubble and the resonant frequency of the contrast agent [9]. Furthermore, children’s distinct body habitus might alter the attenuation properties of the tissues preceding the organ of interest. These patient-related factors affect the imaging results and should not be simply extrapolated to the paediatric population.
The purpose of our study was to evaluate the diagnostic accuracy of US with colour Doppler imaging, subjective contrast-enhanced US and quantitative contrast-enhanced US in the estimation of Crohn disease activity in children by comparing it with histopathology as the reference standard.
Materials and methods
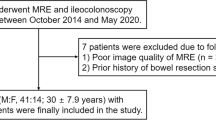
Forty-six children with clinical suspicion of exacerbated inflammatory bowel disease from January 2018 to February 2019 were included in this prospective study. All patients were referred to the abdominal US with colour Doppler imaging and endoscopy with histopathological evaluation as part of clinical care. The indications for endoscopy were: a) suspected clinical diagnosis of inflammatory bowel disease needing histological confirmation (n=32), b) assessment of the activity of Crohn disease during clinical relapse after an inactive phase (n=12) and c) assessment of the activity of Crohn disease during deterioration while on medical treatment (n=2). Additionally, as part of this research patients underwent contrast-enhanced US on the same day as endoscopy (n=28) or within 14 days (n=18) with no change in treatment during the interval. Contrast-enhanced US was performed on bowel segments with ≥4-mm thickened bowel wall on the US with colour Doppler imaging. If multiple diseased segments were identified, we used the two with the most thickened bowel wall. Biopsy specimens were taken from endoscopically normal mucosa or the site most inflamed at each segment along the colon and the terminal ileum. Specimens were sent to the histopathology laboratory and accompanied by crucial clinical information, macroscopic description of the mucosa and a schematic note of the location of the biopsy sample. After receiving biopsy results, patients with a histopathological diagnosis other than Crohn disease were excluded. A flow diagram of our study group is presented in Fig. 1.
The research was conducted following the Helsinki Declaration. The National Medical Ethics Committee approved the study. Patients’ parents and one 18-year old patient signed written informed consent after detailed explanation of the procedure.
Ultrasound with colour Doppler imaging
All US studies (US with colour Doppler imaging and the contrast-enhanced US) were performed by one of two experienced radiologists (D.K. and S.P.). The senior radiologist (D.K.) is skilled in paediatric US and contrast-enhanced US with 20 years of experience with intravesical and intravenous US contrast media administration (for bowel and other organ evaluation). The other radiologist has 10 years of experience in abdominal US and 4 years of experience in bowel contrast-enhanced US examination and analysis.
The US with colour Doppler imaging examinations were performed on an Aplio 500 machine (Canon Medical System Europe, Zoetermeer, the Netherlands), initially with a 3- to 6-MHz convex array transducer and then, for a detailed examination, with a 7.5- to 12-MHz linear transducer. Children were examined following overnight fasting. No special bowel preparation was needed. US with colour Doppler imaging of the intestine was performed by the standard technique as previously described by Biko et al. [10]. The following US data were obtained: location of the most affected bowel segments, bowel wall thickness, assessment of wall layer stratification and the presence of inflammatory fat. Additional observations (lymphadenopathy, free fluid) were also documented. Bowel wall vascularity was assessed with colour Doppler imaging. Images were only acquired if definitive pathology was seen.
Contrast-enhanced ultrasound
Contrast-enhanced US was performed with a 7.5- to 12-MHz linear transducer using contrast-specific software with a low mechanical index and a preset dedicated to the linear probe. The mechanical index was set at or below 0.8; the dynamic range was ≥65. The image was optimised concerning the position of the focus, gain, depth and observation area and remained unchanged during the contrast-enhanced US examination. The second-generation US contrast agent (SonoVue; Bracco, Milan, Italy) in a dose of 0.05 mL/kg was injected by bolus through one of the arm veins followed by a 10-mL saline flush. The subsequent enhancement was recorded as a continuous cine loop file for the 100-s interval immediately after injection. In cases with more than one diseased bowel segment, a second bolus was administered after at least 10 min. The raw native data were exported to the US workstation.
Image review
US with colour Doppler images and contrast-enhanced US studies were reviewed retrospectively independently by the radiologists mentioned above. Each of them was blinded to all clinical information and the results of other studies. The US studies with colour Doppler images were reviewed first and the contrast-enhanced US studies 4 weeks later in an attempt to reduce recall bias.
The estimation of Crohn disease activity with the US with colour Doppler imaging of the most diseased segments was based on the scoring system developed by Medellin-Kowalewski [11]. The inflammation was graded as no signs of inflammation/remission or mild, moderate or severe inflammation.
Contrast-enhanced US studies were reviewed on a US workstation using a proprietary software package (CHI Q, Canon [Toshiba], Tokyo, Japan). Contrast-enhanced US perfusion data are quantified by fitting a software-dedicated perfusion model (lognormal perfusion model with least-squares curve-fitting in our study) to a time-intensity curve extracted from a region of interest. Time-intensity curves were calculated using the intensity values of the pixels and the mean and median values of the image intensity [12]. Regions of interest were drawn manually (size approximately 1 cm2) at the most enhanced part of the bowel wall, excluding perivisceral tissue (Fig. 2). Since acquiring information from a single region of interest might introduce error from peristalsis or breathing, we used three non-overlapping regions of interest. Several parameters related to blood flow and volume were automatically computed by software by analysing the time-intensity curve (Fig. 2): peak enhancement, time to peak, mean transit time and area under the curve. Peak enhancement is defined as a maximum value of signal intensity and is reported in arbitrary units (AU) for linear values. Time to peak is expressed in seconds and defined as the time from zero to maximum signal intensity. Mean transit time is expressed in seconds and defined as the mean time taken by the bubbles to pass through the region of interest (mathematically it is the first moment of the fitted curve). The area under the curve is defined as the area under the time-intensity curve and reported in arbitrary units × seconds (AU×s) [13]. The mean value for each parameter from all three regions of interest was generated and used for further statistical analysis.
Contrast-enhanced US of the terminal ileum in a 16-year-old girl with Crohn disease. a Transverse contrast-enhanced US, dual-screen mode with simultaneous display of gray-scale image (right) and contrast-only image (left) shows intense transmural region of interest (blue oval). b Time-intensity curve automatically generated from the region of interest. X-axis represents time (s) and y-axis represents signal intensity (arbitrary units). Dots represent raw data and curve presents fitted lognormal perfusion model. The starting point of the time-intensity curve corresponds to the moment when the contrast media first appears in the region of interest. High peak intensity (19 arbitrary units) is consistent with severe inflammation
The subjective visual analysis included the assessment of different bowel wall perfusion patterns, as described by Migaleddu et al. [6]. Two types of graphic displays for viewing a time-intensity curve were attained: log and linear representations. Subjective grading included a visual analysis of the graphic representations of the log time-intensity curve, as defined: high peak enhancement and delayed decline at a higher enhancement level indicated severe disease; low peak enhancement with a rapid decline, more closely reaching the baseline, indicated mild disease [14].
Histopathological evaluation
An experienced histopathologist (R.D.G., with 25 years of experience) examined biopsy specimens. The degree of inflammation was evaluated according to the European Crohn and Colitis Organisation criteria as remission, mild, moderate and severe. Fibrosis was identified when abnormal depositions of collagen were seen in the edges of mucosal ulceration.
Due to the lack of validated histological scoring systems and data on outcomes, as well as concerns of sampling error, histological remission is not recommended as target treatment in Crohn disease. Instead, mucosal healing is defined as the treatment goal [15]. Given that persistent mild histopathological inflammation can be displayed in up to one-third of biopsies from patients with endoscopically healed mucosa [16], this most likely does not significantly affect clinicians’ decisions to treat or not to treat. Therefore, we decided to unite remission and mild grades of inflammation into an inactive disease group (i.e. indicating mucosal remission) and moderate and severe grades into an active disease group for dichotomisation of histopathological results.
Statistical analysis
The data for quantitative contrast-enhanced US kinetic parameters were, because of non-normality (Shapiro-Wilk W test), summarised as the median and interquartile range. The differences in the parameters between groups were tested with the Mann-Whitney U test. In multivariate logistic regression analysis, different models were formed to explore which of the kinetic parameters are most important for discriminating between the active and inactive groups. Odds ratios (OR) with 95% confidence intervals (CI) were reported. Models were evaluated with the Akaike information criterion and the Hosmer-Lemeshow test. With both tests, we assessed the fit of logistic regression models, whereby the Akaike information criterion also enabled us to compare different models. The smaller the Akaike information criterion, the better the model fits the data. However, the model with the smallest Akaike information criterion does not necessarily fit the data well, so we also used a goodness-of-fit test to assess the fit. In the case of logistic regression, the P-value of the Hosmer-Lemeshow test was checked and, if more than 0.05, provided evidence that predicted probabilities did not deviate from observed probabilities. Binned residual plots for each of the five models were also formed as the traditional residual plots of linear regression are not very helpful with logistic regression (Online Supplementary Material 1). Binned plots are not very informative in research with small sample size, so we relied instead on more global statistics (i.e. the Akaike information criterion and the Hosmer-Lemeshow test). A receiver operating characteristics curve analysis was applied to determine the threshold values of the kinetic parameters. Sensitivity, specificity and diagnostic accuracy were evaluated for the quantitative contrast-enhanced US, subjective contrast-enhanced US and US with colour Doppler imaging with 95% CI. The agreement between the two radiologists regarding their subjective contrast-enhanced US analysis was tested with kappa (κ) statistic. The values of κ were interpreted as follows: 0–0.20 indicated poor agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, good agreement; and 0.81–1.00, excellent agreement. A P-value of less than 0.05 was considered statistically significant. All analyses were performed using statistical software (SPSS version 25; IBM, Armonk, NY; and MedCalc version 19.0.6; MedCalc Software Ltd., Ostend, Belgium).
Results
Patient characteristics
Twenty-two patients were excluded from the study: 19 patients had a histopathological diagnosis other than Crohn disease (ulcerous colitis, n=7; indeterminate colitis, n=2; and infectious colitis, n=9) and 3 patients were excluded due to inadequate histopathological results. Twenty-four patients were eligible for contrast-enhanced US final analysis (age range: 3.5–18 years; median age: 14 years; interquartile range: 13–17 years; 12 boys, 12 girls). A total of 40 bowel segments were analysed: sigmoid colon, n=10; descending colon, n=6; transverse colon, n=1; ascending colon, n=3; cecum, n=7; and ileum, n=13. One bowel segment was analysed in 8 patients and 2 bowel segments in 16 patients. Patient and segment characteristics are summarised in Table 1.
Only one transient adverse event occurred during contrast-enhanced US examination: a strong metallic taste that vanished after 10 min.
Histopathology
Histopathological examination identified remission in 10 segments (25%), mild inflammation in 12 segments (30%), moderate inflammation in 17 (42.5%) segments and severe inflammation in 1 (2.5%) segment. In agreement with our dichotomisation, 22 of 40 segments (55%) were classified as inactive disease and 18 of 40 segments (45%) as active disease group.
Ultrasound with colour Doppler imaging
The sensitivity, specificity and accuracy of US with colour Doppler imaging analysis were 55.6%, 86.4% and 72.5%, respectively. Seven falsely negative and three falsely positive results occurred (Table 2).
Subjective contrast-enhanced US
The sensitivity, specificity and accuracy of subjective contrast-enhanced US were 77.8%, 77.3% and 77.5%, respectively. Four segments were falsely evaluated as negative and five segments as falsely positive (Table 2). Interobserver agreement between the two radiologists for subjective contrast-enhanced US analysis was good (κ=0.74, 95% CI 0.58–0.90).
Quantitative contrast-enhanced US
Univariate analysis of quantitative contrast-enhanced US parameters showed a significant difference between the inactive and active groups concerning peak enhancement, mean transit time and area under the curve (P<0.001, P=0.015 and P=0.001) (Table 3). Since the time-to-peak parameter was not significant (P=0.103), it was excluded from further analyses. Multivariate logistic regression analyses revealed that the most predictive was the model with peak enhancement only, regardless of the models with mean transit time and/or area under the curve included. All fitted models showed no misfit (Hosmer-Lemeshow test, P>0.05), but according to the Akaike information criterion, the model with only peak enhancement performed better than all the other models (the lowest Akaike information criterion) (Table 4). The patients with higher peak enhancement were more likely to have active inflammation than the patients with lower peak enhancement (OR=1.44, 95% CI 1.11–1.87, P=0.007). A receiver operating characteristics curve for the peak enhancement parameter showed sensitivity 72.2%, specificity 100% and overall diagnostic accuracy 87.5% (Fig. 3). According to peak enhancement at a threshold value of 6.9, there were five false negatives and no false positives in our sample (Table 2) (Fig. 4). The proportions of disagreement (as extracted from Table 2) are 12.5% for peak enhancement, 22.5% for mean transit time, 20% for the area under curve, 22.5% for subjective contrast-enhanced US analysis and 24.5% for the US with colour Doppler imaging, respectively. Detailed bowel segment results, as evaluated by histopathology, US with colour Doppler imaging, subjective and quantitative contrast-enhanced US (peak enhancement parameter) are presented in Online Supplementary Material 2.
A scatterplot of peak enhancement versus four grades of inflammation at histopathology (0–remission, 1–mild, 2– moderate, 3–severe). The threshold value (horizontal line) for peak enhancement is set at 6.9, differentiating mucosal remission (histopathology grades 0 and 1) from active inflammation (histopathology grades 2 and 3). Mucosal remission was falsely estimated in five segments
Discussion
The European Federation of Societies for Ultrasound in Medicine and Biology states that contrast-enhanced US can be used as an alternative imaging modality for the follow-up of children with known inflammatory bowel disease [7]. However, the level of evidence is based on adult studies. Furthermore, a lack of consensus regarding contrast-enhanced US parameters for the diagnosis of active Crohn disease and software packages offering a variety of perfusion measures make translating results between different machines and vendors problematic.
The results of our study revealed that quantitative contrast-enhanced US, particularly the peak enhancement parameter, had the highest performance in detecting the inflammatory activity of Crohn disease in children. The peak enhancement parameter at a threshold value of 6.9 (specific to our quantification program and cannot be used as general cutoff value when other quantification programs are used) showed 72.2% sensitivity, 100% specificity and 87.5% overall diagnostic accuracy. Lower sensitivity in our study is not in line with the results of two previous studies in adults, which reported sensitivity of peak enhancement of 89.4% [17] and 93% [18]. This could be associated with patient characteristics in their studies. Romanini et al. [17] included 33 patients with inflammatory bowel disease, of which only 15 patients had Crohn disease. On the other hand, Ripollés et al. [18] included patients with Crohn disease who were candidates for resection. Of the 40 bowel wall segments in our study, 5 segments (4 of 24 children) were falsely considered to have negative results with peak enhancement below the cutoff value. In one case, this can be attributed to a mismatch of the segment selection on contrast-enhanced US and histopathology. In the remaining four segments, fibrosis might have contributed to falsely lowered peak enhancement values. All of these segments were falsely negative also by subjective contrast-enhanced US and US with colour Doppler imaging and demonstrated a mixed pattern of moderate fibrosis and moderate acute inflammation on histopathology. Similar observations were noted in studies in adults [18, 19]. Furthermore, fibrosis reduces blood volume and blood flow [20], which might have contributed as well.
On the contrary, Wilkens et al. [21] recently demonstrated that relative contrast enhancement could not distinguish between inflammatory activity and fibrosis. This was also noted in an animal model of Crohn disease [22]. Thimm et al. [23] used US elastography on three patients to complement the contrast-enhanced US and detect bowel wall fibrosis through evaluation of tissue stiffness, as previously suggested by Quaia et al. [24].
The time-to-peak parameter did not show any significant difference between active and inactive Crohn disease. This is not in line with the results of previous studies, where time to peak was found to be significantly lower in adults with active Crohn disease [17, 25, 26] and attributed to inflammatory oedema. Other studies [28,27,29], however, reported contradictory results of time to peak and raised incongruous discussions on the relevance of this parameter.
Subjective contrast-enhanced US analysis of the bowel wall enhancement pattern in conjunction with the graphic representation of the log time-intensity curve was superior to US with colour Doppler imaging. Sensitivity, specificity and accuracy for the subjective contrast-enhanced US were 77.8%, 77.3% and 77.5%, and 55.6%, 86.4% and 72.5% for US with colour Doppler imaging analysis, respectively. Migaleddu et al. [6] reported a much better performance of subjective contrast-enhanced US (93.5% sensitivity, 93.7% specificity, 93.6% diagnostic accuracy). This difference can be attributed to the interobserver variability, examinators’ experience and rapid microbubble inflow that does not provide a wide temporal window for an unequivocal evaluation of each enhancement pattern. Furthermore, transmural contrast enhancement pattern has been described in patients with inflammatory as well as fibrotic strictures of the small bowel [19].
Although our sample size was comparable to other studies investigating the same modality in adults, a rather small number of children and bowel segments is a limitation of our study, and was also the reason that only the dichotomous cutoff value for disease activity was provided. The histopathological heterogeneity of the disease activity, presenting in a spectrum from acute inflammation to long-standing fibrosis, is a significant limitation with the impact on our results mentioned above. Incorrect bowel segment classification due to inherent US limitation and a lack of a validated histopathology scoring system are other biases.
Overall, quantitative contrast-enhanced US’s peak enhancement is predictive of active Crohn disease in children with comparable diagnostic accuracy as in adults. Intravenous application of US contrast agent in children is currently off-label in Europe and approved only for evaluation of liver lesions in the United States of America [30]. Intravascular US contrast media use in children is associated with a very low rate of severe adverse reactions (less than 1/10,000 patients; 0.009%) [31]. In our study, one mild adverse event was noted (transient metallic taste). However, any exposure to intravascular US contrast media, with or without previous sensitisation, may result in anaphylaxis [32, 33]. Therefore, precautions should be in place with every contrast-enhanced US examination and examinations should be performed only by adequately trained medical personnel [33]. Albeit a child-friendly method, it may cause distress for the child as cannulation is needed. It does not, however, exceed the discomfort of respective alternative techniques (endoscopy and MR enterography). Besides, US contrast media can be safely administered to patients with renal insufficiency with no risk of contrast-related nephropathy or nephrogenic systemic fibrosis [34]. Hazards associated with sedation or anaesthesia needed in endoscopy and MR enterography are also avoided.
Mucosal healing, rather than symptom control or histological remission, is increasingly recommended as the optimal treatment target of Crohn disease. To evaluate disease activity, the Pediatric Crohn Disease Activity Index and faecal calprotectin are often used. However, the former can be subjective and cumbersome to calculate, and the latter can be present in intestinal infections and as such is not a specific indicator of inflammation. Evaluation of bowel wall thickness with the US with colour Doppler imaging cannot reliably distinguish between active inflammation and quiescent disease and fails to demonstrate blood flow at the capillary level. On the contrary, contrast-enhanced US displays hyperemia and neovascularisation also at perfusion level and, as demonstrated in our study, peak enhancement cut-off value provides objective evaluation of bowel wall enhancement. In our everyday clinical experience, quantitative contrast-enhanced US has shown to be a convenient, complementary method to clinical and laboratory evaluation of Crohn disease activity in children. It is useful particularly in patient follow-up where peak enhancement dynamics from baseline to following controls can be monitored and objective response to treatment noticed. As baseline contrast-enhanced US examination is usually accompanied by histopathological bowel wall evaluation, information regarding fibrosis and its possible impact on peak enhancement value is somewhat provided. In a considerable number of our patients, contrast-enhanced US also reduced the need for more invasive investigations, particularly in children with small bowel disease who refused MR enterography. In some patients, it was also possible to postpone endoscopic evaluation of disease activity.
Conclusion
Quantitative contrast-enhanced US has the potential to become a complementary method in the evaluation of Crohn disease activity in children. In particular, peak enhancement is predictive of active inflammation. Fibrosis may affect peak enhancement results and underestimate inflammatory activity. Hereof, the introduction of US elastography for assessment of fibrosis could be useful. Subjective contrast-enhanced US analysis shows a slightly better diagnostic accuracy than the US with colour Doppler imaging.
References
Schreiber-Dietrich D, Chiorean L, Cui XW et al (2015) Particularities of Crohn's disease in pediatric patients: current status and perspectives regarding imaging modalities. Expert Rev Gastroenterol Hepatol 9:1313–1325
Esteban JM, Maldonado L, Sanchiz V et al (2001) Activity of Crohn's disease assessed by colour Doppler ultrasound analysis of the affected loops. Eur Radiol 11:1423–1428
Horsthuis K, Bipat S, Bennink RJ, Stoker J (2008) Inflammatory bowel disease diagnosed with the US, MR, scintigraphy, and CT: a meta-analysis of prospective studies. Radiology 247:64–79
Sauer CG, Middleton JP, Alazraki A et al (2012) Comparison of magnetic resonance enterography with endoscopy, histopathology, and laboratory evaluation in pediatric Crohn disease. J Pediatr Gastroenterol Nutr 55:178–184
Ripollés T, Martínez-Pérez MJ, Blanc E et al (2011) Contrast-enhanced ultrasound (CEUS) in Crohn's disease: technique, image interpretation, and clinical applications. Insights Imaging 2:639–652
Migaleddu V, Scanu AM, Quaia E et al (2009) Contrast-enhanced ultrasonographic evaluation of inflammatory activity in Crohn's disease. Gastroenterology 137:43–52
Sidhu PS, Cantisani V, Deganello A et al (2017) Role of Contrast-Enhanced Ultrasound (CEUS) in Paediatric Practice: An EFSUMB Position Statement. Ultraschall Med 38:33–43
Kljucevsek D, Vidmar D, Urlep D, Dežman R (2016) Dynamic contrast-enhanced ultrasound of the bowel wall with quantitative assessment of Crohn's disease activity in childhood. Radiol Oncol 50:347–354
Tang MX, Mulvana H, Gauthier T et al (2011) Quantitative contrast-enhanced ultrasound imaging: A review of sources of variability. Interface Focus 1:520–539
Biko DM, Rosenbaum DG, Anupindi SA (2015) Ultrasound features of pediatric Crohn disease: a guide for case interpretation. Pediatr Radiol 45:1557–1566
Medellin-Kowalewski A, Wilkens R, Wilson A et al (2016) Quantitative contrast-enhanced ultrasound parameters in Crohn's disease: their role in disease activity determination with ultrasound. Am J Roentgenol 206:64–73
Akhbardeh A, Sagreiya H, Kaffas AE et al (2019) A Multi-Model Framework to Estimate Perfusion Parameters Using Contrast-Enhanced Ultrasound Imaging. Med Phys 46:590–600
Dietrich CF, Averkiou MA, Correas JM et al (2012) An EFSUMB Introduction into dynamic contrast-enhanced ultrasound (DCE-US) for quantification of tumor-perfusion. Ultraschall Med 33:344–351
Medellin A, Merrill C, Wilson SR (2018) Role of contrast-enhanced ultrasound in the evaluation of the bowel. Abdom Radiol (NY) 43:918–933
Agrawal M, Colombel JF (2019) Treat-to-Target in Inflammatory Bowel Diseases, What Is the Target and How Do We Treat? Gastrointest Endosc Clin N Am 29:421–436
Gong W, Guo K, Zheng T et al (2019) Correlation between endoscopic and histological validated scoring indices in Crohn's disease. Dig Liver Dis 51:812–817
Romanini L, Passamonti M, Navarria M et al (2014) Quantitative analysis of contrast-enhanced ultrasonography of the bowel wall can predict disease activity in inflammatory bowel disease. Eur J Radiol 83:1317–1323
Ripolle's T, Rausell N, Paredes JM et al (2013) Effectiveness of contrast-enhanced ultrasound for characterisation of intestinal inflammation in Crohn's disease: a comparison with surgical histopathology analysis. J Crohns Colitis 7:120–128
Quaia E, De Paoli L, Stock T et al (2012) The value of small bowel wall contrast enhancement after sulfur hexafluoride filled microbubble injection to differentiate inflammatory from fibrotic strictures in patients with Crohn's disease. Ultrasound Med Biol 38:1324–1332
Nylund K, Jirik R, Mezl M et al (2013) Quantitative contrast-enhanced ultrasound comparison between inflammatory and fibrotic lesions in patients with Crohn's disease. Ultrasound Med Biol 39:1197–1206
Wilkens R, Hagemann-Madsen RH, Peters DA et al (2018) Validity of contrast-enhanced ultrasonography and dynamic contrast-enhanced MR enterography in the assessment of transmural activity and fibrosis in Crohn's disease. J Crohns Colitis 12:48–56
Dillman JR, Rubin JM, Johanson LA et al (2017) Can contrast-enhanced sonography detect bowel wall fibrosis in mixed inflammatory and fibrotic Crohn disease lesions in an animal model? J Ultrasound Med 36:523–530
Thimm MA, Cuffari C, Garcia A et al (2019) Contrast-Enhanced Ultrasound and Shear Wave Elastography Evaluation of Crohn's disease Activity in Three Adolescent Patients. Pediatr Gastroenterol Hepatol Nutr 22:282–290
Quaia E, Gennari AG, Cova MA, van Beek EJ (2018) Differentiation of inflammatory from fibrotic ileal strictures among patients with Crohn's disease based on visual analysis: feasibility study combining conventional B-mode ultrasound, contrast-enhanced ultrasound and strain elastography. Ultrasound Med Biol 44:762–770
Girlich C, Schacherer D, Jung EM et al (2012) Comparison between a clinical activity index (Harvey-Bradshaw-Index), laboratory inflammation markers and quantitative assessment of bowel wall vascularisation by contrast-enhanced ultrasound in Crohn's disease. Eur J Radiol 81:1105–1109
De Franco A, Di Veronica A, Armuzzi A et al (2012) Ileal Crohn disease: mural microvascularity quantified with the contrast-enhanced US correlates with disease activity. Radiology 262:680–688
Quaia E, Migaleddu V, Baratella E et al (2009) The diagnostic value of small bowel wall vascularity after sulfur hexafluoride filled microbubble injection in patients with Crohn's disease. Correlation with the therapeutic effectiveness of specific anti-inflammatory treatment. Eur J Radiol 69:438–444
Quaia E, Sozzi M, Angileri R et al (2016) Time-Intensity Curves Obtained after Microbubble Injection Can Be Used to Differentiate Responders from Nonresponders among Patients with Clinically Active Crohn Disease after 6 Weeks of Pharmacologic Treatment. Radiology 281:606–616
Saevik F, Nylund K, Hausken T et al (2014) Bowel perfusion measured with dynamic contrast-enhanced ultrasound predicts treatment outcome in patients with Crohn's disease. Inflamm Bowel Dis 20:2029–2037
Ntoulia A, Anupindi SA, Darge K, Back SJ (2018) Applications of contrast-enhanced ultrasound in the pediatric abdomen. Abdom Radiol (NY) 43:948–959
Piskunowicz M, Kosiak W, Batko T et al (2015) Safety of intravenous application of second-generation ultrasound contrast agent in children: a prospective analysis. Ultrasound Med Biol 41:1095–1099
Knieling F, Strobel D, Rompel O et al (2016) Spectrum, applicability and diagnostic capacity of contrast-enhanced ultrasound in pediatric patients and young adults after intravenous application—a retrospective trial. Ultraschall Med 37:619–626
Coudray S, Fabre C, Aichoun I, Perez-Martin A (2017) Anaphylactic shock with an ultrasound contrast agent. J Med Vasc 42:384–387
Sidhu PS, Cantisani V, Dietrich CF et al (2018) The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med 39:e2–e44
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Online Supplementary Material 1
Binned residual plots for five logistic regression models. (PNG 1384 kb) Data (n=40) were divided into five classes, and within each, the average residual between observed and predicted value was calculated. The grey lines represent ±2 standard deviation bands, which we would expect to contain about 95% of the observations. For all five models, the points lie within limits, so we conclude that all the models look acceptable
Online Supplementary Material 2
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Ponorac, S., Gošnak, R.D., Urlep, D. et al. Contrast-enhanced ultrasonography in the evaluation of Crohn disease activity in children: comparison with histopathology. Pediatr Radiol 51, 410–418 (2021). https://doi.org/10.1007/s00247-020-04870-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-020-04870-3