Abstract
Background
Low b-value (50–100 s/mm2) diffusion-weighted images (low b-value DWI) have been shown to be superior to T2-weighted fast spin echo sequence (T2-W) in detecting liver lesions in adults. There are no such studies assessing this difference in children.
Objective
The purpose of the study was to compare the sensitivity of low b-value DWI images and T2-W images in detecting focal liver lesions in children.
Materials and methods
A retrospective review of liver magnetic resonance imaging (MRI) to assess focal liver lesions in 50 children (22 males, 28 females; age: 2 months to 17 years [mean: 10.9 years]) was performed. Two radiologists reviewed both low b-value DWI and T2-W sequences independently on different occasions to note lesions, the smallest lesion size and the location. A consensus reading of the entire MRI examination and a correlation with follow-up, other imaging modalities and pathology in available cases were used to determine the final number of lesions as a reference standard. The average number of lesions per patient detected by both readers on each sequence was compared with each other and with the reference standard using the signed-rank test. The smallest lesions detected by each sequence were compared using the paired t-test.
Results
One hundred seventy hyperintense lesions were identified on consensus review to serve as the reference standard. The average number of lesions identified by both readers on low b-value DWI was 134 (79%) and on T2-W was 95 (56%). There was excellent interobserver agreement for detection of lesions on low b-value DWI (intraclass correlation coefficient [ICC]=0.96 [0.93–0.98]) and T2-W (ICC=0.85 [0.75–0.91]), with slightly better agreement on low b-value DWI. Both readers identified significantly more number of lesions on low b-value DWI compared to T2-W (Reader 1: P=0.0036, Reader 2: P=0.0001). Compared to the reference standard (mean number of lesions: 3.45), T2-W detected significantly fewer lesions (mean number of lesions: 1.91; P=0.0001) while there was no significant difference in lesion detection on low b-value DWI (mean number of lesions: 2.68; P=0.1527). Low b-value DWI and T2-W were not significantly different in identifying the smallest lesion size (Reader 1: P=0.19, Reader 2: P=0.47).
Conclusion
Low b-value DWI images are more sensitive than T2-W sequences in detecting hyperintense focal liver lesions in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diffusion-weighted imaging (DWI) is a useful technique in pediatric body imaging that can be used for lesion detection, characterization and therapy response assessment [1]. Acquiring DWI involves applying diffusion gradients to T2-weighted (T2-W) images to make them sensitive to water molecule mobility or diffusion. The degree of diffusion weighting is indicated by a b-value. As b-value increases, sensitivity of the sequence to the diffusion increases, and overall signal from water molecules and signal-to-noise ratio decrease. At high b-value, those tissues with restricted diffusion, those with long T2 relaxation or both will only retain signal. Applying lower diffusion gradient, typically b-values of 50–100 s/mm2, eliminates signal from all the vessels with little reduction in signal-to-noise ratio thereby improving conspicuity of T2-hyperintense lesions on these images. Most hepatic lesions display hyperintense signal on T2-W images [2] and retain hyperintense signal on low b-value images that are basically T2-W images with a small diffusion gradient applied [3]. In a few adult studies [3,4,5,6,7,8], low b-value images have been shown to be superior in detecting liver lesions than routine T2-W images. There are no such studies assessing the detection of pediatric hepatic lesions. Use of low b-value images for hepatic lesion detection can complement T2-W images.
The purpose of this study was to compare low b-value diffusion images with T2-W fast spin echo images in detecting focal liver lesions in children.
Materials and methods
Institutional Research Ethics Board approval and a waiver for individual patient consent were granted for this retrospective study.
Patients
The institutional database of radiology reports was retrospectively searched for patients with focal liver lesions who had MR examinations between January 2009 and April 2013. A patient list was prepared by a research associate (H.G.) using the keywords “abdominal MRI” or “liver MRI” and “liver lesion” or “liver mass.” A sample of 50 patients was selected from the institutional picture archiving communication system (PACS; GE Healthcare, Milwaukee, WI), fulfilling the following inclusion criteria: (1) magnetic resonance imaging (MRI) performed for suspicion or evaluation of known focal liver lesions; (2) complete liver MRI protocol including T2-W and DWI images, and (3) reports without mention of limited diagnostic quality or artifactual degradation of images. MRI examinations without DWI or T2-W images or with mention of severe artifact degradation limiting the exam quality in the report were excluded.
MRI technique
MR examinations were performed either on 1.5-T Siemens (Avanto; Siemens Medical System, Erlangen, Germany) or 1.5-T and 3-T Philips (Achieva; Philips Medical System, Best, The Netherlands) scanners. A standardized institution protocol was followed on all three scanners for liver MRI examinations. Included sequences were: coronal single-shot T2-W or STIR (short tau inversion recovery), axial T1-W gradient echo sequence with in- and out-of-phase, axial T2-W fast spin echo with respiratory triggering, axial balanced SSFP (steady state free precession) (TrueFISP [true fast imaging with steady-state precession]/bTFE [balanced turbo field echo]), DWI, and pre-contrast and post-contrast dynamic axial T1-W 3-D gradient echo sequence (VIBE [volumetric interpolated breath-hold examination] [Siemens]/THRIVE [T1-W high-resolution isotropic volume examination] [Philips]). Axial T1-W fast spin echo with fat saturation 5 min after contrast injection was also done. The parameters of all the sequences are summarized in Table 1.
DWI on the Siemens unit was performed with b-values=50, 400, 800 s/mm2, while the Philips units had DWI with b-values=0, 100, 600 s/mm2. This sequence was respiratory triggered in all children and took approximately 4.5 min to acquire. All b-value images and automated monoexponential apparent diffusion coefficient (ADC) maps generated on the scanner were sent to PACS.
Image analysis
Two radiologists independently reviewed the MR examinations (Reader 1=E.S., 2 years of experience, and Reader 2=G.B.C., 10 years of experience). Initially, both readers independently reviewed the low b-value (b-value=50 s/mm2 or 100 s/mm2) DWI (low b-value DWI) sequence and axial T2-W fast spin echo sequence on separate occasions. An interval of at least 4 weeks was kept between the evaluation of the low b-value DWI and T2-W by each reader to minimize recall bias. They noted the number of liver lesions, the smallest lesion size and the location in the liver. The lesion number up to 10 was noted and in cases with more than 10 lesions, the number of lesions was noted as 11. Only T2 hyperintense lesions were evaluated in this study. The presence of any T2 hypointense lesion on T2-W was noted and not included in the analysis. The readers also noted any significant artifact on DWI not limiting the overall diagnostic quality. Both readers were blinded to clinical and laboratory information, diagnosis and indication for the examination during the initial review.
After completing the initial independent review of two sequences, both readers then reviewed entire MRI examinations together in consensus to determine the final number of lesions, background liver and final diagnosis of liver lesions. During this review, correlation with follow-up, other imaging modalities, clinical features and pathology in available cases was made. The final number of lesions for each patient determined during this review served as the reference standard against which the number of lesion detected by low b-value DWI and T2-W sequences was compared.
Statistical analysis
Interobserver agreement between the two readers on the number of lesions detected on low b-value DWI and T2-W sequences was assessed using intra-class correlation coefficient (ICC). The number of lesions per patient detected by each reader on two sequences was compared using the signed-rank test. The average number of lesions by the two readers per patient on each sequence was compared with the reference standard using the signed-rank test. The smallest lesions detected on each sequence by each reader were compared using the paired t-test. In all analyses, P-values<0.05 were considered statistically significant.
Results
Fifty children (22 males, 28 females; ages: 2 months to 17 years [mean: 10.9 years]) were included. Of the 50 MRI examinations, 21 (42%) had DWI performed with b-value=50 mm/s2 and 29 (58%) with b-value=100 mm/s2. Four MRI examinations (8%) were performed without intravenous gadolinium administration.
At least one focal lesion was seen in 39/50 children with no focal lesions in the remaining 11/50. The diagnoses of lesions are summarized in Table 2. The presence of hypointense lesions was noted on T2-W in only 4/50 children; some of these lesions were also well seen on low b-value DWI images. Background liver parenchyma was normal on imaging in 34/50 children, cirrhotic in 13/50, fatty in 2/50 and siderotic in 1/50. Significant artifacts of DWI that didn’t limit diagnostic ability, including distortion, wrapping and movement artifacts, were seen in 5/50 children. However, the images were deemed of enough quality to assess the presence of focal lesions.
Interobserver agreement
There was excellent interobserver agreement for detection of lesions on both low b-value DWI (ICC=0.96 [0.93–0.98]) and T2-W (ICC=0.85 [0.75–0.91]), with slightly better agreement on low b-value DWI.
Analysis of total number of lesions in the cohort
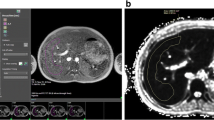
One hundred seventy focal liver lesions were identified on consensus review and served as reference standard. On independent review of the low b-value DWI images, Reader 1 detected 140 lesions while Reader 2 detected 128. On independent review of the T2-W images, Reader 1 detected 108 lesions while Reader 2 detected 82. The average number of lesions identified by both readers on low b-value DWI was 134/170 (79%) and on T2-W was 95/170 (56%) (Figs. 1 and 2). At least one lesion was detected in five patients by Reader 1 and in eight patients by Reader 2 in cases where T2-W did not show any lesion.
Focal nodular hyperplasia in an 8-year-old girl with a past history of atypical teratoid rhabdoid tumor. Axial T2-W fast spin-echo image (a) shows multiple faintly hyperintense lesions (arrows). Low b-value (b=100 s/mm2) image (b) demonstrates these lesions (arrows) with more superior conspicuity and also demonstrates some additional lesions. Post-contrast T1-W THRIVE (T1-W high-resolution isotropic volume examination) image (c) in late arterial phase demonstrates avid enhancement of these lesions (arrows)
Focal nodular hyperplasia in a 15-year-old girl with a history of lymphoma. Axial T2-W fast spin echo image (a) does not show any distinct lesion in the expected location (arrow). Low b-value (b=50 s/mm2) image (b) demonstrates a faint lesion (arrow). Post-contrast T1-W VIBE (volumetric interpolated breath-hold examination) image (c) in the arterial phase demonstrates avid enhancement of the lesion (arrow). Hepatobiliary phase image (d) at 45 min after injection of gadobenate does not demonstrate any lesion in the expected location (arrow) suggesting isointensity with parenchyma and uptake in the lesion in keeping with focal nodular hyperplasia
Per-patient analysis
On a per-patient comparison of the two sequences with each other, both readers identified significantly more lesions on low b-value DWI compared to T2-W (Table 3). The mean numbers of lesions per patient detected on each sequence were averaged for the two readers and compared to the mean number of lesions by reference standard. Compared to the reference standard (mean number of lesions: 3.45), T2-W detected significantly fewer lesions (mean number of lesions: 1.91; P<0.0001) while there was no significant difference in lesion detection on low b-value DWI (mean number of lesions: 2.68; P=0.15).
Comparison of smallest lesion
The average smallest lesion detected by Reader 1 on T2-W in 33/50 children was 14.6 mm (range: 2–84 mm) and on low b-value DWI in 36/50 children was 11.4 mm (range: 2–39 mm). This difference was not statistically significant (P=0.19) by paired t-test. The average smallest lesion detected by Reader 2 on T2-W in 27/50 children was 15.1 mm (range: 2–73 mm) and on low b-value DWI was in 36/50 children was 14.9 mm (range: 2–70 mm). This difference was not statistically significant (P=0.47) by paired t-test. Low b-value DWI and T2-W were also not significantly different in identifying lesions 1 cm or smaller (Reader 1: P=0.44, Reader 2: P=0.47).
Discussion
Our study in a pediatric population confirms previously reported observation in adult studies that low b-value DWI images are more superior in detecting focal liver lesions than T2-W images [3, 5,6,7,8]. The superiority of low b-value DWI to detect lesions as compared to the T2-W sequence was seen in analysis done three different ways including overall cohort comparison, per-patient comparison and a comparison with the reference standard. There was excellent interobserver agreement for both sequences, but it was better for low b-value DWI. Better contrast-to-noise ratio and improved lesion conspicuity by suppression of background vessels improves liver lesion detection on low b-value DWI images. Improved contrast-to-noise ratio can make the lesion on low b-value DWI slightly hyperintense while the lesion is perceived as isointense on T2-W (Fig. 1). A fairly large isointense lesion can be potentially missed on T2-W images. DWI images are less sensitive to motion artifacts as compared to T2-W images. This might also contribute to better lesion detection on low b-value DWI images. While low b-value DWI images in the range of b-value=50–100 s/mm2 are useful in lesion detection, higher b-value images are not. Signal-to-noise ratio is significantly reduced with higher b-values and those lesions without sufficiently longer T2 relaxation time would not have enough signals at high b-value images to be detected on them. Hence, low b-value DWI images should be used for lesion detection and high b-value images for lesion characterization.
Reference standard consensus review detected more lesions than both low b-value DWI and T2-W images because of the combination of all available sequences in the whole exam. In this regard, arterial phase images contributed most significantly as some lesions such as some focal nodular hyperplasia and arterially enhancing lesions of Fontan can only be seen on arterial phase images. Though rare, certain liver lesions such as regenerative nodules can be hypointense on T2-W images [9]. These hypointense lesions may not be detected on low b-value DWI images because of reduced signal-to-noise ratio as compared to T2-W. Hence, we did not include these lesions in our analysis, which was only focused on detecting T2 hyperintense lesions. Hypointense lesions were seen in four patients in our study and some of them were also well seen on low b-value DWI images (Fig. 3). Of 5 patients with 46 regenerative nodules on standard of reference included in the analysis, 3 patients had >10 regenerative nodules and the remaining 2 patients had 6 and 8 regenerative nodules. Of 46 regenerative nodules by reference standard, only 7 and 11 were detected on T2-W images and only 18 and 15 were detected on low b-value DWI images by Reader 1 and Reader 2, respectively. This minority of regenerative nodules detected on low b-value DWI and T2-W were slightly hyperintense. Also take into consideration that 3 patients had >10 regenerative nodules that could be 20, 30 or even 50. Hence, the majority of regenerative nodules in these five patients were still hypointense. A greater number of regenerative nodules is detected on the reference standard because of the combination of multiple sequences and especially arterial phase images where they can be slightly hyperintense
Regenerative nodules in a 13-year-old boy with biliary atresia and cirrhosis. Axial T2-W fast spin echo image (a) shows a hypointense lesion (arrow). Low b-value (b=100 s/mm2) image (b) demonstrates the lesion with better conspicuity (arrow). On pre-contrast T1-W THRIVE (T1-W high-resolution isotropic volume examination) image (c) the lesion (arrow) is hyperintense. On post-contrast T1-W THRIVE image in the late arterial phase (d) the lesion (arrow) remains slightly hyperintense. Hepatobiliary phase image (e) at 45 min after injection of gadobenate demonstrates slight hyperintensity of the lesion (arrow). MRI features are in keeping with a regenerative nodule
Most of the adult studies have evaluated detection of predominantly malignant lesions and, in particular, liver metastases [3, 6, 8]. Our cohort consisted of predominantly benign lesions (Table 1). The study by Yang et al. [7] demonstrated that low b-value DWI detects significantly more malignant lesions as compared to T2-W, but there was no significant difference in detection of benign lesions that mainly consisted of hemangiomas and cysts. This finding, however, was not seen in a study by Parikh et al. [3], in which low b-value DWI detected significantly more malignant as well as benign lesions. This was likely related to the wide range of different benign lesions in their cohort. Some adult studies have demonstrated that the superiority of lesion detection on low b-value DWI images is even more pronounced for small lesions <1 cm [5, 6]. We also compared the detectability of the smallest lesion in each patient in our cohort. However, there was no significant difference in the smallest lesion detected on each sequence. A separate analysis for lesions <1 cm also did not demonstrate any difference between low b-value DWI and T2-W. The reason for this difference with adult experience is not clear to us and our analysis is limited by a small sample size of the smallest lesions. More lesions were detected by low b-value DWI than T2-W with all the diagnoses in cohort. Because of the small sample size for each diagnosis it was difficult to draw conclusive differences amongst them.
For DWI in body imaging, a single-shot fast spin echo echoplanar sequence is the most commonly used sequence [10]. It can be acquired with breath-hold, free breathing or respiratory triggering. In children, it is most commonly acquired with respiratory triggering and provides better signal-to-noise ratio and the ability to use more number of b-values than the other two methods. It takes about 4–5 min for DWI with three b-values. Having a low b-value of about 50–100 s/mm2 in DWI is beneficial in two ways -- it helps to detect lesions better than T2-W and the greater the number of b-values the more accurate the ADC value. A single DWI sequence with a combination of low b-value (b=50–100 s/mm2) for lesion detection and higher (b=600–800 s/mm2) for lesion characterization can potentially replace T2-W, at least in one plane, and save the table time. However, a cautious approach needs to be taken for T2 hypointense lesions, which can be potentially missed on low b-value DWI images. If T2-W is done in two planes, one plane can be replaced with low b-value DWI images. Also, DWI is an artifact-prone sequence and can be affected by distortion, wrapping and susceptibility artifacts as seen in five of our cases. Ensuring optimal technique is important.
Our results need to be interpreted in light of a few limitations. It is a retrospective study. Many of the liver lesions may only be seen on post-contrast images, especially arterial phase, and four of our patients did not have post-contrast imaging, hence our reference standard is not absolute. However, the superiority of low b-value DWI over T2-W is obvious when these two sequences are compared with each other. Our study included 2 types of low b-value DWI images, 50 or 100 s/mm2. While this remains a slight limitation as, theoretically, signal-to-noise ratio will be further reduced on low b-value DWI with 100 s/mm2 as compared to 50 s/mm2, the lesion detectability may not be affected significantly as both are still in the low range. T2 hypointense lesions were not included in the analysis. However, the majority of lesions in the clinical practice are T2 hyperintense and it is our clinical experience that hypointense lesions can be potentially missed on low b-value DWI. Hence, our focus of analysis was the detectability of T2 hyperintense liver lesions.
Conclusion
Low b-value DWI images are more sensitive than T2-W sequences in detecting hyperintense focal liver lesions in children. They can complement T2-W sequences in the liver imaging protocol for lesion detection.
References
Chavhan GB, Alsabban Z, Babyn PS (2014) Diffusion-weighted imaging in pediatric body MR imaging: principles, technique, and emerging applications. Radiographics 34:E73–E88
Alqatie A, Mann E, Moineddin R et al (2015) Solitary liver lesions in children: interobserver agreement and accuracy of MRI diagnosis. Clin Imaging 39:442–448
Parikh T, Drew SJ, Lee VS et al (2008) Focal liver lesion detection and characterization with diffusion-weighted MR imaging: comparison with standard breath-hold T2-weighted imaging. Radiology 246:812–822
Soyer P, Boudiaf M, Placé V et al (2011) Preoperative detection of hepatic metastases: comparison of diffusion-weighted, T2-weighted fast spin echo and gadolinium-enhanced MR imaging using surgical and histopathologic findings as standard of reference. Eur J Radiol 80:245–252
Zech CJ, Herrmann KA, Dietrich O et al (2008) Black-blood diffusion-weighted EPI acquisition of the liver with parallel imaging: comparison with a standard T2-weighted sequence for detection of focal liver lesions. Investig Radiol 43:261–266
Bruegel M, Gaa J, Waldt S et al (2008) Diagnosis of hepatic metastasis: comparison of respiration-triggered diffusion-weighted echo-planar MRI and five t2-weighted turbo spin-echo sequences. AJR Am J Roentgenol 191:1421–1429
Yang DM, Jahng GH, Kim HC et al (2011) The detection and discrimination of malignant and benign focal hepatic lesions: T2 weighted vs diffusion-weighted MRI. Br J Radiol 84:319–326
d'Assignies G, Fina P, Bruno O et al (2013) High sensitivity of diffusion-weighted MR imaging for the detection of liver metastases from neuroendocrine tumors: comparison with T2-weighted and dynamic gadolinium-enhanced MR imaging. Radiology 268:390–399
Chavhan GB, Shelmerdine S, Jhaveri K, Babyn PS (2016) Liver MR imaging in children: current concepts and technique. Radiographics 36:1517–1532
Chavhan GB, Caro-Dominguez P (2016) Diffusion-weighted imaging in pediatric body magnetic resonance imaging. Pediatr Radiol 46:847–857
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grasparil, A.D., Gupta, H., Sheybani, E. et al. Low b-value (50–100) diffusion-weighted images detect significantly more hyperintense liver lesions in children than T2-weighted images. Pediatr Radiol 49, 1299–1305 (2019). https://doi.org/10.1007/s00247-019-04455-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-019-04455-9