Abstract
Background
Tracheomalacia is characterized by excessive expiratory collapse of the trachea.
Objective
To investigate the accuracy of free-breathing cine CT for diagnosis of tracheomalacia in young children with bronchoscopy as reference standard.
Materials and methods
In a retrospective study (May 2001–July 2008), a patient group (n = 27) of children with bronchoscopic evidence of tracheomalacia, and a control group (n = 320) underwent free-breathing cine CT. The tracheal shape on free-breathing cine CT was classified as round, lunate, elongated or crescentic. Cross-sectional area change of the trachea and age were compared between the groups and the diagnostic performance of free-breathing cine CT for tracheomalacia was evaluated.
Results
The patient group showed significantly greater cross-sectional area change of the trachea (57.2% ± 22.2% vs. 10.6% ± 11.2%, P < 0.001) than the control group. If a cross-sectional area change of the trachea of 31.6% was used as a cut-off value for the diagnosis of tracheomalacia, the sensitivity, specificity and accuracy of cine CT were 96.3% (26/27), 97.2% (311/320) and 97.1% (337/347), respectively. If a crescentic shape during the expiratory phase was used, the sensitivity, specificity and accuracy were 51.9% (14/27), 98.8% (316/320) and 95.1% (330/347), respectively.
Conclusion
Free-breathing cine CT has potential to provide the diagnosis of tracheomalacia in young children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tracheomalacia (TM) is a condition described as excessive expiratory collapse of the trachea resulting from weakness of the tracheal wall due to congenial or acquired abnormalities [1, 2]. The congenital form is related to immature tracheal cartilage, whereas the more common acquired form is a consequence of damaged or degenerated tracheal cartilage. TM severity varies considerably; its severest form may result in substantial morbidity and even mortality [1]. TM is often overlooked or misdiagnosed as asthma or another respiratory illness due to its nonspecific clinical manifestations, which results in a considerable delay in diagnosis and treatment. This highlights the importance of a prompt and accurate diagnosis of this condition.
The diagnosis of TM can be made by bronchoscopy or CT by demonstrating excessive expiratory collapse of the trachea. Bronchoscopy is an invasive procedure for which general anesthesia is often employed in children. Bronchoscopy is limited, however, by an operator dependency and has difficulty in evaluating the airways distal to a severe stenosis. As a result, CT is a useful noninvasive imaging method for the diagnosis of TM. However, the ability to follow respiratory maneuvers is almost mandatory for the diagnosis of TM with CT. Hence, general anesthesia with controlled ventilation is usually necessary in young children [2].
Free-breathing cine CT is a technique that does not need the patient to follow breathing instructions or require general anesthesia with controlled ventilation. The use of this method for TM diagnosis has not been tested thoroughly in young children. Accordingly, the purpose of this study was to investigate the diagnostic accuracy of free-breathing cine CT for the diagnosis of TM in young children with bronchoscopy as reference standard.
Materials and methods
Study population
This retrospective study was approved by the local ethics committee and informed consent was waived.
At our institution, free-breathing cine CT was performed for the following reasons: (1) to evaluate tracheobronchomalacia; (2) to evaluate air trapping and (3) to obtain thoracic CT images with less motion artifact by improving their temporal resolution, i.e. partial reconstruction used for cine CT [3, 4].
CT images and medical records of the children who underwent free-breathing cine CT between May 2001 and July 2008 were collected retrospectively. Any cases where respiratory maneuvers were used or an endotracheal or tracheostomy tube was placed during free-breathing cine CT were excluded. In addition, cases in which the trachea was not included in free-breathing cine CT were also excluded. Of 73 children who were suspected of having tracheomalacia, 36 children who did not undergo bronchoscopy or who had focal tracheal stenosis were excluded. Three children with a focal tracheal stenosis were excluded because the lesion may cause a false-positive diagnosis of TM on free-breathing cine CT: a focal tracheal stenosis was defined as a short (less than 2 cm in length) stenosis greater than 50% narrowing, and its presence was evaluated on pediatric spiral CT images covering the whole thorax. The remaining 37 children underwent bronchoscopy and the diagnosis of TM was based on their bronchoscopic findings. Of 832 children who were not suspected of having tracheomalacia, 522 children who had respiratory symptoms during free-breathing cine CT, a lung lesion greater than one segment or a substantial airway narrowing were excluded. In total, 347 children were included in this study cohort and were divided into three groups: patient group with positive bronchoscopy (TM group, n = 27; 15 boys, age range: 7 days–7 years), patient group with negative bronchoscopy (n = 10; 3 boys, age range: 10 days–4 years), and control group (n = 310; 191 boys, age range: 0 days–8 years). The latter two constituted patient groups without tracheomalacia (NTM group, n = 320). The inclusion and exclusion steps are illustrated in Fig. 1.
Underlying diseases in the TM group included a history of esophageal atresia with distal tracheoesophageal fistula in 11 children, bronchopulmonary dysplasia in 4, congenital heart disease in 3 and other illnesses in 9. Underlying diseases in the NTM group included congenital heart disease in 131 children, hemato-oncologic disease in 84, a congenital lung or mediastinal lesion in 27 and other illnesses in 24. In the remaining 54 children in the control group, the CT was negative in 36 and merely showed subsegmental atelectasis in 18.
Free-breathing cine CT
Free-breathing cine CT was obtained with a 4-detector-row CT system (LightSpeed Qx/i; GE Healthcare, Waukesha, WI). For cine CT scanning, the two most central detector rows (2 × 0.625 mm) were used to produce one 1.25-mm slice. To minimize the radiation dose, the scan time for each slice position was adjusted to be slightly longer than one respiratory cycle of each child in the range of 2.0 to 3.0 s. Five or six slices were positioned evenly to cover the lungs and airways as required: the entire lungs were covered to evaluate air trapping or to obtain thoracic CT images with less motion artifacts, while only the central airways were included to evaluate tracheobronchomalacia. By using partial reconstruction (225° gantry rotation, approximately 0.3 s) and multisegment reconstruction (0.2- to 0.3-s intervals), 10–12 cine CT images were reconstructed retrospectively per each slice position [2, 4]. Body weight-adjusted CT parameters were used as described in Table 1. Oral chloral hydrate (Pocral; 50 mg/kg, maximum 1 g; Hanlim, Seoul, Korea) was used for conscious sedation in children younger than 6 years of age. CT dose parameters including volume CT dose index (CTDIvol), dose-length product (DLP) and estimated effective dose using age-, gender-, and tube voltage-specific conversion factors based on the International Commission on Radiological Protection (ICRP) publication 103 [5] were calculated (Table 1).
CT analysis
All cine CT images included in this study showed diagnostic image quality. The cross-sectional area and shape of the trachea were evaluated on a representative slice of 5–6 free-breathing cine CT slices, showing the maximal cross-sectional area change. Tracheal cross-section areas were measured manually by a pediatric radiologist (12 years of experience in pediatric thoracic CT) on a PACS workstation (Petavision; Hyundai Information Technology and Asan Medical Center, Seoul, Korea) with a magnification factor of two and a fixed window setting (width/level: 1,800 HU/-650 HU) (Fig. 2). From the measured maximal (Max) and minimal (Min) areas throughout the respiratory cycle, cross-sectional area change of the trachea was calculated using the following formula:
Images in a 5-month-old girl with bronchoscopy-proven tracheomalacia (TM) and complex congenital heart disease. a Inspiratory-phase and (b) expiratory-phase cine CT images show excessive tracheal collapsibility. Cross-sectional area change of the trachea was 65.7%. Tracheal shape was lunate at inspiration and crescentic at expiration. Posterior concavity was noted at expiration (b)
To define the tracheal shape, a ratio of the transverse diameter to the anteroposterior diameter of the trachea was calculated. Depending on this ratio, the tracheal shape on free-breathing cine CT was classified into round (between 0.8 and 1.2), lunate (≥1.2), elongated (<0.8), or crescentic (≥2.0 with posterior concavity) at inspiration and expiration (Fig. 3).
Tracheal shapes on free-breathing cine CT according to the ratio of the transverse diameter to the anteroposterior diameter of the trachea. a Round shape shows a ratio of between 0.8 and 1.2. b Lunate shape shows a ratio of ≥1.2. c Elongated shape shows a ratio of <0.8. d Crescentic shape shows a ratio ≥2.0 with posterior concavity
Statistical analysis
The data were analyzed using SPSS statistical software version 20.0 (IBM, Chicago, IL). Cross-sectional area change of the trachea on free-breathing cine CT and age at free-breathing cine CT were compared between the groups using an unpaired Student’s t-test and analysis of variance, respectively. With respect to the cross-sectional area change on cine CT for the diagnosis of TM, an area under the receiver operating characteristic curve (AUC) was calculated. An optimal cut-off value was estimated from this receiver operating characteristic curve analysis when a sum of sensitivity and specificity was to be maximal. The diagnostic performance, i.e. sensitivity, specificity and accuracy, of free-breathing cine CT was evaluated for the diagnosis of TM on the basis of the cross-sectional area change of the trachea and the tracheal shape. Continuous variables are presented as the mean ± the standard deviation and nominal values are reported as frequencies. A P-value of less than 0.05 was considered to indicate a statistically significant difference.
Results
Tracheal collapse
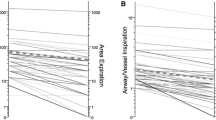
The measured maximal and minimal tracheal cross-sectional areas were 29.7 ± 17.0 mm2 and 13.9 ± 12.4 mm2, respectively, in the TM group and 36.1 ± 17.7 mm2 and 32.6 ± 17.0 mm2, respectively, in the NTM group. The TM group showed significantly greater cross-sectional area change of the trachea (57.2% ± 22.2 vs. 10.6% ± 11.2, P < 0.001) than the NTM group (Fig. 4). Age showed no significant difference between the two groups (660.3 days ± 773.9 vs 738.2 days ± 714.1, P = 0.62). Cine CT had an AUC of 0.98 (Fig. 5). If a cross-sectional area change of the trachea of 31.6% was used as a cut-off value for the diagnosis of tracheomalacia, the sensitivity, specificity and accuracy of cine CT were 96.3% (26/27), 97.2% (311/320) and 97.1% (337/347), respectively.
Box-and-whisker plot demonstrates a significant difference in cross-sectional area change of the trachea on free-breathing cine CT between the bronchoscopy-proven tracheomalacia (TM) and negative tracheomalacia (NTM) groups (57.2% ± 22.2% vs. 10.6% ± 11.2%, respectively; P < 0.001). * Extreme values of NTM group
Tracheal shape
A crescentic shape of the trachea was seen more frequently in the TM group (14.8–51.9%) than in the NTM group (0.3–1.3%) and at expiration in both groups (Table 2). If a crescentic shape during the expiratory phase was used for the diagnosis of TM, the sensitivity, specificity and accuracy were 51.9% (14/27), 98.8% (316/320) and 95.1% (330/347), respectively. Of 14 children with a crescentic tracheal shape during the expiratory phase, only one case demonstrated a cross-sectional area change (18.0%) lower than 31.6%, a cut-off value for the diagnosis of TM estimated in this study. In this case, bronchoscopy showed no evidence of TM.
Radiation dose
Estimated effective doses of cine CT were very low, in the range of 0.08–0.11 mSv for boys and 0.14–0.19 mSv for girls (Table 1).
Discussion
This study showed that free-breathing cine CT has potential to make the diagnosis of TM in young children by demonstrating a cross-sectional area change of the trachea of ≥31.6% or an expiratory crescentic shape. Hopefully, free-breathing cine CT would reduce the need for bronchoscopy, general anesthesia, and respiratory maneuvers needed for the diagnosis of TM in young children.
For the diagnosis of TM, CT should be performed at paired inspiratory and expiratory phases. To obtain the maximal degree of cross-sectional area change of the trachea in patients with TM, dynamic expiratory CT is preferred to end-expiratory CT because the degree of cross-sectional area change of the trachea is underestimated at end expiration due to a lower level of intrathoracic-extratracheal pressure [6]. Dynamic expiratory CT is acquired during the forced expiratory effort after taking a deep breath. Coughing elicits an even higher level of intrathoracic-extratracheal pressure than forced expiration, and cine CT during coughing may be used for diagnosing TM [7]. However, these respiratory maneuvers cannot be performed in young or uncooperative children. Instead, paired end-inspiratory and end-expiratory CT can be obtained in these children with the aid of general anesthesia and controlled ventilation [2].
In contrast, there is no requirement for respiratory maneuvers during free-breathing cine CT; thus, it can be easily performed in young children. Nonetheless, free-breathing cine CT has seldom been used for diagnosing TM. In a previous study [8] using a single-detector spiral CT system in 29 adults with tracheal stenosis or TM, significantly higher cross-sectional area change of the trachea (44% vs. 28%), more levels showing a cross-sectional area change of the trachea of ≥50% (38% vs. 13%), and a better correlation with bronchoscopy were seen with free-breathing cine CT than paired end-inspiratory and end-expiratory CT. Cine CT using an electron-beam CT system was also used previously to assess TM before and after aortosternopexy in ten young children [9] and free-breathing cine CT using a multidetector row CT has further been used to assess air trapping in children [3, 10]. However, free-breathing cine CT has not been regarded as an established imaging technique for diagnosing TM in children [2]. In this respect, the results of this study are very encouraging.
For the CT diagnosis of TM, a cross-sectional area change of the trachea of ≥50% has generally been accepted as the diagnostic criterion in children and adults [1, 2]. However, 78% of healthy volunteers exceeded this limit during forced expiration, resulting in a considerable overlap with genuine TM cases and thus lowering the diagnostic value of dynamic expiratory CT [11]. To prevent an overdiagnosis of TM, the authors suggested the need for a higher diagnostic criterion for TM during forced expiration. When a 31.6% cross-sectional area change of the trachea was used as a cut-off value for TM diagnosis in this study, only one child with bronchoscopy-proven TM showed a cross-sectional area change of the trachea (20.3%) lower than 31.6% and only 2.8% (9/320) in the NTM group exceeded the cut-off value, resulting in a high diagnostic performance of free-breathing cine CT. This might be attributable to a higher respiratory effort in children with TM that leads to a naturally accentuated discrimination between children with TM and without TM. Nonetheless, it remains to be clarified whether free-breathing cine CT is also good at differentiating children with TM from dyspneic children without TM who were excluded from this study.
Regarding the tracheal shape, only an expiratory crescentic shape, which was seen in half of the TM group, had diagnostic value for this disorder. On the contrary, a crescentic shape was infrequently (14.8%) seen at inspiration in the TM group and rarely seen in the NTM group at both inspiration (0.3%) and expiration (1.3%) (Table 2). These results are comparable to those of previous studies in adults [11, 12]. The expiratory crescentic shape was also seen in approximately half of adults with TM [12] and was very rare (1%) in healthy volunteers [11]. The identification of the expiratory crescentic shape in patients with TM may be helpful, not only for diagnosing TM, but also in selecting good candidates for membranous wall tracheoplasty [13]. Because the expiratory crescentic shape of the trachea results from excessive flaccidity of the posterior membranous tracheal wall, symptomatic patients with this tracheal shape are expected to benefit from the procedure of reinforcing the posterior wall by using polypropylene graft. In the aforementioned study of adults with TM [12], the inspiratory lunate shape (the ratio of the transverse diameter to the anteroposterior diameter of the trachea >1.0) was regarded as abnormal and was rarely (6%) observed. As the definition of the lunate shape in this study (the ratio ≥1.2) slightly differs from that used in the previous study, the inspiratory lunate shape was commonly seen in the TM group (55.6%) and the NTM group (47.2%). Consequently, the lunate shape should not be regarded as abnormal on free-breathing cine CT in young children.
Paired inspiratory and expiratory volumetric scans for diagnosing TM may result in radiation dose twice as high as that for standard inspiratory chest CT. Because children are more radiosensitive and have a longer life expectancy to develop radiation-induced harmful effects, the radiation dose of CT imaging techniques for diagnosing TM should be minimized. In a study of 40 children suspected of having TM [14], the radiation dose of paired end-inspiratory and end-expiratory CT could be reduced by 23%, from 6.4 ± 4.4 mSv to 4.8 ±1.9 mSv, without compromising diagnostic confidence; this was achieved by a 50% reduction of tube current for end-expiratory CT [14]. The radiation dose of free-breathing cine CT using noncontiguous sequential scanning is very low (0.08–0.19 mSv in this study) less than 0.2–0.3 mSv in children [15].
Various risk factors and diseases are associated with TM in infants and children [1, 2]. Among them, esophageal atresia with distal tracheoesophageal fistula, congenital heart disease and bronchopulmonary dysplasia were the three main contributors to the TM group in this study. TM is often (11–33%) found in cases of esophageal atresia with distal tracheoesophageal fistula, and more frequently after its surgical repair [16]. Taking this high prevalence of TM into account, any children with respiratory symptoms should be carefully assessed with a high clinical suspicion of TM and free-breathing cine CT should be performed in suspected cases. With respect to congenital heart disease, the prevalence of TM may be variable depending on specific cardiovascular defects and the spatial relationship between TM and adjacent cardiovascular structures should be accurately evaluated with contrast-enhanced cardiac CT and free-breathing cine CT [15, 17]. A study of children with mediastinal aortic vascular anomalies showed a high prevalence (53.3%) of TM [18].
Lateral fluoroscopy may be used for the diagnosis of TM in free-breathing young children but the imaging technique is seldom used for that purpose at our institution. Pulsed fluoroscopy and body size-adapted parameters should be used to reduce radiation dose. In addition, proper lateral positioning is crucial for the diagnosis. However, lateral fluoroscopy evaluating only anteroposterior diameter of the trachea may be disadvantageous because expiratory tracheal collapse in TM may occur in transverse direction. On the contrary, cine CT can assess TM in any direction, and the shape of TM because cross-sectional area of the trachea is evaluated. Moreover, associated abnormalities, such as lymphadenopathy, vascular compression and tracheal wall thickening, can be accurately evaluated at the same imaging session.
This retrospective study had several limitations. First, bronchoscopy was not performed in controls. However, bronchoscopy—an invasive procedure, particularly in children—is difficult to justify in a control group of young children. Second, only a few slices of the entire trachea were evaluated by free-breathing cine CT. As a result, a focal TM may be missed and a focal fixed tracheal stenosis may be misdiagnosed as TM due to the physiological longitudinal motion of the trachea during the respiratory cycle. Therefore, three cases with focal tracheal stenosis were excluded from the bronchoscopy group in this study (Fig. 1). For the same reason, the severity of TM may be underestimated when the level showing the maximal cross-sectional area change is not included in the few scanned CT slices. These technical limitations can be overcome by using volumetric free-breathing cine CT, the four-dimensional airway CT [15, 19]. Third, a reproducibility study of the measurements was not performed in this study. Nonetheless, intra- and inter-individual variations in the measurements would be relatively narrow because fairly conspicuous air-tissue contrast may facilitate consistent delineation of the tracheal cross-sectional area. Ultimately, semiautomatic detection of the tracheal cross-sectional area is recommended. Fourth, sedation might influence tracheal collapse on cine CT. However, breathing is regular in tidal volume in most uncomplicated sedated children.
Conclusion
Free-breathing cine CT has potential to provide the diagnosis of TM in young children by quantifying cross-sectional area change of the trachea and identifying an expiratory crescentic shape of the trachea. Free-breathing cine CT would reduce the need for the general anesthesia and controlled ventilation needed for diagnosing TM in young children.
References
Carden KA, Boiselle PM, Waltz DA et al (2005) Tracheomalacia and tracheobronchomalacia in children and adults: an in-depth review. Chest 127:984–1005
Lee EY, Boiselle PM (2009) Tracheobronchomalacia in infants and children: multidetector CT evaluation. Radiology 252:7–22
Goo HW, Kim HJ (2006) Detection of air trapping on inspiratory and expiratory phase images obtained by 0.3-second cine CT in the lungs of free-breathing young children. AJR Am J Roentgenol 187:1019–1023
Ha HI, Goo HW, Seo JB et al (2006) Effects of high-resolution CT of the lung using partial versus full reconstruction on motion artifacts and image noise. AJR Am J Roentgenol 187:618–622
Goo HW (2012) CT radiation dose optimization and estimation: an update for radiologists. Korean J Radiol 13:1–11
Baroni RH, Feller-Kopman D, Nishino M et al (2005) Tracheobronchomalacia: comparison between end-expiratory and dynamic expiratory CT for evaluation of central airway collapse. Radiology 235:635–641
Boiselle PM, Lee KS, Lin S et al (2006) Cine CT during coughing for assessment of tracheomalacia: preliminary experience with 64-MDCT. AJR Am J Roentgenol 187:W175–W177
Heussel CP, Hafner B, Lill J et al (2001) Paired inspiratory/expiratory spiral CT and continuous respiration cine CT in the diagnosis of tracheal instability. Eur Radiol 11:982–989
Kao SC, Kimura K, Smith WL et al (1995) Tracheomalacia before and after aortosternopexy: dynamic and quantitative assessment by electron-beam computed tomography with clinical correlation. Pediatr Radiol 25:S187–S193
Hong SJ, Goo HW, Roh JL (2008) Utility of spiral and cine CT scans in pediatric patients suspected of aspirating radiolucent foreign bodies. Otolaryngol Head Neck Surg 138:576–580
Boiselle PM, O’Donnell CR, Bankier AA et al (2009) Tracheal collapsibility in healthy volunteers during forced expiration: assessment with multidetector CT. Radiology 252:255–262
Boiselle PM, Ernst A (2006) Tracheal morphology in patients with tracheomalacia: prevalence of inspiratory lunate and expiratory “frown” shapes. J Thorac Imaging 21:190–196
Lee KS, Ashiku SK, Ernst A et al (2008) Comparison of expiratory CT airway abnormalities before and after tracheoplasty surgery for tracheobronchomalacia. J Thorac Imaging 23:121–126
Lee EY, Strauss KJ, Tracy DA et al (2010) Comparison of standard-dose and reduced-dose expiratory MDCT techniques for assessment of tracheomalacia in children. Acad Radiol 17:504–510
Goo HW (2010) State-of-the-art CT imaging techniques for congenital heart disease. Korean J Radiol 11:4–18
Briganti V, Oriolo L, Buffa V et al (2005) Tracheomalacia in oesophageal atresia: morphological considerations by endoscopic and CT study. Eur J Cardiothorac Surg 28:11–15
Goo HW (2004) Evaluation of the airways in patients with congenital heart disease using multislice CT. J Korean Pediatr Cardiol Soc 8:37–43
Lee EY, Zurakowski D, Waltz DA et al (2008) MDCT evaluation of the prevalence of tracheomalacia in children with mediastinal aortic vascular anomalies. J Thorac Imaging 23:258–265
Greenberg SB (2012) Dynamic pulmonary CT in children. AJR Am J Roentgenol 199:435–440
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goo, H.W. Free-breathing cine CT for the diagnosis of tracheomalacia in young children. Pediatr Radiol 43, 922–928 (2013). https://doi.org/10.1007/s00247-013-2637-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2637-x