Abstract
Skeletal injuries are commonly encountered in infants and young children with abusive head trauma. Although certain patterns of intracranial injury suggest abuse, none are diagnostic. Therefore demonstration of associated unsuspected skeletal injuries has important implications, particularly when highly specific fractures are present. Skull fractures are commonly associated with intracranial injury, but no fracture pattern is indicative of physical abuse. Other skeletal injuries including classic metaphyseal lesions and rib, spine and scapular fractures are strong predictors of abusive head trauma in infants with intracranial injury. It is mandatory to perform rigorous skeletal surveys in infants and young children with clinical and neuroimaging findings concerning for abusive head trauma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 1946 John Caffey [1] described a group of young children with unexplained subdural hematomas and long-bone injuries, and this seminal observation ultimately led to the formulation of a specific medical entity of child abuse. The term “battered child syndrome” was coined by Kempe et al. [2] in 1962. The authors suggested that the syndrome should be considered in any child with a combination of multiple fractures, subdural hematoma and bruises. With the recent emergence of the subspecialty of child abuse pediatrics in the United States, significant efforts have been focused on defining these important associations. The occurrence of silent intracranial injuries from abusive trauma in infants presenting with the typical skeletal injuries (e.g., rib fractures and classic metaphyseal lesions) has led to the practice of obtaining brain CT or MRI in infants with these characteristic fractures. Conversely, it is customary to perform skeletal surveys in young patients who have neuroimaging findings concerning for abusive head trauma.
Many excellent articles and book chapters provide overviews of the imaging features of fractures occurring with child abuse. This review examines the skeletal injuries associated with abusive head trauma. The emphasis is on the evidence base, with several case examples. The reader is encouraged to explore the imaging features of these skeletal injuries in the references provided.
The evidence base
In 2012 a systematic review of the literature by Piteau et al. [3] found several injuries to be significantly associated with abusive head trauma, including skull fracture (co-occurring with intracranial injury), rib, metaphyseal and other long-bone fractures, subdural hematomas, cerebral ischemia, retinal hemorrhages, seizures, apnea and an inadequate history. A recent study that was not included in the Piteau review provides further support for the association of abusive head trauma with certain other injuries. In a patient-level meta-analysis from six cohort studies, Maguire et al. [4] examined the positive predictive values of a combination of seven clinical features (head and neck bruising, rib fracture, skull fracture, long-bone fracture, retinal hemorrhage, seizures and apnea) in conjunction with intracranial injury. They reported that any combination of three or more features yielded a positive predictive value for abusive head trauma of 85% of the children studied [4].
Duffy et al. [5] reviewed the reasons for ordering skeletal surveys in a large consecutive sample of 703 children and reported that children with an apparent life-threatening event or seizure and children with suspected abusive head trauma had the highest rates of positive skeletal surveys. Reece and Sege [6] reviewed the medical records of 287 children ages 1 week to 6½ years who had head injuries. Accidents explained the injuries in 81% of the cases and abuse was present in 19%. They found a significantly higher prevalence of skeletal injuries in children with abusive head trauma vs. those with accidental head injury [6].
Imaging
Many sites and patterns of skeletal injury have been described in cases of child abuse, and these fractures can be stratified on the basis of their specificity for abuse [7]. Some of these are deserving of special consideration in the context of abusive head trauma.
Skull fractures
Although skull fractures are commonly associated with inflicted skeletal injury, they are most often noted in accident victims. In their systematic review covering publications from 1982 to 2000, Kemp and associates [8] found that once major trauma was excluded, the probability of abuse in infants and toddlers with skull fracture was 0.3 (0.19–0.46).
Many authors have studied the pattern of skull fractures in an attempt to identify those that carry a positive association with child abuse. Merten et al. [9] found 93 cases of cranio–cerebral injury in 712 physically abused children and found 67 skull fractures (72%) in this group. Fifty-nine (88%) of these were simple linear parietal or occipital fractures; diastatic, comminuted and depressed fractures were uncommon [9]. In a study of 60 accidental skull fractures, Hobbs [10] found that 55 were linear, 3 complex, 3 depressed, 4 diastatic and 2 of the growing type. In contrast, of 29 abusive skull fractures, 6 were linear, 23 multiple or complex, 12 depressed, 10 diastatic and 6 growing. He concluded that a growing fracture implies a severe impact force and that if a minor injury is alleged in such cases, abuse is likely. Hobbs considered depressed fractures to be strongly suspicious of an inflicted injury from a high impact blunt force, unless a definite history of a direct contact injury with a sharp or pointed object is provided, and that a depressed occipital bone fracture is virtually pathognomonic of abuse [10].
In contrast, Meservy and colleagues [11] found no significant differences in the patterns of skull fracture between abused and accidentally injured children with depressed, diastatic or nonparietal fractures or fractures with complex configurations [11]. However, like Hobbs [10] they found that multiple or bilateral fractures and fractures that crossed suture lines were significantly associated with abuse [11]. Reece and Sege [6] found no differences in the prevalence of complex skull fractures in abusive vs. accidental head injuries. And Kemp and others [8] found in their systematic review that most skull fractures in abused children were linear and parietal in location; they emphasized the lack of agreement of studies with respect to the predictive value of diastatic and complex fractures for abuse.
We recently reported the yield of radiographic skeletal surveys in 567 infants (<1 year old) with suspected abuse [12]. Head injury was the clinical indication for the skeletal survey in 42% of cases. Skull fractures were present on the initial skeletal survey in 138 (24%) infants. Seventy-six (55%) of the infants with skull fractures had simple skull fractures and 62 (45%) had complex injuries (Figs. 1 and 2). Simple fractures involved the parietal bone in 73/76 (96%) cases. Overall, 26 of 138 (19%) infants with skull fractures had a positive skeletal surveys (clinically unsuspected fractures), but this prevalence was higher in infants with complex skull fractures (17/62, or 27%) than those with simple fractures (9/76, or 12%) (P = 0.02). Infants with a complex skull fracture were at higher risk for other fractures (odds ratio 2.8; 95% CI 1.2–6.9).
Imaging in a 12-month-old girl with scalp swelling and no history or other signs of trauma. The child had been in foster care since age 10 months for maternal neglect. A skeletal survey was performed. Lateral (a) and anteroposterior (AP) (b) radiographs of the skull show a linear right parietal fracture (arrows). AP (c) and lateral (d) views of the left forearm show a buckle fracture of the distal radial metaphysis (arrows) with subperiosteal new bone formation. e Posteroanterior (PA) view of the left hand shows a possible healing non-displaced fracture involving the base of the left 5th metacarpal (arrow). f PA view of the left hand from the 2-weeks follow-up skeletal survey shows healing of the metacarpal fracture (arrow). Head CT showed no intracranial injury
Imaging in a 2-month-old girl who became irritable after an unwitnessed fall from a small chair. Bilateral parietal skull fractures had been noted at 1 month of age. a Axial head CT shows an interhemispheric subdural hematoma (arrow). b Three-dimensional rendering of a CT acquisition shows a diastatic left parietal fracture. c Portable anteroposterior (AP) radiograph of the chest shows healing fractures of the left 5th and 6th ribs posteromedially (arrowheads); a healing left acromial fracture is partly obscured by the hand of the holding adult (arrow). d Coned AP view of the left humerus from the skeletal survey shows the left acromial fracture to advantage (arrow). e AP radiograph of the left tibia shows a healing classic metaphyseal lesion of the proximal tibia (arrow). There was also a classic metaphyseal lesion on the right distal tibia (not shown). f Oblique anterior maximum-intensity projection of the Na F18-PET bone scan shows increased tracer uptake corresponding to the rib and acromial fractures as well as the classic metaphyseal lesion (arrows)
This discussion leads to an important practical question: Which patients with a skull fracture should undergo skeletal survey? The findings vary.
Wood et al. [13] published a retrospective review of infants with isolated skull fracture. Among 341 infants, 31% had clinical findings that raised suspicion for abuse and 42% had complex skull fractures. Skeletal surveys were obtained in 141 infants (41%) and detected additional fractures in only 2 (1.4%). Both infants with positive skeletal surveys had other clinical findings that raised suspicion for abuse. The authors concluded that skeletal surveys rarely added information beyond the history and physical findings to support a report to child protective services [13].
In contrast, Laskey et al. [14] reviewed the yield of skeletal surveys in children ≤18 months old presenting with isolated skull fractures without significant intracranial injury. Of 175 patients, 150 (86%) underwent a skeletal survey, which revealed additional fractures in 6% of patients, and only one of these was older than 6 months. The authors concluded that a skeletal survey may yield clinically and forensically relevant data in such patients [14].
In their retrospective review Duffy et al. [5] reported that among the 38 children in whom positive skeletal survey results directly influenced the clinical diagnosis, three infants presented with a history of a fall, had isolated skull fractures on head CT and had no stigmata of abuse. The authors suggested that a skeletal survey should be performed in young children with isolated skull fractures and a history of trauma, until additional data are available [5].
A 2013 retrospective review by Deye et al. [15] of 201 infants who were the subject of child abuse consultations and skeletal imaging for apparently isolated skull fractures demonstrated additional fractures on skeletal survey in 12 infants (6%). The authors also reported that patient age, trauma history and skull fracture type (simple/complex) were not sensitive predictors of finding additional fractures on skeletal survey [15].
Although the data do not provide clear answers to the above question, it is reasonable to conclude that the majority of children with skull fractures do not require global skeletal imaging assessments, but all infants and young children with skull fractures should have a careful clinical evaluation and if abuse is a serious differential consideration, consultation with a child protection team is appropriate. This multi-disciplinary approach should permit selection of those children in whom a skeletal survey is appropriate.
Rib fractures
Rib fractures have a high specificity for infant abuse and their presence is often central to diagnosis (Figs. 2 and 3). In their systematic review, Kemp and associates [8] found that after major trauma was excluded rib fractures had the highest probability for abuse (odds ratio 0.71, 95% confidence interval 0.42–0.91). Prevalence of rib fractures among children with suspected or confirmed abuse ranges from 8.7% to 14% [12, 16, 17]. The common occurrence of rib fractures and classic metaphyseal lesions in infants with abusive head trauma is well documented [3, 18, 19]. In the recent patient-level meta-analysis from six cohort studies that estimated the probability of abusive head trauma, Maguire et al. [4] demonstrated that rib fractures offered the strongest evidence of abusive head trauma, with an odds ratio of 45. In their review of more than 1,000 infants and young children with intracranial injury, retinal hemorrhages and rib fractures were the most discriminating clinical features to estimate the probability of abusive head trauma [4]. In our retrospective review of the yield of skeletal surveys for suspected abuse, a total of 490 rib fractures were identified (mean, 6.4; range, 1–24) in 77 children (15.7%) (mean age, 4 months; range, 1–12 months). A higher prevalence of intracranial injury among infants with rib fractures was not demonstrated, but we did not attempt to segregate infants with probable abusive head trauma from others with intracranial injury [12].
Imaging in a 5-month-old girl who presented with a possible seizure. Head CT demonstrated bilateral convexity and interhemispheric subdural hematomas. a Axial T2-W fluid-attenuated inversion recovery (FLAIR) MR image demonstrates thin bilateral hyperintense convexity and interhemispheric subdural hematomas (arrowheads). Chronic posterior fossa subdural hematomas were also present. A skeletal survey was performed. b Anteroposterior (AP) radiograph of the thorax shows healing posterior and lateral rib fractures (arrowheads) and a healing right clavicle fracture (arrow). c Coned down AP view of the right shoulder defines the healing clavicle fracture (arrow) as well as a proximal humeral classic metaphyseal lesion (arrowhead). Ophthalmological exam revealed bilateral retinal hemorrhages
The classic metaphyseal lesion
The classic metaphyseal lesion is a hallmark of abusive injury (Figs. 2 and 3). This injury has been studied extensively, most recently by correlating the features between high resolution CT and histopathology [20]. In their retrospective study covering a 10-year period, Kleinman and others [19] compared the prevalence of the classic metaphyseal lesions on high-detail American College of Radiology (ACR) standardized skeletal surveys in infants at low and high risk for abuse. Low-risk infants met all of the following criteria: skull fracture without significant intracranial injury on head CT, history of a fall, and no other social risk factors for abuse. High-risk infants met all of the following criteria: significant intracranial injury, retinal hemorrhage and skeletal injuries (excluding classic metaphyseal lesions and skull fractures) [19]. There were 42 low-risk infants (age range, 0.4–12 months; mean age, 4.4 months) and 18 high-risk infants (age range, 0.8–10.3 months; mean age, 4.6 months) [19]. At least one classic metaphyseal lesion was identified in nine infants (50%) in the high-risk category and none in the low-risk group (P < 0.0001; 95% CI 0–8% to 29–76%) [19]. Although this study did not specifically address the connection between classic metaphyseal lesions and abusive head trauma, the occurrence of classic metaphyseal lesions in 50% of the high-risk-for-abuse cohort supports this association [19].
Spinal injuries
Some studies report spinal injuries with coexistent subdural hematoma and other evidence of abusive head trauma [17, 21, 22]. We recently reported a significant correlation between spinal fractures and intracranial injury (Fig. 4) [23]. Ten of 14 (71%) children with spinal fractures had intracranial injury; eight children had a combination of unilateral or bilateral subdural hematomas and brain parenchymal injury or subarachnoid hemorrhage suggestive of abusive head trauma [23]. One of these children had an unsuspected skull fracture on skeletal survey with MRI findings suggesting hemorrhage along the margins of the tentorium and mild restricted diffusion in the cerebellar hemispheres [23]. Another child presented with right hemiparesis had brain MR findings initially interpreted as consistent with an acute ischemic injury; however after demonstration of fractures on the skeletal survey, additional brain and spine MR imaging pointed strongly to abusive head trauma [23]. Among all patients who underwent skeletal survey and neuroimaging for suspected abuse, we found a significant correlation between spinal fractures and intracranial injury (P < 0.05) [23]. Children with spinal fractures were at significantly greater risk for intracranial injury than those without spinal injury (odds ratio 5; 95% CI 1.6–16.4); among children with positive skeletal surveys this correlation was also significant (P < 0.05) [23]. Children with spinal fractures were at significantly greater risk for intracranial injury than those without spinal injury and positive skeletal survey (odds ratio 5.5; 95% CI 1.6–18.8) [23].
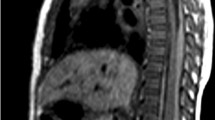
Imaging in a 12-month-old girl with altered mental status. a Axial cranial CT shows interhemispheric subdural hematomas (arrows) and loss of the gray–white matter differentiation in the left parieto–occipital and right frontal regions (arrowheads). b Axial diffusion-weighted MR image shows extensive bilateral cerebral restricted diffusion, which was confirmed on apparent diffusion coefficient maps (not shown). Retinal hemorrhages were also evident on MR imaging (not shown). Coned AP (c) and lateral (d) views of the thorax from the skeletal survey reveal definite compression deformity of the vertebral bodies of T7, T8 and T9 (arrows) and possibly T6 and T10 (arrowheads). Additional healing long-bone metaphyseal fractures were present (not shown)
Scapular fractures
Scapular fractures are most often noted in infants who have typical patterns of abuse elsewhere, and therefore they appear to occur from indirect forces (Fig. 2). Typically the fractures occur through the middle third of the acromion, and they should not be confused with a normal anatomical variant [7]. In our retrospective review of the yield of skeletal surveys in infants, 13 scapular fractures were noted in 8 infants; they all had additional skeletal injuries and 6 had associated intracranial injury. Scapular fracture showed a statistically significant correlation with intracranial injury (P = 0.029); infants with scapular fractures had a higher risk of associated intracranial injury (odds ratio 5.5, 95% CI 1.1–27.4) [12].
Other fractures
The presence of multiple other osseous injuries, particularly those of differing ages (Fig. 1), often points to an abusive etiology for intracranial injury in infants and young children. Moderate specificity injuries, such as fracture of the hands and feet (Fig. 1) and epiphyseal separations or Salter–Harris injuries, lend strong support to the diagnosis of abusive head trauma, particularly in non-ambulatory children. It is notable that none of Caffey’s [1] original cases with subdural hematomas had documented high-specificity injuries.
Imaging strategies
All infants and young children with suspected abusive head trauma should undergo a radiographic skeletal survey according to ACR guidelines [24]. This should be followed in most cases after 2 weeks with a repeat skeletal survey. Additional skeletal imaging with scintigraphy, particularly Na F18-PET, should be employed when initial radiographic findings are inconclusive or when the documentation of initially radiographically occult injuries is desired (Fig. 2). Focused MRI has value in select cases, particularly when epiphyseal separation and spinal fracture or dislocations are present. Whole-body MRI is likely to be used more frequently in this context, particularly when high-field-strength imaging is optimized with appropriate surface coils and imaging parameters [25, 26].
Conclusion
Skeletal injuries are commonly encountered with abusive head trauma in infants and young children. Although certain patterns of intracranial injury suggest abuse, none are diagnostic. Therefore demonstration of associated unsuspected skeletal injuries has important implications, particularly when highly specific fractures are present. The significance of the neuroimaging and clinical findings may come under considerable scrutiny in child welfare and criminal proceedings, during which various possible explanations for the medical findings are explored and often disputed. As a component of a thorough multidisciplinary assessment, rigorous skeletal imaging may provide reliable documentation of child abuse and permit protection of the child and others at risk in the domestic environment.
References
Caffey J (1946) Multiple fractures in the long bones of infants suffering from chronic subdural hematoma. Am J Roentgenol Radium Ther 56:163–173
Kempe CH, Silverman FN, Steele BF et al (1962) The battered-child syndrome. JAMA 181:17–24
Piteau SJ, Ward MGK, Barrowman NJ et al (2012) Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: a systematic review. Pediatrics 130:315–323
Maguire SA, Kemp AM, Lumb RC et al (2011) Estimating the probability of abusive head trauma: a pooled analysis. Pediatrics 128:e550–564
Duffy SO, Squires J, Fromkin JB et al (2011) Use of skeletal surveys to evaluate for physical abuse: analysis of 703 consecutive skeletal surveys. Pediatrics 127:e47–52
Reece RM, Sege R (2000) Childhood head injuries: accidental or inflicted? Arch Pediatr Adolesc Med 154:11–15
Kleinman P (1998) Diagnostic imaging of child abuse, 2nd edn. Mosby, Maryland Heights
Kemp AM, Dunstan F, Harrison S et al (2008) Patterns of skeletal fractures in child abuse: systematic review. Br Med J 337:a1518
Merten DF, Osborne DR, Radkowski MA et al (1984) Craniocerebral trauma in the child abuse syndrome: radiological observations. Pediatr Radiol 14:272–277
Hobbs CJ (1984) Skull fracture and the diagnosis of abuse. Arch Dis Child 59:246–252
Meservy CJ, Towbin R, McLaurin RL et al (1987) Radiographic characteristics of skull fractures resulting from child abuse. AJR Am J Roentgenol 149:173–175
Barber I, Perez-Rossello JM, Wilson CR et al (2014) The yield of high-detail radiographic skeletal surveys in suspected infant abuse. Pediatr Radiol. doi:10.1007/s0024701430643
Wood JN, Christian CW, Adams CM et al (2009) Skeletal surveys in infants with isolated skull fractures. Pediatrics 123:e247–e252
Laskey AL, Stump TE, Hicks RA et al (2013) Yield of skeletal surveys in children ≤18 months of age presenting with isolated skull fractures. J Pediatr 162:86–89
Deye KP, Berger RP, Lindberg DM et al (2013) Occult abusive injuries in infants with apparently isolated skull fractures. J Trauma Acute Care Surg 74:1553–1558
Day F, Clegg S, McPhillips M et al (2006) A retrospective case series of skeletal surveys in children with suspected non-accidental injury. J Clin Forensic Med 13:55–59
Karmazyn B, Lewis ME, Jennings SG et al (2011) The prevalence of uncommon fractures on skeletal surveys performed to evaluate for suspected abuse in 930 children: should practice guidelines change? AJR Am J Roentgenol 197:W159–W163
King J, Diefendorf D, Apthorp J et al (1988) Analysis of 429 fractures in 189 battered children. J Pediatr Orthop 8:585–589
Kleinman PK, Perez-Rossello JM, Newton AW et al (2011) Prevalence of the classic metaphyseal lesion in infants at low versus high risk for abuse. AJR Am J Roentgenol 197:1005–1008
Tsai A, McDonald AG, Rosenberg AE et al (2014) High-resolution CT with histopathological correlates of the classic metaphyseal lesion of infant abuse. Pediatr Radiol 44:124–140
Swischuk LE (1969) Spine and spinal cord trauma in the battered child syndrome. Radiology 92:733–738
Kemp AM, Joshi AH, Mann M et al (2010) What are the clinical and radiological characteristics of spinal injuries from physical abuse: a systematic review. Arch Dis Child 95:355–360
Barber I, Perez-Rossello JM, Wilson CR et al (2013) Prevalence and relevance of pediatric spinal fractures in suspected child abuse. Pediatr Radiol 43:1507–1515
American College of Radiology (2011) ACR–SPR practice guideline for skeletal surveys in children: revised 2011 (resolution 54). ACR, Reston, VA, pp 1–6. http://www.acr.org/~/media/9bdcdbee99b84e87baac2b1695bc07b6.pdf. Accessed 29 May 2014
Drubach LA, Johnston PR, Newton AW et al (2010) Skeletal trauma in child abuse: detection with 18 F-NaF PET. Radiology 255:173–181
Perez-Rossello JM, Connolly SA, Newton AW et al (2010) Whole-body MRI in suspected infant abuse. AJR Am J Roentgenol 195:744–750
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barber, I., Kleinman, P.K. Imaging of skeletal injuries associated with abusive head trauma. Pediatr Radiol 44 (Suppl 4), 613–620 (2014). https://doi.org/10.1007/s00247-014-3099-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-014-3099-5