Abstract
Background
Wandering spleen is a rare condition in children that is often caused by loss or weakening of the splenic ligaments. Its clinical presentation is variable; 64% of children with wandering spleen have splenic torsion as a complication.
Objective
To provide up-to-date information on the diagnosis, clinical management and diagnostic imaging approaches for wandering spleen in infants and children and to underline the importance of color Doppler US and CT in providing important information for patient management.
Materials and methods
We report a series of three children with wandering spleen treated at our children’s hospital over the last 6 years. All three underwent clinical evaluation, color Doppler US and CT and were surgically treated. We also reviewed 40 articles that included 55 patients younger than 18 years reported in the Medline database from 2002 to 2012.
Results
We correlated pathological data with imaging findings. Color Doppler US, the first imaging modality in investigating abdominal symptoms in children with suspected wandering spleen, yielded a diagnostic sensitivity of 54.9%, whereas CT achieved about 71.7%.
Conclusion
Radiologic evaluation has a major role in confirming the diagnosis of a suspected wandering spleen and avoiding potentially life-threatening complications requiring immediate surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A wandering or ectopic spleen is a condition in which the spleen migrates from its normal anatomical location in the left upper quadrant to any other position in the abdomen or pelvis. It is caused by loss or weakening of the ligaments that usually hold the organ in its common location. The varied clinical presentations and nonspecific findings make radiologic evaluation essential to confirm the diagnosis, thus allowing immediate surgery to manage splenic torsion and its potentially life-threatening complications. Previous case reports and reviews on wandering spleen in children provide poorly detailed information on the diagnostic imaging workup.
We report a series of three children with wandering spleen treated at our hospital in the last 6 years. While seeking up-to-date information on diagnosis, clinical management and diagnostic imaging approaches in infants, children and adolescents we reviewed the literature. Here we summarize the imaging data from previous case reports and case series in patients younger than 18 years published from 2002 to 2012 [1–40]. We investigated the correlation between pathological data and imaging findings, and we present up-to-date information on how diagnostic imaging modalities can provide essential information in the planning of disease management and patient care.
Materials and methods
The institutional review board approved the study procedures, and we obtained informed consent from our patients before they were included in the study.
We reviewed the literature and analyzed the Medline database from 2002 to 2012, focusing on the radiologic findings in children (younger than 18 years at diagnosis) with wandering spleen. We only considered full-text articles in which children underwent color Doppler US or CT examination. We excluded from the review case reports and case series presenting only clinical findings or surgical therapy and those describing radiologic imaging (splenic position, size, imaging appearances, and parenchymal blood flow) in a confused manner.
Since 2007 three children admitted to our hospital were diagnosed as having wandering spleen. We reviewed their clinical reports. All three children’s diagnostic workup included color Doppler US and CT scan. Two children also underwent radiographic studies. In one child we used an IU22 real-time sonographic system (Philips Healthcare, Best, The Netherlands) and in the other two we used a Sonoline Antares US system (Siemens Medical Solutions, Issaquah, WA) for US examinations. Color Doppler US studies always began with a systematic overview using 1- to 6-MHz curvilinear transducers followed by more detailed imaging using 5- to 12-MHz linear transducers. In two children admitted from 2007 to 2009, CT scans were acquired with a Somatom Plus scanner (Siemens, Erlangen, Germany). The scanning parameters were 120 kVp and 40–120 mA. The protocol used a table of 4 mm/s with 4-mm collimation, and images were reconstructed at 2-mm intervals.
In the only child treated in 2012 we used a second-generation dual-source CT system (Somatom Definition Flash; Siemens, Forchheim, Germany) with two X-ray tubes and two detectors set at an angular offset of 95°. Each detector is equipped with 64 detector rows for data acquisition with a collimated slice width of 0.6 mm. Scan parameters were as follows: pitch = 2.7, slice acquisition 128 × 0.6 mm, and gantry rotation time 0.28 s, 50–100 mA at 100–120 kV. Images were reconstructed with a slice thickness of 1 mm.
The children were not sedated for the CT examination nor were they told how to breathe. Images were acquired in the cranio-caudal direction. In two children helical CT scans were acquired in the portal-venous phase; in one child CT images were acquired both in the hepatic arterial and portal venous phases.
Non-ionic, iodine-based contrast agents were used in all three children at a concentration of 300 mg iodine per ml. Contrast-agent dosing was determined by body weight (2 ml/kg body weight). The mean time elapsing between contrast agent injection and scanning was 45 s for infants and small children and 65 s for adolescents. For all these surgically treated patients we compared pathological data with imaging findings (Table 1).
Results
Our literature search retrieved 40 articles [1–40] reported during the last 10 years that included 55 children. Age ranged from 1 day to 18 years, mean age 8 years, with 30 males and 25 females. Of the 55 children, 51 underwent at least one color Doppler US examination. Color Doppler US correctly identified a wandering spleen or its association with splenic torsion in 28/51 cases (diagnostic sensitivity: 54.9%). In our literature review 39/55 children underwent at least one CT examination. In 28 of these 39 children CT correctly diagnosed wandering spleen (sensitivity 71.7%). Of the all children identified in our literature review, 35 were evaluated both by color Doppler US and CT. All children identified in our literature review and the three with wandering spleen we describe here were surgically treated.
Patient 1
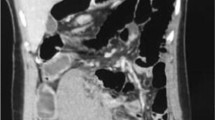
A 30-month-old girl was brought to the Emergency Department with a 3-day history of abdominal pain. Physical examination showed a tense abdomen with generalized pain. Laboratory tests showed an increased white blood cell count (18.8 × 103/μL). The diagnostic imaging workup began with a plain abdominal radiograph, which showed dilated bowel loops with no radiographic signs of intestinal obstruction. Color Doppler US showed no spleen in the left hypochondrium but an enlarged ectopic spleen located in the lower abdominal quadrants, characterized by a large hypoechoic intraparenchymal area altering the core structure and a small free-fluid collection in the peritoneal cavity. No vascular flow was visible in the splenic hilum or central region. Contrast-enhanced CT (DLP, 240 mGy/cm) confirmed the diagnosis of ectopic spleen with splenic vein thrombosis and a visible splenic artery. The splenic parenchyma contained a large non-enhancing central, hypodense area associated with splenic capsule hyperdensity relative to the splenic parenchyma. The pancreatic tail was displaced inferiorly, and next to the medial splenic border there was an area of heterogeneous attenuation characterized by alternating circular bands of radiodensity and radiolucency (Fig. 1). Urgent laparotomy showed a large and congested spleen with a 360° twist around its pedicle. Because the wandering spleen failed to regain its normal vascularity after detorsion, the girl underwent splenectomy. Histopathological examination demonstrated splenic necrosis and fibrosis.
Contrast-enhanced CT imaging in a 30-month-old girl with a 3-day history of abdominal pain (patient 1). Axial CT image obtained in the portal venous phase shows a large central hypodense area in the ectopic splenic parenchyma without contrast enhancement, with a rim sign–hyperdensity in the splenic capsule (white arrow)–strongly suggesting a parenchymal infarction and probably resulting from collateral circulation. The pancreatic tail was altered and displaced inferiorly and lies next to the dorsal–medial splenic border. The image shows an area of inhomogeneous attenuation characterized by alternating circular bands of radiodensity and radiolucency (whorl sign, black arrow)
Patient 2
A 12-year-old boy was brought to our Emergency Department with a 3-month history of recurrent abdominal pain. Physical findings included a tender, distended abdomen and a large, palpable, movable and hard woody mass in the pelvic region. Routine laboratory tests yielded reduced hematocrit values (31.6%; normal 36–49%) with decreased hemoglobin (11.1 g/dl; normal 13–16 g/dl), neutrophilia (87.5%; normal 39–59%), and reduced blood lymphocyte levels (6.9%; normal 26–48%).
Plain radiographs failed to show the spleen in its usual location and showed separated bowel loops (mass effect) in the mid-lower abdomen. Color Doppler US confirmed an abdomino-pelvic mass with apparent asplenia. The mass in the mesogastrium–left iliac fossa was the shape of a comma, suggesting an ectopic enlarged spleen. At the level of the inferior splenic pole, medially, color Doppler US showed a round lesion (9 cm in diameter) with a hypoechoic heterogeneous pattern relative to the normal splenic parenchyma; its inferior border reached the bladder dome, without evident infiltration. Color Doppler US examination demonstrated, within the mass, an anomalous cartwheel vascularization characterized by a main arterial supply and venous drainage with a radial pathway without sonographic signs of arterio-venous fistulas (Fig. 2). In the fasting state, artery waveforms demonstrated an arterial peak systolic value of 32 cm/s and a resistive index of 0.54. Venous flow velocity was uniform and the mean flow velocity was 13 cm/s; Doppler flow velocimetry yielded similar values in the mass and in the splenic parenchyma. Other findings were bilateral uretero-pyelic dilatation and a small fluid collection.
Transverse sonogram of the mesogastrium-left iliac fossa in a 12-year-old boy with a large palpable mass and a 3-month history of recurrent abdominal pain (patient 2). Color Doppler US shows a large round hypoechoic lesion medial to the inferior pole of the wandering spleen and exhibiting a radial, cartwheel-like vascular pattern
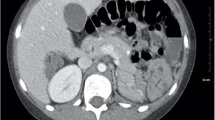
Contrast-enhanced CT images were acquired in the hepatic arterial and portal venous phases (DLP, 303 mGy/cm) and showed regularly opacified twisted vessels at the splenic hilum. The spleen appeared homogeneous except for a small hypoattenuating nodular area (14 mm in diameter) (Fig. 3). After contrast medium injection, CT scans in both phases showed a central radial hypodensity in the splenic mass (Fig. 4). Bowel loops were displaced and draped around the spleen, distal ureters were compressed and the bilateral upper urinary tract dilation was confirmed. The portal vein and spleno-portal confluence enhanced normally; the scan also visualized perigastric collateral veins. The pancreatic tail was located inferiorly and was intermingled with adipose tissue and the twisted splenic pedicle (Fig. 5). The boy underwent urgent laparoscopy, which showed an enlarged, bilobed spleen characterized by 360° torsion around its pedicle and without evidence of ligamentous attachments; the inferior portion, consisting of a large, round, tender mass, was excised (Fig. 6). Because surgical splenic pedicle detortion resulted in a normal-appearing spleen the boy underwent splenopexy with a retroperitoneal pouch. Pathological examination of the operative specimen disclosed a large splenic lymphangioma.
Axial contrast-enhanced CT in patient 2, a 12-year-old boy. In the portal-venous phase a small hypoattenuating nodular area is visible in the splenic parenchyma (arrow), suggesting a small pseudocyst, probably related to trauma or infarction
Contrast-enhanced CT in patient 2, a 12-year-old boy. Axial CT image in the portal-venous phase shows the splenic mass isoattenuating to the normal splenic tissue and shows a central radial hypodensity caused by dilated lymphatics; the right lower quadrant contains a small fluid collection
Axial contrast-enhanced CT in patient 2, a 12-year-old boy. Next to the medial border of the wandering spleen there is a twisted splenic pedicle intermingled with fat and ectopic pancreatic tissue displaced inferiorly (whorl sign, arrow); the image also shows bilateral upper urinary tract dilation
Intraoperative photograph in patient 2, a 12-year-old boy. The surgical specimen contains a long, torsed vascular splenic pedicle associated with a splenic mass, diagnosed at pathological examination as a lymphangioma
Patient 3
A 15-year-old boy was evaluated in the Cardiology Department during periodic controls because of aortic insufficiency after rheumatic cardiac disease; physical examination revealed an enlarged spleen with its inferior pole palpable 4–5 cm below the rib cage. Laboratory tests excluded infectious and hematological causes of splenomegaly. At abdominal sonography evaluation no spleen could be demonstrated in the normal position; an enlarged spleen with a granular and hypoechoic parenchyma could be seen extending from the medial margin of the left kidney to the pelvis; splenic borders were irregular and multilobed. At color Doppler US no demonstrable flow could be seen in the splenic vein at the hilum but several dilated, tortuous veins arose from the portal vein, suggesting cavernomatous splenic vein swapping (Fig. 7). US also showed a small perisplenic fluid collection. CT scan (DLP, 270 mGy/cm) corroborated the sonographic findings, confirming an enlarged wandering spleen that was inhomogeneous in density, without focal intraparenchymal lesions. The splenic vein was abruptly interrupted next to the spleno-portal confluence (Fig. 8) and collateral varicoid venous circles were seen at the splenic hilum, presumably representing cavernomatous swapping transformation involving the splenic vein (Fig. 9) associated with large perigastric collateral veins (Fig. 10). The splenic artery at the hilum was pervious although thinned. The pancreatic tail had shifted toward the spleen and appeared heterogeneously enhanced. One month later, an elective laparotomy confirmed splenic vein thrombosis accompanied by splenic cavernomatous changes in the wandering spleen and the boy underwent splenectomy. Histopathological examination showed a congested spleen with signs of venous thrombosis.
Transverse color Doppler US scan of the mesogastrium in a 15-year-old boy with an enlarged palpable spleen at physical examination (patient 3). US shows an enlarged, hypoechoic and ectopic spleen with irregular and multilobed borders; no flow was visible in the splenic vein at the splenic hilum but some dilated, tortuous veins arise from the portal vein (arrow), suggesting a cavernomatous splenic vein swapping
Contrast-enhanced CT in patient 3, a 15-year-old boy. This oblique multiplanar reconstruction image shows the splenic vein abruptly interrupted next to the spleno-portal confluence (arrow)
Contrast-enhanced CT in patient 3, a 15-year-old boy. Reconstructed coronal image shows an enlarged wandering spleen with inhomogeneous density. Collateral varicoid venous circles at the splenic hilum and in the left upper quadrant appear compatible with cavernomatous splenic vein swapping (arrowhead). The pancreatic tail is shifted toward the spleen and shows heterogeneous enhancement (long arrow)
Contrast-enhanced CT scan in patient 3, a 15-year-old boy. Axial view shows collateral varicoid venous circles near the splenic hilum associated with large perigastric collateral veins (arrow)
Discussion
Wandering spleen (ectopic, located in the lower abdomen) is an extremely rare condition in children, confirmed by the three children presented here, the only three cases of wandering spleen seen in our hospital over the last 6 years. These cases also support findings that children with wandering spleen are typically between 3 months and 10 years old, the most frequent age at presentation being younger than 1 year [41]. The gender distribution in our series agrees with the reported predominance of boys with wandering spleen [20]. Although this condition can be diagnosed at all ages, from childhood to adolescence, and in both genders, it is most often seen in women in the third decade of life [42]. Our review provided information on the causes and clinical presentation and emphasized the role of diagnostic imaging in finding a differential diagnosis, complications, and indications for surgery in children with wandering spleen.
Precisely what caused the spleen to migrate in our three patients remains conjectural. None of our young patients had the deficient anterior abdominal wall musculature typical in prune-belly syndrome [43] or a family history of wandering spleen [16]. Nor did they have specific clinical or laboratory findings to direct the diagnosis. Among the principal, normal anchoring structures, the gastrosplenic ligament attaches the spleen to the stomach, the phrenocolic ligament supports the inferior splenic pole and the lienorenal ligament fixes the spleen to the posterior abdominal wall. Congenital absence, abnormal development or acquired ligamentous laxity results in a hanging spleen that has a long vascular pedicle and migrates from its normally fixed location in the left upper quadrant. Although CT scans and color Doppler US cannot visualize these anatomical abnormalities they can disclose indirect signs, including a hanging or enlarged spleen and structural changes in the spleen [1, 41, 43, 44].
The three children we describe here and the case reports collected in our review all underline wandering spleen as a condition that has a variable clinical presentation. In all three children we treated routine laboratory tests yielded nonspecific findings. Diagnostic imaging therefore proved crucial in allowing an early diagnosis. None of our patients experienced complications related to torsion such as gangrene, abscess, local peritonitis, intestinal obstruction, variceal hemorrhage and necrosis involving the pancreatic tail [20]. Two children presented with abdominal pain and one with endocarditis. Only one had a palpable mass. Wandering spleen can be an incidental finding in asymptomatic patients (15%), or patients can present with abdominal pain (55%) or with a palpable mass (90%) [20]. Symptoms and signs may be silent for a long time (wandering spleen rarely leads to abnormal laboratory findings except for occasional pancytopenia caused by hypersplenism) [45], until complications arise related to torsion, splenic vascular pedicle torsion or abdominal organ compression. Torsion has been described in 64% of children with wandering spleen [20]; these patients sometimes have recurrent abdominal pain related to intermittent torsion and spontaneous detorsion caused by congestion. Patients with acute prolonged torsion and infarction that leads to marked congestion and capsular stretching frequently present with an acute abdomen. Some patients also present with associated symptoms such as nausea, vomiting, fever, peritoneal signs and leukocytosis [46].
All three children studied in our hospital underwent color Doppler US evaluation early in the diagnostic workup, and this imaging modality provided the definitive diagnosis. Color Doppler US is among the early imaging choices for evaluating the abdomen in children with abdominal pain or masses or both. In two children in our small series (patients 1 and 2) we first obtained plain films to exclude clinically suspected intestinal obstruction. At color Doppler US imaging we immediately suspected a wandering spleen because no spleen was visible in the left hypochondrium but an ectopic spleen-like mass could be seen in another abdominal site. The key practice point is to scan the child in various positions to demonstrate splenic mobility [47]. In all three children we describe the wandering spleen was enlarged. An enlarged wandering spleen is a typical imaging finding, perhaps reflecting chronic or recurrent torsion and subsequent venous congestion [23, 25]. In two children color Doppler US visualized a granular, hypoechoic splenic parenchyma. In one child color Doppler US identified a large, hypoechoic intraparenchymal area with an altered core structure, suggesting necrotic changes. In patient 1, the acute torsion made it impossible for color Doppler US to detect flow within the splenic parenchyma. In the third patient, no venous flow was visible at the splenic hilum but splenic hilar evaluation identified entangled vessels, suggesting a cavernomatous splenic vein transformation. In these two children the color Doppler US features strongly suggested splenic torsion.
In patient 2 color Doppler US also had to characterize the expansive lesion with a coarse echotexture identified in the lower splenic pole. This sonographic pattern has been reported in a single case of atypical splenic lymphangioma in a normally located spleen [48]. The sonographic radial vascular pattern identified in the splenic mass in patient 2 is unusual because lymphangiomas usually have no visible vascularity. These vascular appearances could suggest a benign splenic neoplasm of vascular origin, such as a hemangioma or hamartoma, but mainly in hemangioma color Doppler US shows an increased vessel density (more than five structures for cm2), whereas pulsed Doppler demonstrates a high flow velocity (up to 90 cm/s) and low resistive index with a broadened flow spectrum. In our case, color Doppler US showed a normal flow pattern around the dilated vessels.
Our literature review spanning 2002 to 2012 confirmed our original idea that although wandering spleen is a well-described clinical entity, apart from case reports and small series few publications have addressed imaging findings. In reviewing the literature we found it difficult to obtain all the information we needed given that the diagnostic procedures differed in the various studies and many procedures were not explained in sufficient detail, partly because most studies took a predominantly surgical viewpoint.
In our review sonographic data we considered diagnostically important were the spleen’s position in the abdomen (correct location vs. ectopic site), size, the splenic parenchymal echotexture (particularly any parenchymal structure inhomogeneity suggesting necrosis or infarction vs. a homogeneous splenic parenchyma) and, when reported, parenchymal blood flow, the color Doppler US appearances of the splenic vascular pedicle (pervious vs. thrombosed vs. torsed). When we assessed the possible correlation between each of these echo variables and splenic torsion to evaluate their diagnostic specificity, we found that color Doppler US proved to be a useful diagnostic tool, yielding 54.9% sensitivity. In four patients the imaging report described an ectopic spleen associated with splenomegaly but underestimated splenic pedicle torsion. In the most of the other false-negative cases the spleen was normally located in its usual site but slightly medially shifted. In three cases the ectopic spleen was sonographically described as an abdominal mass but diagnosed at surgery as torsed.
Although a complete color Doppler US report should describe in detail how the vascular splenic pedicle appears, our literature review found this information in only 21/51 children studied. Color Doppler US described absent or reduced arterial flow in 10 children; in 90% of them this sonographic feature was confirmed surgically (ectopic torsed spleen). In 2007 Soleimani et al. [42] described their experience with wandering spleen and reviewed the literature from 1895 to 2005 including five children in their small series. They recommended abdominal color Doppler US as a good tool for diagnosing a wandering spleen, achieving up to 52% accuracy [42].
Although in our experience color Doppler US proved useful for evaluating the spleen’s position and parenchymal blood flow, we agree with others who suggest complementing color Doppler US with CT, especially when torsion is suspected at clinical examination or early imaging [46, 49]. In all the three children with wandering spleen described here contrast-enhanced CT yielded direct and indirect findings indicating splenic pedicle torsion, confirming in two children splenic vein thrombosis, in one child associated with cavernomatous splenic vein swapping. In one child CT showed regularly opacified but twisted vessels at the splenic hilum. In two of the three children CT scan also identified collateral varicoid perigastric circulation along the great curvature of the stomach, arising from the chronic splenic volvulus. A volvulus is an unusual complication that requires urgent surgery because it can lead to life-threatening upper gastrointestinal hemorrhage [50]. The CT appearance of the splenic parenchyma differed remarkably in our three patients. In patient 1 CT showed a large central intraparenchymal hypodense area without contrast enhancement, with the rim sign—splenic capsule hyperdensity relative to the parenchyma—probably arising from collateral circulation and strongly suggesting parenchymal infarction. In patient 2, in whom we suspected a splenic mass, CT showed the wandering spleen to be homogeneous except for a small hypoattenuating nodular area possibly representing a small pseudocyst, probably caused by trauma or infarction (perfusion-metabolic alterations, probably related to intermittent splenic pedicle torsion). To better characterize the mass associated with the wandering spleen in this child, we used both an arterial and portal venous phase instead of the more commonly used split bolus. In both phases the splenic mass contained a central radial hypodensity, effectively excluding hemangioma and hamartoma. The differential diagnosis included hemo-lymphoid tumors and other neoplasms rare in children such as littoral cell angioma, hemangioendothelioma, hemangiopericytoma, angiosarcoma and lymphangiosarcoma. In patient 3—the one with splenic cavernomatous changes—we found an enlarged wandering spleen heterogeneous in density but without focal intraparenchymal lesions.
When our three patients first presented at the hospital they already had complications. On CT scan they all had the whorl sign strongly suggesting splenic pedicle torsion. In all of them, the pancreatic tail was displaced inferiorly, showed heterogeneous attenuation and was intermingled with adipose tissue and the twisted splenic pedicle.
In the diagnostic imaging workup in our three patients, and in accordance with our current practice, we did not use MRI nor did we use diffusion-weighted MRI, a promising diagnostic adjunct in patients with wandering spleen [51]. Although MRI might have provided useful information and could have replaced CT, when color Doppler US appearances caused us to suspect wandering spleen we needed urgent confirmation. Two patients referred by the Emergency Department underwent urgent radiologic examination so we had no time to arrange for the necessary MRI equipment and staff. We were unable to examine the spleen and its vessels with contrast-enhanced color Doppler US because this procedure is not approved in children in Italy.
Although we found in our literature review that MRI was used when feasible, CT diagnosed wandering spleen in 28 of the 39 children who underwent at least one CT examination (sensitivity 71.7%); in 17 of these children the spleen was torsed. In two patients CT exam was considered to be false-negative; in these cases CT scan correctly identified a wandering spleen but missed a splenic torsion, later discovered surgically [1, 12]. In three children [6, 12, 36] CT correctly showed signs suggesting a torsed wandering spleen, but the radiologists misinterpreted them (in two children they suspected an abdominal neoplastic mass and in one child an abdominal abscess). In our literature review we did not consider splenomegaly as a predictive, specific sign indicating splenic torsion at CT examination. The CT features considered highly suggestive of wandering spleen include the absence of the spleen in its normal location, a lower abdominal or pelvic mass with homogeneous or heterogeneous splenic parenchyma with attenuation values lower than those in normal splenic tissue, a whorled appearance in splenic vessels and surrounding fat, and sometimes ascites and necrosis involving the pancreatic tail [49].
In our review, the CT report described parenchymal structural features in the wandering spleen only in 24 of the children included. Of these 24 children, 19 had focal or diffuse abnormalities in splenic attenuation or both; 18/19 (94.7%) subsequently underwent splenectomy for ectopic, torsed spleen. The only discordance between diagnostic imaging data and histological results regarded a patient in whom color Doppler US disclosed diffuse hyperechoic abnormalities whereas CT scan visualized a completely fragmented splenic parenchyma [33]. Surgical examination disclosed only slight arteriolar intraparenchymal bleeding in a wandering spleen, so the child was successfully treated with massive arteriolar hemostasis and splenopexy.
Our retrospective review underlined the whorl sign as a very specific sign of splenic torsion; the correlation between the whorl sign and splenic vascular pedicle torsion achieves a predictive value of 100%, as Raissaki et al. [44] already noted. The whorl sign refers to twisted splenic pedicle intermingled with fat and ectopic pancreatic tissue, resulting in alternating circular radiodensity and radiolucency bands at post-contrast CT [42, 52]. This appearance reflects the normally developed dorsal pancreatic bud within the dorsal mesogastrium. If the dorsal mesogastrium is incomplete or fails to fuse with the parietal peritoneum, some pancreatic tail segments may become intraperitoneal—instead of retroperitoneal—and can therefore be involved in splenic torsion [44]. In a 12-year study characterizing CT findings, all the patients in whom wandering spleen was complicated by acute torsion had CT findings indicating torsion.
The diagnostic workup for wandering spleen in infants and children should whenever possible include color Doppler US followed by CT or MRI scan. In 10 of the 35 children in our review who underwent both imaging modalities, color Doppler US failed to diagnose wandering spleen but CT correctly identified it. Hence CT seems far more sensitive than color Doppler US in detecting and characterizing this condition. In their review of the literature, Brown et al. [39] calculated that when CT was used it was diagnostic in 79% of the patients and showed an abdominal mass in 14%.
In our small series of children with wandering spleen the diagnostic imaging workup disclosed two extremely rare entities so far unreported in children. A lymphangioma, as described in patient 2, is a distinctly unusual finding in a wandering spleen. The literature includes only one case, in a young woman after pregnancy [53], but the echographic macrocystic pattern in her case distinctly differed from the color Doppler US findings in our patient’s mass [54]. Previous literature reports describe a wandering spleen associated with a true mass (epidermoid cysts, simple cysts, pseudocysts, lymphomas and inflammatory pseudotumors) [53]. An equally unusual imaging finding in one of our children, patient 3, was the collateral varicoid venous circles at the splenic hilum, such as cavernomatous splenic vein swapping, suggesting chronic splenic torsion.
Surgery, splenectomy and splenopexy are the only treatment options in children with wandering spleen. Because increasing evidence underlines the major role of the spleen in the reticulo-endothelial system, and concern exists about the risk of post-splenectomy sepsis, most surgeons prefer to maintain the organ with splenopexy except in patients with massive splenic infarction or splenic vessel thrombosis [16, 40]. Underlining the rarity of wandering spleen, a torsed wandering spleen is diagnosed in about 0.2–0.3% of overall patients who require splenectomy [46].
Conclusion
Our study confirms how important diagnostic imaging is in identifying a wandering spleen before life-threatening complications develop. The best imaging modalities for correctly localizing the ectopic spleen and demonstrating its vascularity and viability are color Doppler US and CT.
The first-line imaging modality for investigating abdominal disease in children is usually color Doppler US but CT scan is extremely useful for diagnosing this condition early, especially when clinical investigation or imaging studies imply splenic torsion.
A reasonable surgical option, especially in children without massive infarction and thrombosis, is detorsion and splenopexy.
References
Ayaz UY, Dilli A, Ayaz S et al (2012) Wandering spleen in a child with symptoms of acute abdomen: ultrasonographic diagnosis. Case report. Med Ultrason 14:64–66
Cripps M, Svahn J (2011) Video. Hand-assisted laparoscopy for wandering spleen. Surg Endosc 25:312
Magno S, Nanni L, Retrosi G et al (2011) An unusual case of acute pancreatitis and gastric outlet obstruction associated with wandering spleen treated by laparoscopic splenopexy. J Laparoendosc Adv Surg Tech A 21:467–470
Chu J, Li Z, Luo B et al (2011) Wandering spleen with torsion and complete infarction. Acta Radiol 52:911–913
Arleo EK, Kovanlikaya A, Mennitt K et al (2010) Multimodality imaging of a neonatal wandering spleen. Clin Imaging 34:302–305
Saouab R, Dafiri R (2010) Post-traumatic acute abdominal pain. Br J Radiol 83:804–806
Maschio M, Cozzi G, Sanabor D et al (2010) Splenomegaly as presentation of a wandering spleen. J Pediatr 157:859
Ozakaki T, Ohata R, Miyano G et al (2010) Laparoscopic splenopexy and gastropexy for wandering spleen associated with gastric volvulus. Pediatr Surg Int 26:1053–1055
Fiquet-Francois C, Belouadah M, Ludot H et al (2010) Wandering spleen in children: multicenter retrospective study. J Pediatr Surg 45:1519–1524
Dillman JR, Strouse PJ (2010) The “wandering” spleen. Pediatr Radiol 40:231
Sanchez R, Lobert P, Herman R et al (2010) Wandering spleen causing gastric outlet obstruction and pancreatitis. Pediatr Radiol 40:S89–S91
Di Crosta I, Inserra A, Gil CP et al (2009) Abdominal pain and wandering spleen in young children: the importance of an early diagnosis. J Pediatr Surg 44:1446–1449
Lien CH, Lee HC, Yeung CY et al (2009) Acute torsion of wandering spleen: report of one case. Pediatr Neonatol 50:177–180
Feroci F, Miranda E, Moraldi L et al (2008) The torsion of a wandering pelvic spleen: a case report. Cases J 1:149
Sodhi KS, Gupta P, Rao KL et al (2008) Marfanoid hypermobility syndrome and skeletal abnormalities in a rare case of torsion of wandering spleen. Br J Radiol 81:145–148
Ben Ely A, Seguier E, Lotan G et al (2008) Familial wandering spleen: a first instance. J Pediatr Surg 43:23–25
Choh SA, Naseer AC, Dar I et al (2008) Wandering spleen presenting as recurrent abdominal pain in a young female. Indian J Pediatr 75:1181–1182
Upadhyaya P, St Peter SD, Holcomb GW 3rd (2007) Laparoscopic splenopexy and cystectomy for an enlarged wandering spleen and splenic cyst. J Pediatr Surg 42:23–27
Gayer G (2002) Torsion of a wandering spleen. Isr Med Assoc J 4:658–659
Liu HM, Lau KK (2007) Wandering spleen: an unusual association with gastric volvulus. AJR Am J Roentgenol 188:328–330
Lacreuse I, Moog R, Kauffmann I et al (2007) Laparoscopic splenopexy for a wandering spleen in a child. J Laparoendosc Adv Surg Tech A 17:255–257
Kleiner O, Newman N, Cohen Z (2006) Pediatric wandering spleen successfully treated by laparoscopic splenopexy. J Laparoendosc Adv Surg Tech 16:328–330
Takayasu H, Ishimaru Y, Tahara K et al (2006) Splenic autotransplantation for a congested and enlarged wandering spleen with torsion: report of a case. Surg Today 36:1094–1097
Lopez-Tomassetti FE, Artega GI, Martín MA et al (2006) An unusual case of hemoperitoneum owing to acute splenic torsion in a child with immunoglobulin deficiency. J Postgrad Med 52:41–42
Karmazyn B, Steinberg R, Gayer G et al (2005) Wandering spleen: the challenge of ultrasound diagnosis: report of 7 cases. J Clin Ultrasound 33:433–438
Esposito C, Settimi A, Centonze A et al (2005) Enlarged wandering spleen treated with hemisplenectomy and fixation of the residual spleen. Pediatr Surg Int 21:488–490
Schaarschmidt K, Lempe M, Kolberg-Schwerdt A et al (2005) The technique of laparoscopic retroperitoneal splenopexy for symptomatic wandering spleen in childhood. J Pediatr Surg 40:575–577
Saxena AK, Van Tuil C, Groszek-Terwei I et al (2005) Torsion of a wandering spleen with stomach volvulus and nonrotation: extraperitoneal pocket splenopexy. Surgery 137:265
Mcheik JN, Richer JP, Levard G (2005) Torsion of the spleen in children. Arch Pediatr 12:1496–1499
Martínez-Ferro M, Elmo G, Laje P (2005) Laparoscopic pocket splenopexy for wandering spleen. A case report. J Pediatr Surg 40:882–884
Hedeshian MH, Hirsh MP, Danielson PD (2005) Laparoscopic splenopexy of a pediatric wandering spleen by creation of a retroperitoneal pocket. J Laparoendosc Adv Surg Tech 15:670–672
Tucker ON, Smith J, Fenlon HM et al (2004) Recurrent torsion of a wandering spleen. Am J Surg 188:96–97
Balliu PR, Bregante J, Pérez-Velasco MC et al (2004) Splenic haemorrhage in a newborn as the first manifestation of wandering spleen syndrome. J Pediatr Surg 39:240–242
Ajello A, Minniti A, Malatesta A et al (2004) The wandering spleen: something to bear in mind in the presence of a mobile abdominal mass. Eur J Pediatr 163:277–278
Qazi A, Awadalla S (2004) Wandering spleen: a rare cause of mesenteroaxial gastric volvulus. Pediatr Surg Int 20:878–880
Kim SC, Kim DY, Kim IK (2003) Avulsion of wandering spleen after traumatic torsion. J Pediatr Surg 38:622–623
Kessler A, Miller E, Keidar S et al (2003) Mass at the splenic hilum. J Ultrasound Med 22:527–530
Romero JR, Barksdale EM (2003) Wandering spleen: a rare cause of abdominal pain. Pediatr Emerg Care 19:412–414
Brown CV, Virgilio GR, Vazquez WD (2003) Wandering spleen and its complications in children: a case series and review of the literature. J Pediatr Surg 38:1676–1679
Steinberg R, Karmazyn B, Dlugy E et al (2002) Clinical presentation of wandering spleen. J Pediatr Surg 37:30
Herman TE, Siegel MJ (1991) CT of acute splenic torsion in children with wandering spleen. AJR Am J Roentgenol 156:151–153
Soleimani M, Mehrabi A, Kashfi A et al (2007) Surgical treatment of patients with wandering spleen: report of six cases with a review of the literature. Surg Today 37:261–269
Paterson A, Frush DP, Donnelly LF et al (1999) A pattern-oriented approach to splenic imaging in infants and children. Radiographics 19:1465–1485
Raissaki M, Prassopoulos P, Daskalogiannaki M et al (1998) Acute abdomen due to torsion of wandering spleen: CT diagnosis. Eur Radiol 8:1409–1412
Misawa T, Yoshida K, Shiba H et al (2008) Wandering spleen with chronic torsion. Am J Surg 195:504–505
Sodhi KS, Saggar K, Sood BP et al (2003) Torsion of a wandering spleen: acute abdominal presentation. J Emerg Med 25:133–137
Taori K, Sanyal R, Deshmukh A et al (2005) Pseudocyst formation: a rare complication of wandering spleen. Br J Radiol 78:1050–1052
Komatsuda T, Ishida H, Konno K et al (1999) Splenic lymphangioma: US and CT diagnosis and clinical manifestations. Abdom Imaging 24:414–417
Fonseca AZ, Ribeiro M, Contrucci O (2013) Torsion of a wandering spleen treated with partial splenectomy and splenopexy. J Emerg Med 44:33–36
Singla V, Galwa RP, Khandelwal N et al (2008) Wandering spleen presenting as bleeding gastric varices. Am J Emerg Med 26:637
Buckley O, Ward EVM, Doody O et al (2007) MRI of the wandering spleen. Clin Radiol 62:504
Sheflin JR, Lee CM, Kretchmar KA (1984) Torsion of wandering spleen and distal pancreas. AJR Am J Roentgenol 142:100–101
Alerci M, Dore R (1990) Computed tomography of cystic lymphangioma in a wandering spleen. Acta Radiol 31:589–590
Octavio S, de Toledo L, Cozcolluela Cabrejas R et al (2006) Wandering spleen associated to inflammatory pseudotumor. Radiologia 48:173–176
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lombardi, R., Menchini, L., Corneli, T. et al. Wandering spleen in children: a report of 3 cases and a brief literature review underlining the importance of diagnostic imaging. Pediatr Radiol 44, 279–288 (2014). https://doi.org/10.1007/s00247-013-2851-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2851-6