Abstract
Background
Before introducing 70-kVp settings in the low-kilovoltage strategies for pediatric examinations, it was mandatory to demonstrate, at similar dose levels, an equivalence of image quality at 70 kVp and 80 kVp.
Objective
To assess image quality of chest CT examinations acquired at 70 kVp in comparison with standard scanning at 80 kVp.
Materials and methods
We prospectively evaluated 129 children with a 70-kVp scanning protocol (group 1). All scanning parameters were kept similar to those usually selected for pediatric standard 80-kVp protocols, except the milliamperage increased by a factor of 1.6 to maintain comparable radiation dose. Image quality of group 1 examinations was compared to that of a paired population scanned at 80 kVp (group 2). The noninferiority hypothesis was fixed at 10% of the mean level of image noise.
Results
There was no significant difference in the mean dose length product (DLP) and the volume computed tomography dose index (CTDIvol) between the groups (DLP: 20.5 ± 5.8 mGy.cm [group 1] vs. 19.7 ± 7.6 mGy.cm [group 2]; P = 0.06) (CTDIvol: 0.8 ± 0.1 mGy [group 1] vs. 0.8 ± 0.18 mGy [group 2]; P = 0.94). The mean of differences in image noise between group 1 and group 2 examinations was −1.38 (−2.59; −0.18), verifying the noninferiority hypothesis. Subjective image quality did not significantly differ between group 1 and group 2 examinations (P = 0.18).
Conclusion
At equivalent radiation dose levels, 70-kVp protocols provide similar image quality to that achievable at 80 kVp.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Technological developments of multidetector CT have contributed to a substantial increase in its diagnostic implications and accuracy in children [1]. In parallel, great efforts have been directed toward optimization of pediatric CT with the main objective of applying the ALARA principle because of the risk of radiation-induced cancer in this population [2–4]. After initial trends mainly focusing on the reduction of tube current, there has been a growing interest in scanning children at low energy levels. Standard tube potentials, as they are used in adults, have been shown to increase radiation in children without significantly improving image quality [5, 6]. In general, 80 kVp for the youngest (smallest) children, increasing to 100 kVp to school-age children, with a maximum of 120 kVp is generally recommended for general chest multi-detector CT [7]. Several studies in recent years have reported the possibility of a broader use of 80 kVp protocols for scanning pediatric populations [8, 9]. Lowering the tube voltage has the additional advantage of increasing the attenuation of iodinated contrast medium because of a greater photoelectric effect and increased Compton scattering [10, 11]. The recent introduction of 70 kVp in clinical practice [12] offers the possibility to further exploit the advantages of low-kVp scanning in pediatric populations. However, these potential options cannot be investigated without assessing the image quality achievable at 70 kVp in pediatric populations. The present study was thus undertaken to compare, at equivalent radiation dose, the image quality of chest CT examinations acquired at 70 kVp to that of the current standard of reference, namely 80-kVp scanning protocols.
Materials and methods
CT scanning protocols
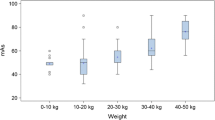
Since the introduction of 70 kVp as a commercial product on dual-source 128-slice multi-detector CT systems (Somatom Definition Flash; Siemens Healthcare, Forchheim Germany), the standard scanning protocol for pediatric chest CT examinations in our department systematically used this kilovoltage, replacing 80 kVp, i.e. the kilovoltage previously systematically selected on the same CT unit for this population of patients. The choice of the reference tube current-time product (i.e. reference mAs) for the 70-kVp examinations was established on a body-weight-adaptive scheme similar to that used for 80-kVp protocols (Fig. 1). It required an adjustment of the milliamperage by a factor of 1.6 (the manufacturer’s recommendation) in order to maintain the same radiation dose (Fig. 2). The multiplication factor was individually determined prior to CT scanning: (1) for a given body weight, the CT technologist entered the parameters of an 80 kVp protocol, which provided the CTDIvol of a theoretical 80-kVp examination; (2) then the kilovoltage selection was set at 70 kVp and the milliamperage was adapted to ensure the same CTDIvol. The weight-based low-dose protocols at 80 kVp used in our clinical routine resulted from a 3-year experience of chest CT scanning with a second-generation dual-source CT scanner. The pragmatic approach to the establishment of the milliamperage settings at 80 kVp was to ensure a diagnostic image quality at the lowest radiation dose. The milliamperage was adjusted empirically to the reference noise level (the standard deviation of the CT numbers measured in the tracheal lumen) of diagnostic pediatric chest CT images, being in the range of 10.0–12 HU, higher for larger patients. The 80-kVp protocols had been established under the supervision of a senior radiologist with 25 years’ experience in pediatric chest CT (JR). The imaging protocol uses higher tube current for children of older age and greater weight and thus compensates for different attenuations in neonates and small children. As shown in Fig. 1, the reference mAs for 80-kVp protocols ranged from 49 to 63, applicable to children ranging from newborns to children up to 41 kg.
Phantom validation of maintenance of radiation dose at 70 kVp after adjustment of the tube current by a factor of 1.6. A standard 16-cm water CT phantom was scanned twice using similar parameters (collimation: 64 × 2 × 0.6 mm with z-flying focal spot for the simultaneous acquisition of 128 overlapping 0.6-mm slices; pitch: 2.0; B20f kernel for image reconstruction) at 70 kVp and 80 mAs (a) and 80 kVp and 50 mAs (b). The CTDIvol was maintained at 0.79 mGy for both acquisitions. Note that the image noise was 20.7 HU in (a) and 20.5 HU in (b). CTDI vol volume computed tomography dose index
The other scanning parameters for standard chest CT examinations consisted of thin-collimated (i.e. 64 × 2 × 0.6 mm), high-pitch (i.e. pitch of 2.0) and high-temporal-resolution acquisitions over the entire thorax, using two tubes with a single energy in a non–electrocardiographically gated mode. The acquisitions were obtained without sedation or general anesthesia, always in the craniocaudal direction after deep inspiration (whenever possible); there was no activation of the automatic tube current modulation. Contrast agent was manually injected if clinically indicated. The scan was started immediately after contrast material injection. From each raw dataset, contiguous transverse images were reconstructed with a slice thickness of 1 mm with a standard filtered back projection-algorithm using a high-spatial-resolution kernel (B50, lung images) and a soft-tissue kernel (B20, mediastinal images), respectively. This observational study with retrospective analysis of data was approved by the institutional ethics committee with waiver of informed consent in agreement with national regulations.
Study population
Study groups
Over a 6-month period (September 2011–March 2012), 129 consecutive children underwent a noncontrast (n = 75) or contrast-enhanced (n = 54) chest CT examination at 70 kVp; they will be further referred to as group 1 patients. The main clinical indications for chest CT included acquired respiratory diseases (n = 71), congenital cardiovascular diseases (n = 23), cystic fibrosis (n = 16), congenital bronchopulmonary diseases (n = 14) and miscellaneous disorders (n = 5). In order to perform comparative analysis of image quality at 70 kVp and 80 kVp, 129 children matched by age, body weight and type of chest CT examination (i.e. contrast or noncontrast) were retrospectively selected from our database of children prospectively scanned at 80 kVp on the same CT unit over a 2-year period (preceding installation of the 70-kVp protocol); they will be further referred to as group 2 patients. Each paired dataset was chosen as follows. After each 70-kVp examination, we searched for the most recent examination in our 80-kVp database fulfilling the following criteria: (1) same age (±1 year) and weight (±1 kg); (2) similar technical conditions (i.e. contrast- or noncontrast examination). The paired datasets were not matched by gender nor clinical indication for chest CT examination. Figure 3 illustrates the age and gender distribution in the studied populations.
Sample size calculation
We chose image noise at the level of the trachea on mediastinal images as a primary outcome for the sample size computation because measurements at this anatomical site on mediastinal images are typically used for assessing objective image noise on chest CT examinations. We assumed that, in the worst-case scenario, the dose reduction induced by the reduced kilovoltage (i.e. 70-kVp protocol) could increase the image noise. We used a noninferiority hypothesis for computing an estimated sample size, estimating that a small increase in image noise (i.e. the worst-case scenario) would be acceptable with respect to the potential benefits of the 70-kVp scanning mode for pediatric chest CT. On standard examinations (i.e. 80 kVp), the mean image noise measured at the level of the trachea on mediastinal images had been estimated at 10.3 ± 3.9 HU (mean ± standard deviation) in our database of 506 consecutive pediatric chest CT examinations [13], values within the range of recent reports [14]. We hypothesized that an increase in noise ranging between 5% and 10% could be acceptable with the 70-kVp protocol. Consequently, the noninferiority margin was fixed at 10% of the mean level of image noise, namely 1.03 rounded to 1. Assuming a correlation value of 0.5 between the two measurements of noise according to the two reconstruction techniques, a standard deviation of 4, an estimated number of 126 patients was necessary for 80% power with significance of 2.5% (significance level recommended for the noninferiority test). During the inclusion period, the investigators enrolled a total of 129 consecutive patients in the present investigation.
Parameters analyzed
Scanning characteristics in groups 1 and 2
The readers systematically recorded effective tube current (eff mAs), the volume-weighted CT dose index (CTDIvol) in milligrays (mGy) and the dose length product (DLP) in milligray.centimeters (mGy.cm) for all group 1 and group 2 examinations.
Image analysis in groups 1 and 2
For each patient group, objective and subjective image quality were evaluated. Objective image quality was based on image noise analysis; it was determined by measuring the standard deviation of the attenuation value in Hounsfield units within a circular region-of-interest placed in the tracheal lumen at the level of the aortic arch. The regions of interest were positioned to encompass the homogeneous portion of the air column without including surrounding soft-tissue structures. The surface of the regions of interest varied according to the tracheal diameter: the average region of interest was 0.25 cm2 for tracheal diameters of 0.5 cm and larger; the smallest surface (i.e. 0.09 cm2) was measured within the tracheal lumen of a newborn (tracheal diameter: 0.3 cm).
Subjective image quality of lung and mediastinal images was specifically assessed, based on the analysis of the impact of image noise on the analyzability of a set of anatomical structures. On mediastinal images the readers scored the analyzability of four structures: (1) the thymus, (2) the trachea and adjacent lymph node station at the level of the aortic arch, (3) the carina and adjacent lymph node stations and (4) the esophagus. On lung images the readers scored the analyzability of four anatomical structures: (1) the pulmonary fissures, (2) proximal bronchi and adjacent pulmonary vessels (i.e. structures down to the subsegmental level), (3) peripheral bronchi and adjacent pulmonary vessels (i.e. structures beyond the subsegmental level) and (4) peripheral vascular structures within 10 mm of pleura. These structures were chosen on the basis of the European guidelines on quality criteria for multislice CT [15]. Each individual structure was rated using a four-point scale (score 1, no image noise and clear delineation of the structure; score 2, mild image noise responsible for slight blurring of the structure; score 3, moderate image noise responsible for moderate blurring of the structure; score 4, marked noise and extensive blurring that makes reliable analysis of the structure impossible). The term “blur” is used to mean “degradation of the delineation of a structure.” The mean value of the individual scores on lung images defined the image quality of lung images; the mean value of the individual scores on mediastinal images defined the image quality of mediastinal images. The mean value of the lung and mediastinal scores defined the image quality of the entire chest CT examination, scoring 1 to 4 (scores 1 to 3 were diagnostic; score 4 was nondiagnostic). No attempt was made to analyze image quality of the liver or upper abdomen because our examinations consisted of chest CT scans.
Conditions of image analysis
Two chest radiologists with CT experience of 4 and 7 years (SH and TN, respectively) evaluated subjective and objective image quality by consensus. In cases of discordant scores in subjective image analysis, the corresponding images were reanalyzed in presence of a third reader with 10 years’ experience (JBF). Results of subjective image quality represented concordant readings. Image analysis was performed on a clinical workstation (syngo MultiModality Workplace; Siemens, Erlangen, Germany) onto which lung and mediastinal images of group 1 and group 2 examinations had been systematically transferred. Group 1 and group 2 examinations were presented in random order. Images were viewed using standard mediastinal window settings (width 400 HU, center 40 HU) and lung parenchymal window settings (width, 1,600 HU; center, −600 HU). Adjustment of window level and width was allowed during the qualitative assessment.
Statistical analysis
The statistical analyses were performed using SAS software (SAS Institute Inc., Cary, NC). Results were expressed as means and standard deviations for continuous variables, and frequencies and percentages for categorical variables. The noninferiority hypothesis was assessed using a two-sided 95% confidence interval for the true difference between the two means of image noise measured at the level of the trachea on mediastinal images (scanning mode at 70 kVp minus standard scanning mode at 80 kVp). Noninferiority could be acknowledged if the upper limit of this confidence interval was lower than 0.77 (i.e. the noninferiority margin). After the test run of noninferiority, it is possible to infer superiority if the two following conditions hold: (1) the assumption of noninferiority is accepted; (2) the two-sided test of difference between the means allows one to reject equality of means and allows one to conclude in the sense of superiority [16]. This procedure was employed for the evaluation of image noise at the level of the trachea on mediastinal images. For continuous variables, comparisons between groups were performed using a paired Student’s t-test. Comparisons of image quality scores between groups were performed using a Wilcoxon test. The statistical significance was defined as P < 0.05.
Results
Group 1 and group 2 demographics
Group 1 patients included 75 boys and 54 girls with a mean (±SD) age of 4.6 ± 3.95 years (range: 0.01–15.62; median: 3.58) and a mean (±SD) body weight of 16.3 ± 10 kg (range: 2.16–40; median: 15). Group 2 patients consisted of 65 girls and 64 boys with a mean (±SD) age of 4.6 ± 3.9 years (range: 0–13.8; median: 3.44) and a mean (±SD) body weight of 16.2 ± 10 kg (range: 2.1–41; median: 15). There was no statistically significant difference in the mean value of body weight (P = 0.41) and age (P = 0.68) between groups 1 and 2.
Radiation dose in group 1 and group 2
The mean (±SD) effective tube current time product was 83 ± 8.0 mAs in group 1 and 51.2 ± 10.3 mAs in group 2. The mean dose length product was 20.5 ± 5.8 mGy.cm (range: 12–41) in group 1 and 19.7 ± 7.6 mGy.cm (range: 5–50) in group 2 (P = 0.06). The higher range of dose length product values in group 2 compared to group 1 could be explained by the lack of strict similarity in the size of the chest in each pair of children. Moreover, because the paired datasets were not matched by clinical indications, some CT examinations might have also included the cervical region or liver.
Comparison of image quality between groups 1 and 2
Objective image quality
The noninferiority hypothesis was verified as the difference of means of image noise between group 1 and group 2 was −1.38 with a confidence interval (CI) of −2.59; −0.18. Similar findings were observed when stratifying group 1 and group 2 patients according to the patients’ body weight (<15 kg or ≥15 kg): (1) At <15 kg, the difference of the means was −1.50 (CI: −3.61; 0.61); (2) At ≥15 kg, the difference of the means was −1.27 (CI: −2.55; 0.01).
The mean image noise was significantly lower in group 1 compared to group 2 (group 1: 9.9 ± 6.3 HU; group 2: 11.3 ± 6.6 HU; P = 0.025). This difference in objective image noise was not observed when comparing group 1 and group 2 patients <15 kg (group 1: 12.4 ± 7.2 HU; group 2: 14 ± 7.6 HU; P = 0.160), but it was close to statistical significance when comparing group 1 and group 2 patients ≥15 kg (group 1: 7.5 ± 4.1 HU; group 2: 8.8 ± 4.2 HU; P = 0.051).
Subjective image quality
There was no statistically significant difference when comparing the means of the overall scores of chest CT examinations between group 1 and group 2 whether considering the populations as a whole (P = 0.1803) (Table 1) or stratifying them according to the patients’ body weight (<15 kg: P = 0.865; ≥15 kg: P = 0.090) (Table 2).
No significant difference was observed when comparing the overall scores for mediastinal images between group 1 and group 2 (P = 0.800) (Table 1) or the subgroups according to body weight (<15 kg: P = 0.486; ≥15 kg: P = 0.801) (Table 2).
The scores of subjective image quality of mediastinal images were also analyzed in the paired subgroups of examinations acquired with (n = 54) and without (n = 75) administration of contrast material. Concerning the 54 pairs of chest CT angiographic examinations, the mean score of subjective image quality was 2.10 at 80 kVp and 2.20 at 70 kVp (P = 0.04). Concerning the 75 paired children who underwent a noncontrast chest CT examination, the mean score of subjective image quality was 2.01 at 80 kVp and 1.92 at 70 kVp (P = 0.02).
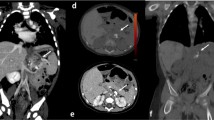
Comparison of scores of image quality for lung images showed significantly lower scores in group 1 compared to group 2 (P = 0.042) (Table 1) in the overall study group; similar findings were observed for patients ≥15 kg (P = 0.029), while no difference was observed for patients <15 kg (P = 0.5099) (Table 2). In group 1 examinations, all lung images were of diagnostic quality; similar findings were observed in group 2. Figures 4, 5 and 6 illustrate subjective image quality in different categories of age: 0–1 year (Fig. 4); 1–5 years (Fig. 5); 5–10 years (Fig. 6). Figure 7 compares the image quality of lung and mediastinal images of contrast-enhanced chest CT examinations, illustrating the better vascular attenuation at 70 kVp.
Comparison of image quality at 70 kVp and 80 kVp in matched patients (category: 0–1 year old). a, b Axial CT (70 kVp) . Mediastinal (a) and lung (b) images obtained at the level of the right bronchus intermedius in a 9-month-old girl (weight: 7.5 kg). Subjective image quality of both images was rated as 2.75. Objective image noise was 31.6 HU. c, d Axial CT (80 kVp) imaging. Mediastinal (c) and lung (d) images obtained at the same anatomical level in a 2-month-old boy (weight: 7.1 kg). Subjective image quality of lung and mediastinal images was rated as 2.75 and 3, respectively. Objective image noise was 15.9 HU
Comparison of image quality at 70 kVp and 80 kVp in matched patients (category: 1–5 years old). a, b Axial CT (70 kVp). Mediastinal (a) and lung (b) images obtained at the level of the right bronchus intermedius in a 5-year-old girl (weight: 18 kg). Subjective image quality of lung and mediastinal images was rated as 1.75 and 2, respectively. Objective image noise was 8.4 HU. c, d Axial CT (80 kVp) imaging. Mediastinal (c) and lung (d) images obtained at the same anatomical level in a 5-year-old girl (weight: 18 kg). Subjective image quality of both images was rated as 2. Objective image noise was 5.5 HU
Comparison of image quality at 70 kVp and 80 kVp in matched patients (category: 5–10 years old). a, b Axial CT (70 kVp). Mediastinal (a) and lung (b) images obtained at the level of the right bronchus intermedius in a 10-year-old girl (weight: 39 kg). Subjective image quality of lung and mediastinal images was rated as 1.5 and 1.75, respectively. Objective image noise was 9.8 HU. c, d Axial CT (80 kVp). Mediastinal (c) and lung (d) images obtained at the same anatomical level in a 10-year-old boy (weight: 38 kg). Subjective image quality of lung and mediastinal images was rated as 1 and 2, respectively. Objective image noise was 3.8 HU
Comparison of image quality of chest CT angiograms at 70 kVp and 80 kVp in matched patients (category 0–1 year old). a, b Axial CT (70 kVp). Mediastinal (a) and lung (b) images obtained at the level of the right bronchus intermedius in a 1-year-old girl (weight: 11 kg). Subjective image quality of lung and mediastinal images was rated as 2.3 and 2, respectively. Objective image noise was 7.8 HU. c, d Axial CT (80 kVp). Mediastinal (c) and lung (d) images obtained at the same anatomical level in a 1-year-old boy (weight: 11 kg). Subjective image quality of lung and mediastinal images was rated as 2.8 and 2.3, respectively. Objective image noise was 7 HU
Discussion
This is the first study providing detailed information on image quality of chest CT examinations acquired at 70 kVp in pediatric populations. Our study design enabled us to acquire datasets at 70 kVp with a radiation dose equivalent to that delivered at 80 kVp., i.e. the current standard for infants and small children [17]. This was achieved after adjustment of the milliamperage by a factor of 1.6 for the 70-kVp protocols according the manufacturer’s recommendations and confirmed by calculation of the mean values of the CTDIvol and dose length product, which did not significantly differ between group 1 and group 2 examinations. This prerequisite fulfilled, the image quality of the 70-kVp images could then be compared to that of the reference standard, i.e. images acquired at 80 kVp in paired populations. We tested a noninferiority hypothesis, assuming that the image noise at 70 kVp would not differ by more than 10% when compared to that of the 80-kVp images. This hypothesis was verified because the difference of means of image noise between 70 kVp and 80 kVp examinations was −1.38 with an upper limit of the confidence interval lower than 0.77 (i.e. −2.59).
This allowed us to compare objective and subjective image noise between the two scanning protocols, keeping in mind that image noise is one of the most important factors determining image quality to make an accurate diagnosis [18]. Regarding objective image noise, it was found to be statistically significantly lower in 70 kVp images (i.e. group 1 examinations) than in 80 kVp images (i.e. group 2 examinations). When group 1 and group 2 patients were stratified according the children’s weight, reduction in image noise was statistically significant for children weighing less than 15 kg and close to statistical significance in children more than 15 kg. It is noteworthy that the mean noise level at 70 kVp in our study (i.e. 9.9 HU) is lower than that reported in the literature for 80 kVp examinations (mean image noise: 14.4 HU in children <15 kg and 12.3 HU in children 15.0–59.0 kg), a finding observed despite a lower radiation dose (20.5 mGy.cm vs. 98 mGy.cm) [19]. Regarding subjective image quality, we observed no statistically significant difference in the overall scores of image quality between groups 1 and 2, whether considering each group as a whole or stratifying them according to patient body weight. Group 1 and group 2 examinations were all rated as being of diagnostic image quality. The overall scores were established as mean values of lung and mediastinal scores. When mediastinal scores were specifically compared, image quality at 70 kVp did not significantly differ from that of images acquired at 80 kVp. Regarding lung images, lower scores of image quality were found at 70 kVp, a finding directly linked to results in group 1 children weighting >15 kg.
Several explanations can be proposed for this difference in image quality, which did not alter the diagnostic value of images, with a mean score of 1.65 in a scale ranging from 1 (excellent) to 4 (poor). The paired patient selection allowed us to match patients by body weight and age but without any possibility to take into account differences in the patients’ morphotype. Moreover, stored data of age and body weight were asymmetrically rounded. The paired patient choice based on body weight and age could have contributed to a bias in patient selection [20]. Last, one cannot exclude the influence of underlying disease in the assessment of subjective image quality analysis.
This study confirms that low-kVp protocols can be adapted to chest CT scanning of pediatric patients, providing diagnostic image quality not only for small children but also for children up to 40 kg. Our dosimetric results are below published values for dose estimates [9, 21], reinforcing the current recommendations for pediatric chest protocols to move from 120 kVp [1, 22] or 100 kVp [9] to 80 kVp or 70 kVp [23]. The low level of noise measured in group 1 examinations suggests the possibility of further decreasing the radiation dose with 70-kVp protocols. This scanning strategy would require the replacement of filtered-back projection, i.e. the standard mode for image reconstruction, by iterative reconstructions. This has recently been successfully applied to reduced-dose chest examinations by Lee et al. [24] and to pediatric cardiac CT examinations [25]. The second advantage of 70-kVp protocols could be found in contrast-enhanced chest CT examinations. This is due to the fact that the mean energy level of the X-ray beam at 70 kVp is closer to the k-edge of iodine, thus resulting in a higher attenuation of iodine than that observed at 80 kVp [26]. This improved vascular enhancement could help in the avoidance of re-imaging in infants and small children, a non-exceptional problem related to unfavorable contrast dynamics in these age categories and, in some cases, to impaired flow [27]. Owing to the chest morphology of children, the higher tube current necessary for 70-kVp examinations remains within the technical capabilities of the X-ray tube. Therefore, the integration of 70 kVp protocols for chest CT scanning in pediatric patients is technically feasible. Recent studies with phantoms suggest that the optimal tube voltage in children may be even lower (approximately 60 kVp) [1].
Our study has several limitations. First, it compared paired populations and not individuals scanned twice. Although theoretically possible, a study based on the latter option would have been more difficult to plan, requiring sequential examinations in children without changes over time in children’s body weight or characteristics of underlying diseases. Second, image analysis was obtained by consensus between two readers, precluding any evaluation of inter- and intra-observer agreement. However, this limitation was overcome by the inclusion of a third reader in cases of discordant ratings. Third, there was no specific evaluation of lesion conspicuity at 70 kVp. Because children were not paired according to the clinical indication for CT, this could not be integrated in the list of evaluated parameters.
Conclusion
This study demonstrates that it is possible to achieve similar image quality at 70 kVp to that obtained at 80 kVp in children.
References
Nievelstein RAJ, van Dam IM, van der Molen AJ (2010) Multidetector CT in children: current concepts and dose reduction strategies. Pediatr Radiol 40:1324–1344
Brenner D, Elliston C, Hall E et al (2001) Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 176:289–296
Hall EJ, Brenner DJ (2008) Cancer risks from diagnostic radiology. Br J Radiol 81:362–378
Euratom FP6 project: safety and efficacy in computed tomography (CT): a broad perspective (2005–2007) AZ: FP6/002388. http://cordis.europa.eu/fetch?CALLER=FP6_PROJ&ACTION=D&DOC=4&CAT=PROJ&QUERY=013543d2b76d:3023:226b4e6d&RCN=74114
Siegel MJ, Schmidt B, Bradley D et al (2004) Radiation dose and image quality in pediatric CT: effect of technical factors and phantom size and shape. Radiology 233:515–522
Herzog C, Mulvihill DM, Nguyen SA et al (2008) Pediatric cardiovascular CT angiography: radiation dose reduction using automatic anatomic tube current modulation. AJR Am J Roentgenol 190:1232–1240
Frush DP (2011) Radiation, thoracic imaging and children: radiation safety. Radiol Clin N Am 49:1053–1069
Singh S, Kalra MK, Moore MA et al (2009) Dose reduction and compliance with paediatric CT protocols adapted to patient size, clinical indication, and number of prior studies. Radiology 252:200–208
Kroft LJ, Roelofs JJ, Geleijns J (2010) Scan time and patient dose for thoracic imaging in neonates and small children using axial volumetric 320-detector row CT compared to helical 64-, 32-, and 16-detector row CT acquisitions. Pediatr Radiol 40:294–300
Schmidt B, Saba OI, Banckwitz R et al (2010) Assessment of a 70kV acquisition mode for pediatric CT scanning. Presented at: Radiological Society of North America 2010 Scientific Assembly and Annual Meeting, Chicago
Yu L, Li H, Fletcher JG et al (2010) Automatic selection of tube potential for radiation dose reduction in CT: a general strategy. Med Phys 37:234–243
Gnannt R, Winklehner A, Goetti R et al (2012) Low kilovoltage CT of the neck with 70 kVp: comparison with a standard protocol. AJNR Am J Neuroradiol 33:1014–1019
Santangelo T, Colas L, Niemann T et al (2013). Radiation dose levels in pediatric chest CT: experience in 506 children evaluated with dual-source CT (B0729). Insights Imaging 4(Suppl 1):145–384
Goo HW (2011) Individualized volume CT dose index determined by cross-sectional area and mean density of the body to achieve uniform image noise of contrast-enhanced pediatric chest CT obtained at variable kV levels and with combined tube current modulation. Pediatr Radiol 41:839–847
Bongartz G, Golding SJ, Jurik AG et al (2004) European guidelines for multislice computed tomography. Funded by the European Commission. Contract number FIGM-CT2000-20078-CT-TIP. March 2004. Available at www.msct.eu
Committee for Proprietary Medicinal Products (CPMP), European Agency for the Evaluation of Medicinal Products (EMEA) (2001) Points to consider on switching between superiority and noninferiority. Br J Clin Pharmacol 52:223–228
Lee T, Tsai IC, Fu YC et al (2006) Using multidetector-row CT in neonates with complex congenital heart disease to replace diagnostic cardiac catheterization for anatomical investigation: initial experiences in technical and clinical feasibility. Pediatr Radiol 36:1273–1282
Singh S, Kalra MK, Gilman MD et al (2011) Adaptive statistical reconstruction technique for radiation dose reduction in chest CT: a pilot study. Radiology 259:565–573
Kim JE, Newman B (2010) Evaluation of a radiation dose reduction strategy for pediatric chest CT. AJR Am J Roentgenol 194:1188–1193
Schneeweiss H, Komlos J, Ahmad AS (2010) Symmetric and asymmetric rounding: a review and some new results. Adv Stat Anal 94:227–247
Shrimpton PC, Hillier MC, Lewis MA et al (2006) National survey of dose from CT in the UK: 2003. Br J Radiol 79:968–980
Frush DP, Herlong JR (2005) Pediatric thoracic CT angiography. Pediatr Radiol 35:11–25
Yu L, Bruesewitz MR, Thomas KB et al (2011) Optimal tube potential for radiation dose reduction in pediatric CT: principles, clinical implementations, and pitfalls. Radiographics 31:835–848
Lee SH, Kim MJ, Yoon CS et al (2012) Radiation dose reduction with the adaptive statistical iterative reconstruction (ASIR) technique for chest CT in children: an intra-individual comparison. Eur J Radiol 81:934–938
Mieville FA, Gudinchet F, Rizzo E et al (2011) Paediatric cardiac CT examinations. Impact of the iterative reconstruction method ASIR on image quality: preliminary findings. Pediatr Radiol 41:1154–1164
Cardinal HN, Holdsworth DW, Drangova M et al (1993) Experimental and theoretical X-ray imaging performance comparison of iodine and lanthanide contrast agents. Med Phys 20:15–31
Paul JF, Rohnean A, Elfassy E et al (2011) Radiation dose for thoracic and coronary step-and-shoot CT using a 128-slice dual-source machine in infants and small children with congenital heart disease. Pediatr Radiol 41:244–249
Conflicts of interest
We acknowledge that Martine Remy-Jardin received research grants from Siemens Healthcare, Erlangen, Germany. Jacques Remy is a consultant for Siemens Healthcare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Niemann, T., Henry, S., Duhamel, A. et al. Pediatric chest CT at 70 kVp: a feasibility study in 129 children. Pediatr Radiol 44, 1347–1357 (2014). https://doi.org/10.1007/s00247-014-3027-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-014-3027-8