Abstract
Background
Knowledge of the optimal lengths for central venous catheterization prior to the procedure may lessen the need for repositioning and prevent vascular complications.
Objective
To establish the optimal lengths for non-tunneled central venous catheter insertion through the right and left internal jugular veins.
Materials and methods
We included 92 children who received US-guided central venous catheterization via right or left internal jugular veins in intensive care units. The calculated distance between the skin and carina was considered the optimal length for right and left internal jugular venous catheterization. Univariate and multivariate linear regression analyses was used to identify predictors.
Results
Age, height and weight showed significant correlations with optimal insertion lengths for right and left internal jugular vein approaches on univariate analysis, while height was the only significant independent predictor of optimal insertion length.
Conclusion
The optimal insertion lengths (cm) suggested by our data are, for the right internal jugular vein 0.034 × height (cm) + 3.173, and for the left 0.072 × height (cm) + 2.113.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ultrasonography-guided non-tunneled central venous catheterization has been shown to be a safe procedure that can be performed at the bedside of patients in intensive care units [1, 2]. For children in the intensive care setting, central venous catheters are frequently inserted to measure central venous pressure and to administer drugs or fluid for treatment [3]. However, unlike in an angiography room, the adequacy of the catheter position cannot be assessed until a chest radiograph is obtained after completion of the procedure, leaving open the possibility of malpositioning being undetected for up to several hours. Therefore, knowing the optimal length for central venous catheterization prior to the procedure is clinically important to lessen the need for a time-consuming repositioning procedure, to prevent unnecessary radiation exposure after repositioning and to prevent rare but serious vascular complications of the central venous catheter caused by inappropriate placement of the catheter tip.
Under US guidance central venous catheters are usually inserted though one of the two internal jugular veins because of their large diameter and superficial location [3]. However, although several studies have reported the optimal insertion lengths for central venous catheters through the right internal jugular or subclavian veins in children [4, 5], a more comprehensive overview has not been reported. In addition, only one study reported the optimal length for the left internal vein approach in children [6]. However, the study by Kim et al. [6] was performed by measuring the vascular length on 3-D reformatted CT images, not by assessing actual insertion lengths. Furthermore, they did not consider the length of the subcutaneous tract in their formulas.
Therefore, the purpose of our study is to estimate the optimal length for non-tunneled central venous catheter insertion through the right and left internal jugular veins in children.
Materials and methods
Our institutional review board approved this study and waived the need for informed consent. We retrospectively included, from January 2010 to September 2011, 92 children without cardiovascular anomalies who received US-guided central venous catheterization via the right or left internal jugular veins while in the neonatal or pediatric intensive care unit. All children in the study had initial central venous catheter placement. All central venous catheterizations were performed by pediatric radiologists (J.E.C. and Y.H.C., with 20 years and 8 years of experience, respectively) using a portable sonographic machine (z.one ultra, Zonare Medical Systems, Mountain View, CA) with a 5–10-MHz linear-array transducer and 4-F or 5-F central venous catheters (ARROWgard Blue, Arrow International, Reading, PA). The puncture was done around the apex of the triangle formed by the sternal and clavicular heads of the sternocleidomastoid muscle and the clavicle. Data on age, gender, height and weight at the time of catheter insertion were collected through a retrospective review of the medical records of each child.
Calculation of optimal insertion lengths
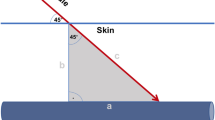
In our routine practice, we record the actual inserted length of the central venous catheter in medical charts, and portable chest radiographs are obtained immediately after completion of central venous catheterization. Data on the inserted lengths of the central venous catheters were obtained upon review of the medical charts. Thereafter, the distance between the carina and catheter tip was measured along the catheter on the portable chest radiograph obtained immediately after catheter insertion (Fig. 1). In this study, we chose the carina as the target anatomical landmark for determination of proper central venous catheter placement, because it has been known to be slightly cephalad to the anatomical junction between the superior vena cava and right atrium [7] and is easily identifiable on chest radiographs. The measured distance between the carina and catheter tip was multiplied by 0.9, because objects are magnified by 8–10% on portable anteroposterior radiographs [4, 8]. Finally, the distance between the skin entry site and the carina along the catheter was calculated as follows:
We considered the distance between the skin and carina to be the optimal insertion length.
Prospective application of the formulas
We tested the formulas in a limited-population pilot study from June 2014 to July 2014. The distance between the catheter tip and the carina was measured using a portable chest radiograph obtained immediately after catheter insertion.
Statistical analysis
Relationships between the optimal insertion length (the distance between the skin and carina) and age, gender, height and weight, respectively, were examined using simple linear regression analysis. We then performed multiple linear regression analysis using the backward method to identify significant independent predictors of the optimal lengths for central venous catheter insertions via right and left internal jugular veins using age, gender, height and weight as independent variables. Variables with an associated significance level greater than 0.2 were removed from the model one at a time. We generated scatter plots of insertion length versus the significant variables and calculated the coefficients of determination (R2) for the right and left internal jugular vein approaches. In addition, we used residual plots to evaluate drift, variance and deviation. The residual standard errors were calculated to measure the discrepancy between the linear model predictions and the observed data. All statistical analyses were performed using MedCalc (MedCalc for Windows, version 12.7.0; MedCalc Software, Mariakerke, Belgium), a commercially available software program. A P-value of less than 0.05 was considered statistically significant.
Results
The study included 54 boys and 38 girls, mean age 18.5 months, range 5 days to 116 months. Central venous catheters were inserted via the right internal jugular vein in 54 and via the left internal jugular vein in 38. Mean age was 20.5 months (range 5 days to 116 months) for right and 15.7 months (range 18 days to 80 months) for left internal jugular vein catheterizations. Detailed demographic data are presented in Table 1.
Univariate analysis revealed that age, height and weight showed significant correlations with optimal insertion lengths for right and left internal jugular veins. Coefficients of determination were highest for height in right and left internal jugular vein insertion groups (Table 2).
For multivariate analysis using the backward method, height was selected as the strongest predictor of optimal insertion length for both right and left internal jugular vein approaches. The addition of other factors failed to contribute significantly in predicting optimal insertion lengths (Table 3,Fig. 2).
Plots of insertion length versus height for the right and left internal jugular vein approaches. a Insertion length for right internal jugular vein catheterization (cm) = 0.034 × height (cm) + 3.173. b Insertion length for left internal jugular vein catheterization (cm) = 0.072 × height (cm) + 2.113. Insertion length = distance from skin entry site to the level of the carina. CVC central venous catheterization, LIJV left internal jugular vein, RIJV right internal jugular vein
The regression equations describing the optimal insertion lengths for central venous catheters inserted via the right and left internal jugular veins were:
The residual plots showed random scattering and a constant variance throughout the entire range of the height for right and left internal jugular vein approaches (Fig. 3). The residual standard errors were 0.757 and 0.829 for right and left internal jugular vein approaches, respectively.
Residual plots of optimal insertion length versus height for the right (a) and left (b) internal jugular vein approaches. The residual plots show no drift and a constant variance throughout the entire range of the height. CVC central venous catheterization, LIJV left internal jugular vein, RIJV right internal jugular vein
After obtaining the formulas, these formulas were applied to 17 consecutive cases of central venous catheterization (12 right and 5 left internal jugular vein catheterizations; 9 boys, 8 girls; mean age 23.7 months, range 2–72 months). The mean distance from the catheter tip to the carina was 5.2 ± 2.9 mm (range 2.0–11.0 mm) for insertion via the right internal jugular vein and 2.9 ± 1.5 mm (range 2.0–11.0 mm) for insertion via the left internal jugular vein. No children needed line repositioning .
Discussion
In various clinical circumstances, central venous catheterization is necessary at the bedside of children in pediatric intensive care units, but it can be difficult and challenging, predominantly because of the children’s small size and risks of associated morbidity and mortality [9]. Because two-dimensional US guidance has been shown to reduce complication rates related to central venous catheter insertion, it has been routinely utilized in clinical practice [1]. When using US guidance, both internal jugular veins are preferred over subclavian veins because internal jugular veins are much larger in diameter and more superficially located than subclavian veins. However, the optimal placement of the central venous catheter with its tip at the superior vena cava–right atrial junction cannot be confirmed by sonography. Thus, portable chest radiographs are required after catheter insertion [10]. If the post-procedural chest radiograph indicates that the central venous catheter is inserted too deeply, repositioning may be needed. A shallowly inserted catheter cannot be advanced and must be exchanged to maintain sterility. Alterations also require another radiograph, with potentially avoidable radiation. Furthermore, complications related to improper catheter positioning have been reported, including cardiac tamponade, severe cardiac arrhythmias, hematomas and superior vena cava syndrome [10]. Consequently, knowledge of the optimal catheter insertion lengths through the right and left internal jugular veins is clinically important.
The ideal position of the catheter tip has been known to be at the junction between the superior vena cava and right atrium [11]. Traditionally the radiographic cavoatrial junction, defined as the intersection between the linear line representing the mediastinum and the curvilinear line representing the right heart border, has been used as a landmark for central venous catheter placement. However this radiographic cavoatrial junction has been shown to be unreliable as a landmark for proper catheter placement because it is quite different from the anatomical cavoatrial junction [12]. Furthermore, the radiographic cavoatrial junction is difficult to accurately identify on portable chest radiographs in children because of the relatively large thymic shadow and parallax effect [13]. Therefore we used the lower margin of the carina as the radiologic landmark for proper central venous catheter placement because the carina is relatively easy to identify on anteroposterior chest radiographs and the anatomical cavoatrial junction has been reported to be consistently slightly caudal to the carina [7]. Yoon et al. [7] noted the carina to be 1.5 ± 0.7 cm cephalad to the anatomical cavoatrial junction (95% confidence interval [CI] 1.3–1.8, range 0.3–2.8 cm).
Previous studies have established that the insertion length is related to age, height and weight, and that height best correlates with the optimal insertion length [4–6]. Our results are in agreement with these studies. According to our results, coefficients of determination, which are statistical measures of how well the regression line approximates real data, were the highest for height in both right and left internal jugular vein approaches.
Specifically, in terms of catheterization via the right internal jugular vein, Andropoulos et al. [4] reported the optimal insertion lengths for right internal jugular placement in infants and children. Compared to their results (insertion length [cm] = 1.54 + 0.09 × height in cm), the optimal lengths of insertion via the right internal jugular vein in our study are generally smaller. We believe this difference may have been caused by the differences in the skin puncture level and the target point of the catheter tips. In their study, they used a high approach to the right internal jugular vein, while we generally used a middle-to-low approach by puncturing the level of the muscular triangle formed by the sternal and clavicular heads of the right sternocleidomastoid muscle. In addition, Andropoulos et al. [4] used the radiographic junction of the superior vena cava and right atrium as the target point for the central venous catheter placement, while we used the carina as the target point for catheter placement.
As for the left internal jugular vein approach, there has been only one study, by Kim et al. [6], that reported the optimal depth for the left internal jugular vein approach. However the length calculated by their formula was quite small; it was measured from the superior border of the left clavicle to the cavoatrial junction on a reformatted CT image, and the distance from the catheter insertion point on the skin to the clavicle was not considered. As an example, if the height of a child was 90 cm, the recommended catheter insertion length would be 8.6 cm in our study, whereas it would be 6.0 cm in the study by Kim et al. [6]. We believe that in clinical practice, our results would be more comprehensive and easier to calculate.
Interestingly, we observed that in our equations obtained through multivariate analysis, the coefficient of determination was relatively lower in the right internal jugular vein approach than in the left internal jugular vein approach (right internal jugular vein approach vs. left internal jugular vein approach was 0.488 vs. 0.721). We believe that the derived insertion length for the right internal jugular vein approach may have been more influenced by variations induced by the puncture level in the neck and the depth of the subcutaneous tissue in the neck because of its relatively short insertion length, compared with that of the left internal jugular vein approach.
There are several limitations to our study. First, we calculated the distance from the skin puncture site to the carina instead of measuring the distance to the anatomical cavoatrial junction, which has been generally considered the ideal location. Therefore, our results may be more appropriate as a guideline for a safe location within the distal superior vena cava rather than an ideal position of the central venous catheter tip at the cavoatrial junction. Second, the study population is relatively small compared with prior studies. Furthermore, the formulas were derived from children age 5 days to 116 months for the right internal jugular vein approach and 18 days to 80 months for the left internal jugular vein approach, so the formulas are only applicable to these age ranges. Third, even though the use of these formulas can be helpful in determining the length of the catheter prior to insertion, the need for post-insertion chest radiograph is not obviated because malposition cannot be completely excluded. Fourth, this study was retrospectively performed. Even though the formulas were prospectively tested in 17 patients, it should be further validated prospectively in a large patient population. Last, the effect of catheter size was not considered in our study. Because the 5-F catheter is stiffer than the 4-F catheter, it would be associated with the shorter length being required, particularly in younger children with more pliable venous systems. However, the subgroup analysis according to the catheter size was not performed because the total population number was small.
Conclusion
This study showed that height is the most significant single predictor for proper central venous catheter placement. In addition, we obtained simple formulas to determine the optimal lengths for right and left internal jugular vein catheterization in children. By applying these formulas in a situation where fluoroscopy is not available at the time of insertion, initial malposition of the central venous catheter may be prevented, thus minimizing the repositioning risks.
References
National Institute for Clinical Excellence (2002) Guidance on the use of ultrasound locating devices for placing central venous catheters. Technology Appraisal Guidance No. 49, September 2002, http://www.nice.org.uk/guidance/ta49/
Maecken T, Grau T (2007) Ultrasound imaging in vascular access. Crit Care Med 35:S178–S185
Trieschmann U, Cate UT, Sreeram N (2007) Central venous catheters in children and neonates — what is important? Images Paediatr Cardiol 9:1–8
Andropoulos DB, Bent ST, Skjonsby B et al (2001) The optimal length of insertion of central venous catheters for pediatric patients. Anesth Analg 93:883–886
Kim JH, Kim CS, Bahk JH et al (2005) The optimal depth of central venous catheter for infants less than 5 kg. Anesth Analg 10:1301–1303
Kim H, Jeong CH, Byon HJ et al (2013) Predicting the optimal depth of left-sided central venous catheters in children. Anaesthesia 68:1033–1037
Yoon SZ, Shin JH, Hahn S et al (2005) Usefulness of the carina as a radiographic landmark for central venous catheter placement in paediatric patients. Br J Anaesth 95:514–517
John SD, Swischuk LE (1995) Chest. In: Swischuk LE, John SD (eds) Differential diagnosis in pediatric radiology. Williams & Wilkins, Baltimore, pp 85–105
Stenzel JP, Green TP, Fuhrman BP et al (1989) Percutaneous central venous catheterization in a pediatric intensive care unit: a survival analysis of complications. Crit Care Med 17:984–988
De Jonge RC, Polderman KH, Gemke RJ (2005) Central venous catheter use in the pediatric patient: mechanical and infectious complications. Pediatr Crit Care Med 6:329–339
Bjarnason H, Lehmann S (1997) Central venous access. In: Castañeda-Zuñiga WR (ed) Interventional radiology. Williams & Wilkins, Baltimore, pp 941–965
Hsu JH, Wang CK, Chu KS et al (2006) Comparison of radiographic landmarks and the echocardiographic SVC/RA junction in the positioning of long-term central venous catheters. Acta Anaesthesiol Scand 50:731–735
Teele SA, Emani SM, Thiagarajan RR et al (2008) Catheters, wires, tubes and drains on postoperative radiographs of pediatric cardiac patients: the whys and wherefores. Pediatr Radiol 38:1041–1053, quiz 1151
Acknowledgments
We thank Allison Alley for language consultation and editing.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choi, Y.H., Cheon, JE., Shin, S.H. et al. Optimal insertion lengths of right and left internal jugular central venous catheters in children. Pediatr Radiol 45, 1206–1211 (2015). https://doi.org/10.1007/s00247-015-3289-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3289-9