Abstract
Background
Spinal fractures are uncommon manifestations of child abuse and elimination of the lateral views of the spine from the initial skeletal survey protocol has been recommended.
Objective
To establish the prevalence of spinal fractures detected on skeletal surveys performed for suspected child abuse and their association with intracranial injury (ICI).
Materials and methods
The ACR standardized skeletal surveys and neuroimaging studies of 751 children (ages 0–4 years) were reviewed. A positive skeletal survey was defined as having one or more clinically unsuspected fractures.
Results
Fourteen children had a total of 22 definite spinal fractures. This constituted 1.9% (14/751) of the total cohort, and 9.7% (14/145) of children with a positive skeletal survey. Advanced imaging confirmed the fractures in 13 of the 14 children and demonstrated 12 additional spinal fractures. In five cases, spinal fractures were the only positive skeletal findings. In 71% (10/14) of the children, the spinal fractures were accompanied by ICI. Children with spinal fractures were at significantly greater risk for ICI than those without spinal injury (P < 0.05).
Conclusion
Spinal fractures are not rare in children with positive skeletal surveys performed for suspected abuse and they may be the only indication of skeletal trauma. There is an association between spinal fractures and ICI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spinal fractures are considered to be uncommon manifestations of child abuse [1–10]. They are usually “silent” and can be missed unless appropriate skeletal imaging is performed [11]. In a comprehensive review, Kemp et al. [12] found that spinal fractures are important indicators of abuse in infants and young children. The actual prevalence of spinal involvement in abused children is difficult to determine. In large series, figures range from 0% to 3% [1–5, 7, 8]. Karmazyn et al. [9] found that 0.3% (3/930) of skeletal surveys revealed spinal fracture. Jha et al. [13] found only 1 compression spinal fracture in 530 skeletal surveys. Based on this low prevalence, elimination of the lateral views of the spine from the initial skeletal survey protocol has been suggested [9, 13]. In a multicenter retrospective review of the data from 2,049 initial skeletal surveys in children younger than 10 years, Lindberg et al. [14] found that 16 children (0.8%) had spinal fractures. Kleinman et al. [10] found that 2.7% (10/635) of skeletal surveys in the film/screen era in children younger than 2 years of age had spinal fractures. Their prevalence rose to 10.2% (10/98) when only surveys with >1 fracture were considered [10] and the authors concluded that eliminating lateral views of the spine from the skeletal survey protocol could lead to missing important injuries [10, 14].
The high prevalence of other skeletal and extraskeletal injuries in children with abusive spinal fractures has been well-documented [8, 10, 11]. Furthermore, several authors have noted the presence of spinal injuries in children with abusive head trauma. Seven of the 25 children in Kemp et al.’s [12] review and two of the three cases in Karmazyn et al.’s [9] paper also had abusive head trauma. The purpose of our study was to evaluate the prevalence of spinal fractures detected on the skeletal surveys performed for suspected child abuse and to determine the correlation between spinal fracture and intracranial injury.
Materials and methods
This retrospective study was approved by the institutional review board and was compliant with HIPAA guidelines. We carried out a search of the radiology procedures database for skeletal surveys performed for suspected child abuse at a large urban children’s hospital from July 2005 to January 2013. A total of 775 children were identified during this time period. Based upon the general view that skeletal surveys in older children have a low yield and that these studies in this population are infrequently performed in our institution, children older than 4 years of age were excluded (n = 15) [5, 15]. Also, children with probable or confirmed metabolic bone disease or genetic disorder were excluded (n = 9). For the remaining 751 cases, the imaging studies, radiology reports and medical records were reviewed. Follow-up skeletal surveys were performed in 17% (128/751) of the cases. Although no strict selection protocol was used, we generally followed the recommendations of the American Academy of Pediatrics to repeat the survey at approximately 2 weeks when abnormal or equivocal findings are found on the initial study and/or when abuse remains suspected on clinical grounds [16]. The skeletal surveys were performed according to American College of Radiology (ACR) guidelines using a high-resolution (50 μm resolution) computed radiographic (CR) system for infants (<1 year old) and a standard CR system (100 μm) for older children [17]. Images were reviewed on a high-resolution PACS workstation by a pediatric radiologist with 5 years of experience and compared with the radiology reports. Fractures were classified as “definite” or “possible” based on the radiographic features. Discordant assessments were resolved by consensus with one of two other pediatric radiologists with 10 years and 35 years of experience, respectively. The definite and possible fractures were tabulated for the initial and follow-up studies and entered into a skeletal survey data entry module developed in Oracle 11 (Oracle, Redwood Shores, CA). A summary of the skeletal injuries was created by combining the findings of the initial and follow-up skeletal survey. Given the uncertainties in dating spinal fractures radiographically, injuries were all classified as “indeterminate” with reference to age.
A skeletal survey was defined as positive when it showed at least one definite fracture that was clinically unsuspected [18]. Skeletal surveys in which incidentally discovered rib fractures were an indication for the skeletal survey (n = 21) were also considered positive. The medical records of children with fractures of the spine were reviewed by a child abuse pediatrician to identify the indication for the skeletal survey, to determine if a report of suspected abuse was filed with child protective services and if the report was substantiated.
Sixty-six percent (495/751) of the children had cranial CT and/or MRI studies; the reports were reviewed and the presence and characteristics of intracranial abnormalities were recorded. A pediatric neuroradiologist with 15 years of experience reviewed the neuroimaging studies of children with spinal fracture. All of the children with skeletal survey and neuroimaging studies (n = 495) were included in a subcohort that included all children with spinal fracture. Intracranial injury and spinal fracture were compared as dichotomous variables in this group. Fisher exact test was used to test significance of injury correlations in contingency tables and odds ratios were also calculated. Statistical significance was defined by a p-value < 0.05. Statistical analyses were performed using IBM SPSS 21 (SPSS, Chicago, IL).
Results
Subjects and clinical indications
The mean age of the 751 children in the cohort was 10 months (range: 4 days−4 years); 75% (567/751) were infants (<1 year), 14% (108/751) were 1 to 2 years and 10% (76/751) were >2 years. There were 440 boys and 311 girls. Fourteen children with definite spinal fractures were identified with a mean age of 16 months (range: 2–39 months). The results for these children are summarized in Table 1. Clinical indication for the skeletal survey in our 14 cases included suspected abusive head trauma in 3 children (cases 1, 4 and 12), incidental rib fractures in 2 (cases 2 and 9), bruises in 5 (cases 3, 5, 6, 8 and 13) and long bone fractures in 3 (cases 7, 10 and 11). In case 14, concern for abuse was based on the presence of intracranial injury (ICI) and bruises after an unwitnessed fall.
Skeletal survey findings
Nineteen percent (145/751) of the children had a positive skeletal survey, with a higher prevalence in children <24 months compared to those >24 months (20% vs. 10%) (Table 2). The prevalence of definite spinal fracture was 1.9% (14/751) in the entire cohort, and 9.7% (14/145) of children with a positive skeletal survey only. Children older than 24 months had a higher prevalence of spinal fractures than children <24 months (5.3% vs. 1.5%) (Table 2), but statistical analysis was not performed because of our unbalanced age groups (675 vs. 76).
Seven children had definite radiographic evidence of spinal injury at multiple levels, with a total of 22 definite fractures. Initial skeletal survey demonstrated 20 definite and 12 possible fractures. Follow-up skeletal survey was obtained in four children, and two of the possible spinal fractures were considerate definite. At least one of the spinal fractures was visible on the frontal projection in 64% (9/14) of the children (Fig. 1). In 36% (5/14) of the children and in 45% (10/22) of the definite spinal fractures, the injury was demonstrated only on the lateral projection of the spine (Fig. 2). When the injuries were evident on the frontal projection, the fractures were generally less conspicuous than on the lateral view (Fig. 1). In one case, a solitary fracture was evident only on the frontal projection (Fig. 3). We identified four lumbar fractures in two children (cases 8 and 10) and two sacral fractures in two children (cases 9 and 11) that were only evident on the dedicated lateral view of the sacrum and lumbar spine (Fig. 4).
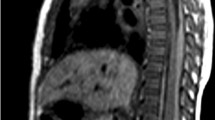
Two-year-old girl (case 13) with multiple contiguous vertebral body compression fractures visible on frontal and lateral views. Frontal (a) and lateral (b) views of the thorax from the skeletal survey demonstrate vertebral body compression fractures involving T5 and T6 (long arrows). Spinal injuries are better visualized on the lateral projection, where “possible” T4 and T7 vertebral body compression fractures are also visualized (short arrows in b). The only other osseous injury was a subtle left 7th costochondral junction rib fracture that was evident on the frontal view of the thorax but was initially overlooked (short arrow in a). c Sagittal T2-weighted MR image of the spine confirms the presence of compression fractures involving the vertebral bodies from T4 through T7 (long arrows), and an additional signal abnormality at the T3 vertebral body (short arrow) suggesting compression fracture
A 2-year-old boy (case 4) with multiple contiguous and non-contiguous vertebral body compression fractures. a No fractures were evident on the anterior view of the thorax. b The lateral view of the thorax demonstrates a definite compression deformity of the T4 vertebral body (long arrow) and a possible superior plate compression fracture of the T9 vertebrae (short arrow). c Sagittal reformat from the abdominal CT performed to rule out abdominal visceral injury confirmed the T9 vertebrae compression fracture (upper arrow) and demonstrates an additional T10 superior endplate irregularity suggesting compression fracture (lower arrow). d Posterior maximum intensity projection image from the subsequent 18 F-NaF PET bone scan shows increased tracer uptake in the T4, T9 and T10 vertebra and focal uptake in both distal fibular diaphyses (arrows) corresponding to bilateral diaphyseal fibular healing fractures evident on the skeletal survey (not shown)
A 3-year-old boy (case 3) with a solitary vertebral body compression fracture visible only on the frontal radiograph. a Frontal view of the thorax from the skeletal survey demonstrates subtle loss of height along the left lateral aspect of T7 (arrow). b The lateral radiograph is unremarkable. c, d Posterior and lateral maximum intensity projections from the 18 F-NaF PET bone scan show corresponding increased tracer uptake at the fracture site (arrows), but no other skeletal injuries
An 8-month-old girl (case 8) with lumbar and lower thoracic vertebral body compression fractures. a Frontal view of the abdomen from the skeletal survey shows no injuries. b Lateral view of the lumbar spine demonstrates compression fractures of the L3 and L4 vertebral bodies (long arrows), and “possible” superior plate vertebral compression fractures from T12 to L2 (short arrows). c Sagittal reformat from the abdominal CT confirms multiple contiguous compression vertebral body fractures from T12 to L4 (short arrows, T12 to L2; long arrows, L3 and L4). Left lobe liver laceration and peritoneal free fluid were also present (not shown)
Additional skeletal injuries were identified in 64% (9/14) of the children; three had rib fractures and classic metaphyseal lesions (CML), four had long bone fractures, one had two CMLs and one had an isolated costochondral rib fracture (Fig. 1). Including case 10, in which the femur fracture initiated the request for a skeletal survey, spinal fractures were the only finding found on skeletal survey in 36% (5/14) of the children. The spinal fractures were not evident clinically in all the cases, including the child with the T12 fracture dislocation (case 9).
Additional imaging
Additional imaging confirmed the spinal fractures in 13 children; 18 F-NaF PET in 7, conventional technetium 99 m methylene diphosphonate scintigraphy in 1, CT in 5 and MR in 5. These studies detected 12 new definite spinal fractures. In five children (cases 4, 8, 9, 12 and 13), additional imaging confirmed eight “possible” fractures that were appreciable only on the lateral projection of the spine, and in three children (cases 4, 12 and 14), CT or MR revealed four additional compression spinal fractures not detected on the skeletal survey. Overall, 34 spinal fractures were included in our imaging analysis.
Characteristics of spine fractures
Injury levels ranged from C4-S3. One fracture involved the cervical spine, 25 injuries involved the thoracic spine, 6 involved the lumbar spine and 2 involved the sacrum. The thoracolumbar spine fractures were all vertebral body compression type, except in a child with a T12 fracture dislocation (case 9), a case which has been reported previously [19]. Isolated compression-type thoracic vertebral body fractures were noted in four children (cases 1, 3, 5 and 7) (Fig. 3). There were multiple contiguous thoracic or thoracolumbar compression fractures in six cases (cases 2, 8, 10, 12, 13 and 14) (Fig. 1), multiple non-contiguous vertebral body injuries in two children (cases 6 and 9) (Fig. 5), a combination of contiguous and non-contiguous injuries in one case (case 4) (Fig. 2), and one case of isolated sacral injury (case 11).
An 8-week-old girl (case 6) with non-contiguous vertebral body compression fractures. a Frontal view of the thorax from the skeletal survey reveals compression deformity of the body of the T10 vertebrae (arrow). b The lateral view better demonstrates the same injury (long arrow) and depicts an additional subtle T3 body compression fracture (short arrow). c Sagittal T2-weighted MR image confirms both spinal body compression fractures (arrows). d Posterior MIP image from the subsequent 18 F-NaF PET bone scan shows increased tracer accumulation in the T10 vertebrae, but no abnormal uptake at T3. No other skeletal injuries are demonstrated
Neuroimaging
Neuroimaging results are summarized in Table 1. All of the children with spinal injury had imaging of the brain. In 71% (10/14), the spinal fractures were accompanied by ICI. Whole-spine MR was performed in four cases (cases 6, 9, 13 and 14), demonstrating the vertebral fractures and absence of spinal cord involvement in all cases. Spinal subdural hematomas were observed in two children within the thoracic (case 9) and lumbar and sacral regions (case 13). In addition, a cervical spinal SDH was partially demonstrated in the sagittal T1-weighted image of the brain MR in case 5.
When results of children with neuroimaging (n = 495) were analyzed, we found that 159 of the 481 children (33%) with no spine fracture had associated intracranial injury. This compared with 10 instances of intracranial injury in the 14 children (71%) with spinal injury (P < 0.05). Children with spinal fractures were at significantly greater risk for intracranial injury than those without spinal injury (odds ratio 5; 95% confidence interval 1.6–16.4). This increased risk was also present for only those children with a positive skeletal survey and imaging of the brain (n=122); 33 % (36/108) vs. 71 % (10/14) (P < 0.05, odds ratio 5.5; 95 % confidence interval 1.6–18.8).
Clinical outcome
All 14 children with spinal injury had other clinical, neuroimaging or skeletal findings concerning for abuse. In all 14 cases, a mandated report was filed with child protective services and further investigation supported the finding of child abuse in 13 cases, resulting in civil actions to ensure their safety of the child; one of the children died shortly after diagnosis due to traumatic brain injury (case 12).
Discussion
There is a rich literature describing a wide variety of spinal injuries in abused children dating to Astley’s [20] 1953 case report of a “crumpled” vertebral body fracture in a 32-month-old child with multiple other inflicted injuries. Numerous reports of abusive spinal injuries followed, and in 1997 the ACR recommended that skeletal surveys for suspected child abuse include dedicated frontal and lateral views of the cervical, thoracic and lumbosacral spine [17]. A review of the implementation of this standard in the US found that nearly all facilities (98.1%) imaged the spine in the lateral projection [21]. With these advances in comprehensive skeletal imaging practices for suspected abuse, some recent research has been directed toward modification of the filming protocol to optimize detection, and where possible, reduce unnecessary radiation exposure. Karmazyn and others [22] demonstrated an increased yield of skeletal surveys with the inclusion of lateral views of the extremities, supplementing the ACR protocol with eight additional exposures. Other studies have suggested that elimination of the lateral spine views on the follow-up skeletal survey can reduce radiation exposure without compromising the ability to obtain important diagnostic information [23, 24].
The reported low prevalence of vertebral injuries in child abuse has also prompted some to consider eliminating lateral views of the spine from the standard initial skeletal survey protocol. In the largest single institutional study to date on skeletal injuries in suspected abuse, Karmazyn et al. [9] reviewed the reports of skeletal surveys of 930 children younger than 2 years of age and found 0.3% (3/930) of children had vertebral compression fractures. Jha and colleagues [13] reviewed the reports of 530 skeletal surveys and found only 1 case of thoracic spinal compression fracture. In a retrospective multicenter review of the data from 2,049 initial skeletal surveys in children younger than 10 years, Lindberg et al. [14] found that 16 children (0.8%) had spinal fractures and 3.4% (16/471) of the children with a positive skeletal survey had spinal fractures.
In contrast, Kleinman and colleagues [10] recently reported a historical review of the film/screen skeletal surveys performed at the University of Massachusetts Medical Center in Worcester on 365 children <2 years old and found 25 spine fractures in 2.7% (10/365) of cases. Our 1.9% prevalence of spinal injuries, drawn from another New England city, is more in accord with their data and supports the conclusion that, although spinal fractures are uncommonly encountered in abused children, they are not rare. Importantly, when only children with positive skeletal surveys are considered, our prevalence rose substantially to 9.7%, a figure quite similar to Kleinman’s prevalence of 10.2% of skeletal surveys with >1 fracture [10, 14]. Our higher prevalence of several earlier studies could, in part, be related to the fact that we included older children in our cohort (up to 4 years). We noted a significant difference in the prevalence of spinal fractures between children younger than 2 years and those older than 2 years of age. A similar finding is also evident in the 20-center study data of Lindberg et al. [14]. Among their children with positive skeletal surveys, 2.6% (10/417) of patients younger than 24 months had a spinal fracture, and 11% (6/54) of patients older than 24 months had a spinal fracture. This finding has potential implications for skeletal survey screening of children beyond infancy.
Our results support the value of the lateral view in the radiographic evaluation of the spine. The study design did not permit a statistical analysis of the separate yields of the frontal and lateral radiographs since, in some cases, the fracture was inconspicuous on the frontal view and noted only after the finding was detected on the lateral projection. In such cases, the injury would probably have been missed without the two-view examination.
Our review did not include children with possible or definite spinal injury described on scintigraphy or cross-sectional imaging, if it was not evident on the skeletal survey. It is generally acknowledged that radiographs tend to underestimate the number of vertebral injuries, and this was confirmed by documentation of 12 new fractures in the 13 children who had additional imaging. Bone scintigraphy, CT and MRI increase the yield and heighten diagnostic confidence in the detection of spinal injuries [25]. We rarely perform CT for simple vertebral body compression deformities, but we do carefully scrutinize the spine on appropriate reformats from abdominal and chest CTs obtained for assessment of visceral injuries. We do commonly use radionuclide bone scans to supplement radiography and 18 F-NaF PET is particularly well-suited to this application since it delivers a comparable dose, but superior image contrast and spatial resolution compared to technetium 99 m based bone scintigraphy [24]. In their case series from our institution, Drubach et al. [25] included a case of a 10-month-old boy with three mid-thoracic vertebral compression fractures that were detected on 18 F-NaF PET imaging, but were not visible on baseline or follow-up skeletal survey. The fractures were subsequently confirmed with MRI. This child was imaged at our institution during the study time frame, but since the spinal fractures were not evident radiographically, the skeletal survey was considered negative with respect to the spinal injury. Therefore, the frequency of spinal injuries in our cohort is actually greater than our results indicate, but the true prevalence cannot be estimated since advanced spinal imaging was only performed in a small minority of our study group.
Although solitary vertebral compression fractures were present in five cases, our data demonstrate a higher prevalence of both multiple contiguous and non-contiguous injuries. Studies based on accidental trauma in children have considered that contiguous compression fractures are a common feature of pediatric spinal injury [26, 27]. Increased mobility of the child’s spine when compared to adults allows for dissipation of applied forces over a greater number of spinal segments, minimizing the incidence of burst fractures and neurological injury [27]. Non-contiguous spinal injuries have been described in up to 6% of children with accidental spinal trauma [28], and this pattern had also been noted with abusive injury [29]. In our case with the fracture-dislocation of T12 (case 9), the highest injury was at C4 and the lowest at S4, without intervening injury between these levels and T12 [19].
Vertebral body compression deformities are less common in the lumbar spine. We identified four lumbar fractures in two children. The lumbar fractures occurred in the lower lumbar spine region in case 8, but CT imaging confirmed additional contiguous upper lumbar and lower thoracic vertebral involvement in this case.
Fractures of the sacrum in child abuse are rare subtle injuries that require lateral radiographs of the spine that encompasses the sacrum and coccyx [6]. In our study, two children had fractures of the sacrum and coccyx; both showed mild compression. In one child (case 11), the sacral fracture was the only spinal injury identified. In the other (case 9), the overlying soft tissue fluid signal on MRI suggested that a slamming impact on the buttocks was responsible for the T12 fracture/dislocation [19].
Our study supports the view that single or multiple compression deformities, identified incidentally in the work-up of suspected abuse, are more common than the clinically important fracture/dislocations detailed in published cases reports [6, 12]. All of our cases showed a notable absence of clinical or physical evidence of spinal injury.
Associated clinically unsuspected skeletal findings on the skeletal survey were present in the majority (64%) of our cases, including injuries with high specificity for abuse such as rib fractures or CMLs in five cases (36%). All children with spinal injuries included in our study had other evidence suggesting inflicted injury, but it is notable that in five of our cases, the only clinically occult osseous injuries demonstrated on the skeletal survey were the spinal fractures.
Some studies report spinal injuries with coexistent abusive head trauma [9, 11, 12, 30], but a statistical relationship between spinal fractures and ICI in abused children has not been clearly established. In a recent systematic review of the literature designed to determine the clinical and radiographic characteristics associated with abusive and non-abusive head trauma, the authors made no reference to spinal injuries [31]. Koumellis and others [32] found spinal subdural hematoma in 44% of 18 children with abusive head trauma, and two of their cases had thoracic spine fractures noted radiographically. The authors emphasized that spinal subdural collections were likely related to pooling of blood originating from intracranial subdural hematomas [32]. Three of our patients had spinal subdural hematomas, as well as intracranial injury. With new recommendations for extending brain MR imaging to the spine in cases of suspected abusive head trauma [12, 32], special attention should be given to the vertebral osseous and ligamentous structures. Our findings indicate a significant relationship between spine fractures and ICI in a population of children with suspected child abuse. It is well-accepted that fractures are associated with ICI, but spinal fractures appear to have a special significance. We found that children with spinal fractures were at significantly greater risk for ICI than those with positive skeletal surveys, but no spinal injury.
The child protection and public health implications of these findings are important. In all cases, elements of the clinical presentation prompted additional inquiry and evaluation. The unexplained skeletal injuries, intracranial trauma and concerning social dynamics revealed upon further investigation by child protective services resulted in civil actions to ensure the safety of these children. One child died from intracranial injuries.
The principal limitation of our study was the retrospective design. The precise rationale for ordering the study was inferred from medical records only in the 14 cases with spinal fracture. Thus, our overall prevalence of spinal injury of 1.9% may not be generalizable to populations with different thresholds for ordering skeletal survey. We believe our 9.7% prevalence of spinal injuries among children with positive skeletal surveys may be a more meaningful figure. Since advanced imaging was done in a minority of children, our study likely underestimates the true prevalence of spinal injury in children with inflicted injuries. However, the study does provide a reasonable estimate of the likelihood of encountering a spine fracture radiographically in a child with suspected abuse.
Conclusion
Our study shows that spinal fractures are not rare in patients with positive skeletal surveys in suspected child abuse. Spinal fractures may be the only skeletal findings that support a traumatic event. Vertebral fractures in abused children are likely the consequence of high-energy events that are associated with a significant risk of intracranial injury, and this risk appears to be greater than in children without spinal injuries. Our study supports the current ACR guideline advising inclusion of the lateral views of the spine in the initial skeletal survey in cases of suspected abuse.
References
Galleno H, Oppenheim WL (1982) The battered child syndrome revisited. Clin Orthop Relat Res 162:11–19
King J, Diefendorf D, Apthorp J et al (1988) Analysis of 429 fractures in 189 battered children. J Pediatr Orthop 8:585–589
Kleinman PK, Marks SC Jr, Richmond JM et al (1995) Inflicted skeletal injury: a postmortem radiologic-histopathologic study in 31 infants. AJR Am J Roentgenol 165:647–650
Kogutt MS, Swischuk LE, Fagan CJ (1974) Patterns of injury and significance of uncommon fractures in the battered child syndrome. Am J Roentgenol Radium Ther Nucl Med 121:143–149
Merten DF, Radkowski MA, Leonidas JC (1983) The abused child: a radiological reappraisal. Radiology 146:377–381
Kleinman PK (1987) Diagnostic imaging of child abuse. Williams & Wilkins, Baltimore, pp 149–167
Belfer RA, Klein BL, Orr L (2001) Use of the skeletal survey in the evaluation of child maltreatment. Am J Emerg Med 19:122–124
Day F, Clegg S, McPhillips M et al (2006) A retrospective case series of skeletal surveys in children with suspected non-accidental injury. J Clin Forensic Med 13:55–59
Karmazyn B, Lewis ME, Jennings SG et al (2011) The prevalence of uncommon fractures on skeletal surveys performed to evaluate for suspected abuse in 930 children: should practice guidelines change? AJR Am J Roentgenol 197:W159–W163
Kleinman PK, Morris NB, Makris J et al (2013) Yield of radiographic skeletal surveys for detection of hand, foot, and spine fractures in suspected child abuse. AJR Am J Roentgenol 200:1–4
Swischuk LE (1969) Spine and spinal cord trauma in the battered child syndrome. Radiology 92:733–738
Kemp AM, Joshi AH, Mann M et al (2010) What are the clinical and radiological characteristics of spinal injuries from physical abuse: a systematic review. Arch Dis Child 95:355–360
Jha P, Stein-Wexler R, Coutler K et al (2013) Optimizing bone surveys performed for non-accidental trauma with attention to maximizing diagnostic yield while minimizing radiation exposure. Pediatr Radiol. doi:10.1007/s00247-012-2614-9 Epub ahead of print 29 January
Lindberg DM, Harper NS, Laskey AL et al (2013) Prevalence of abusive fractures of the hands, feet, spine, or pelvis on skeletal survey: perhaps “uncommon” is more common than suggested. Pediatr Emerg Care 29:26–29
Meyer JS, Gunderman R, Coley BD et al (2011) ACR appropriateness criteria(®) on suspected physical abuse-child. J Am Coll Radiol 8:87–94
American Academy of Pediatrics Section on Radiology (2009) Diagnostic imaging of child abuse. Pediatrics 123:1430–1435
Reston VA (2011) ACR-SPR practice guideline for skeletal surveys in children: revised 2011 (resolution 54). J Am Coll Radiol 1–6
Duffy SO, Squires J, Fromkin JB et al (2011) Use of skeletal surveys to evaluate for physical abuse: analysis of 703 consecutive skeletal surveys. Pediatrics 127:e47–e52
Tran B, Silvera M, Newton A et al (2007) Inflicted T12 fracture-dislocation: CT/MRI correlation and mechanistic implications. Pediatr Radiol 37:1171–1173
Astley R (1953) Multiple metaphyseal fractures in small children (metaphyseal fragility of bone). Br J Radiol 26:577–583
Kleinman PL, Kleinman PK, Savageau JA (2004) Suspected infant abuse: radiographic skeletal survey practices in pediatric health care facilities. Radiology 233:477–485
Karmazyn B, Duhn RD, Jennings SG et al (2011) Long bone fracture detection in suspected child abuse: contribution of lateral views. Pediatr Radiol 42:463–469
Harlan S, Nixon G, Campbell K et al (2009) Follow-up skeletal surveys for nonaccidental trauma: can a more limited survey be performed? Pediatr Radiol 39:962–968
Sonik A, Stein-Wexler R, Rogers KK et al (2010) Follow-up skeletal surveys for suspected non-accidental trauma: Can a more limited survey be performed without compromising diagnostic information? Child Abuse Negl 34:804–806
Drubach LA, Johnston PR, Newton AW et al (2010) Skeletal trauma in child abuse: detection with 18F-NaF PET. Radiology 255:173–181
Finch GD, Barnes MJ (1998) Major cervical spine injuries in children and adolescents. J Pediatr Orthop 18:811–814
Leonard M, Sproule J, McCormack D (2007) Paediatric spinal trauma and associated injuries. Injury 38:188–193
Mahan ST, Mooney DP, Karlin LI et al (2009) Multiple level injuries in pediatric spinal trauma. J Trauma 67:537–542
Twomey EL, Iemsawatdikul K, Stephens BG et al (2004) Multiple thoracic vertebral compression fractures caused by non-accidental injury: case report with radiological-pathological correlation. Pediatr Radiol 34:665–668
Feldman KW, Avellino AM, Sugar NF et al (2008) Cervical spinal cord injury in abused children. Pediatr Emerg Care 24:222–227
Piteau SJ, Ward MGK, Barrowman NJ et al (2012) Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: a systematic review. Pediatrics 130:315–323
Koumellis P, McConachie NS, Jaspan T (2009) Spinal subdural haematomas in children with non-accidental head injury. Arch Dis Child 94:216–219
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barber, I., Perez-Rossello, J.M., Wilson, C.R. et al. Prevalence and relevance of pediatric spinal fractures in suspected child abuse. Pediatr Radiol 43, 1507–1515 (2013). https://doi.org/10.1007/s00247-013-2726-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2726-x