Abstract
Background
Eosinophilic colitis (EC) is a gastrointestinal disease of undetermined etiology whose clinical features overlap with those of the inflammatory bowel diseases. To the best of our knowledge, the CT imaging features of EC have not been described in children.
Objective
To report and analyze the clinical, imaging and histological findings in seven children with EC.
Materials and methods
Children with EC were identified in a pediatric pathology database, and those with CT imaging within 2 months of diagnosis were included, totaling seven children. Clinical, imaging and pathological features were reviewed and analyzed.
Results
The most common presenting symptoms were abdominal pain, bloody diarrhea and rectal bleeding. EC was characterized as a dense and predominantly eosinophilic inflammatory infiltrate in the lamina propria or epithelium without granulomas. CT scans were abnormal in six children (86%), demonstrating colonic wall thickening, predominantly cecal, in five (71%), mild to moderate terminal ileal thickening in two (29%), and pneumatosis in one (14%). Right colonic involvement was greater than terminal ileal involvement.
Conclusion
CT imaging findings in children with EC include right colonic wall thickening of variable extent downstream and absent or mild involvement of the terminal ileum. EC should be considered in the differential diagnosis in children presenting with abdominal pain and bloody diarrhea.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eosinophilic colitis (EC) is in the spectrum of primary eosinophilic gastrointestinal disorders, which also includes eosinophilic esophagitis, eosinophilic gastritis and eosinophilic gastroenteritis. In each of these diseases, there is an infiltration of the gut wall by eosinophils. EC is the least commonly reported of these disorders [1]. Symptoms of EC include bloody diarrhea, abdominal pain and weight loss. Colonoscopy findings include edema, erythema and superficial ulcerations. Diagnosis is based on histological identification of increased eosinophils, which can predominantly affect the submucosa, muscularis propria or serosal layer [2]. Symptoms and signs are related to the layer that is predominantly involved. Patients with disease showing mucosal predominance present with protein-losing enteropathy, anemia, malabsorption and diarrhea [3]. Those with transmural disease present with intestinal obstruction, volvulus [4], intussusception [5, 6] or perforation [7, 8]. Serosal involvement is generally associated with ascites [9], which can be eosinophilic [10]. Diagnosis is confounded by the fact that no standard exists for the normal quantity of colonic eosinophils. Peripheral blood eosinophil levels are typically elevated but can often be normal. EC is a diagnosis of exclusion and the differential diagnosis of colonic eosinophilia includes inflammatory bowel disease (IBD), bacterial or parasitic colitis, drug-induced colitis and hypereosinophilic syndrome [11]. Treatment for EC is oral corticosteroids. Although a series of reports present detailed radiological findings of EC in adults, imaging findings in children have not been described [4–10, 12]. Our objective was to review the clinical, imaging and pathological features in children with EC.
Materials and methods
We obtained institutional review board (IRB) approval prior to performing this retrospective HIPAA-compliant investigation. The requirement for patient informed consent was waived.
The Children’s Hospital of Colorado pediatric pathology database from January 2010 to September 2011 was searched for children with a clinical diagnosis of EC. Fifteen children’s records were identified and all available imaging was reviewed. Of these children, seven met the inclusion criterion of having abdominal and pelvic imaging within 2 months of biopsy. All relevant fluoroscopic, CT and magnetic resonance enterography (MRE) imaging was retrospectively reviewed by two pediatric radiologists (J.B., L.F.) with 1 and 14 years of experience in pediatric radiology, respectively. Because there are no published standards for normal bowel wall thickness in children, the large and small bowel were deemed thickened if there was appropriate luminal distention and the bowel wall was objectively more prominent than “barely perceptible” [13]. Mesenteric lymph nodes were deemed enlarged if the short-axis diameter exceeded 8 mm [14]. Histological samples were reviewed by two pathologists (K.C., J.M.), with 9 years of pathology experience and 5 years of experience in the examination of tissues, respectively. The clinical information was compiled for all children, and included age and gender, race, clinical symptoms, medications, laboratory data including complete blood count with differential, serum inflammatory markers (erythrocyte sedimentation rate, C-reactive protein), IgE levels, IBD serologies and basic metabolic panel, and fecal studies including culture, Hemoccult and inflammation (calprotectin).
Results
Clinical data
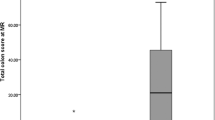
The seven children ranged in age from 15 months to 16 years (10.2 ± 6.3 years, mean ± SD) with a predominance of boys (four boys, 57%). The ethnic distribution was five (71%) Caucasian and two (29%) Hispanic. The most common presenting symptoms were abdominal pain (in six children), bloody diarrhea (in five), peripheral edema (in three) and rectal bleeding (in three). No clinical features highly suggestive of IBD were identified, such as growth failure or extraintestinal manifestations of IBD. At presentation, four children had a white blood cell count greater than 10,000/μl and three children had an absolute peripheral eosinophil count greater than 600/μl. Laboratory findings included anemia (in three children), hypoalbuminemia (in three), thrombocytosis (in three) and elevated systemic inflammatory markers (in three). Six of the seven children had Hemoccult-positive stools and all stool cultures were negative for infection. Two children had increased fecal calprotectin (ordered to assess neutrophilic inflammation). One child had an abnormal IBD serology (ordered to determine whether additional immunosuppression or studies were needed). This child received topical steroids. Serum IgE was normal when measured.
Pathological data
Mucosal pinch biopsies of the terminal ileum and colon obtained at the time of endoscopy revealed eosinophilic gastrointestinal mucosal eosinophilia, lamina propria lymphoplasmacytosis and rare neutrophils. Mucosal eosinophilia is defined as an increase in eosinophilia number and distribution. In the children described here, eosinophils were increased above other inflammatory cells to a value greater than 50–70 eosinophils per high-power field, depending on the location of the biopsy, and involved the lamina propria and in some children also invading the epithelium. Eosinophils showed degranulation and a fibrotic stromal background. Eosinophils were present within the crypt epithelial cells, and crypt abscess was a common finding (Fig. 1).
Radiological data
Seven children had CT examinations of the abdomen and pelvis, all performed with intravenous and oral contrast agents. Sagittal and coronal mean multiplanar reconstructions of all studies were produced. In two of the seven children, enteric contrast agent had not reached the colon at the time of imaging, limiting evaluation. The colon was abnormal in six of the seven children. No colonic abnormality was evident in one of two children with no colonic intraluminal contrast. Cecal wall thickening was present in five children (71%). Wall thickening ranged from isolated haustral thickening (Fig. 2) to circumferential thickening (Figs. 3 and 4). In four of the five children with wall thickening, the cecum or ascending colon was the most affected portion. Mucosal hyperenhancement isolated to the cecum and ascending colon without wall thickening was present in one child (14%). One child (14%) had pneumatosis with wall thickening, predominantly involving the rectum (Fig. 5).
Patient 5 (10-year-old boy). a Sagittal CT image shows moderate cecal wall thickening (black arrow) and mild terminal ileal wall thickening (white arrow). b Coronal CT image shows cecal wall thickening greater than descending colonic wall thickening (black arrow) and a small amount of infrahepatic ascites (white arrow)
Patient 6 (13-year-old boy). a Oblique coronal CT image shows moderate ascending colonic wall thickening with luminal contrast (black arrow) and featureless descending colonic wall thickening without luminal contrast (white arrow). b Oblique axial CT image shows mild transverse colonic wall thickening (black arrow)
In addition to colonic wall thickening, terminal ileal thickening was present in two children (29%), mild in one (Fig. 3) and moderate in the other. The degree of thickening in each was less than the degree of colonic wall thickening. Mild segmental jejunal and duodenal wall thickening was present in one child. Ascites was present in three children (43%), a moderate amount in one and a small amount in two. These children did not have clinical signs to suggest alternative hepatic, cardiac or renal etiologies for their ascites. Bilateral pleural effusions were present in one child. Enlarged mesenteric lymph nodes were present in three children (43%). CT findings are summarized in Table 1.
Two children had three MRE examinations, which were normal (patient 5 had one and patient 7 had two examinations). No colonic contrast agent was used for the MRE examinations. A fluoroscopic upper gastrointestinal examination with small-bowel follow-through was performed in patient 3, and was normal.
Discussion
EC is a relatively uncommon idiopathic cause of colitis in children. It is a diagnosis of exclusion that is made after other causes of colonic eosinophilia, such as infection and IBD, are excluded. IBD is a clinical diagnosis that has characteristic symptoms and classic histopathological features such as granulomas in Crohn disease and chronic colitis with neutrophilic inflammation and crypt branching in ulcerative colitis. Although eosinophils are associated with IBD, the children described here had a predominant eosinophilic inflammation and not the overriding features associated with Crohn disease or ulcerative colitis. Whether the children described here develop either of these diseases will be determined by long-term follow-up.
Clinical symptoms and colonoscopy findings in EC are nonspecific. Diagnosis relies on histological sampling that shows dense eosinophilic infiltration of the intestinal mucosa. Presentation of the serosal form of EC can lead to ascites as the presenting feature; in this form, mucosal biopsies can be unrevealing and the diagnosis might rest on analyses of ascites and exclusion of other causes of eosinophilia [15].
Descriptions of the radiological features of EC are limited to case reports and reviews describing adults. Reports of imaging in EC describe unusual presentations, including a contrast enema demonstrating colocolonic intussusception [6], ileal wall thickening, mesenteric lymphadenopathy and a radiograph of cecal volvulus complicating EC [4]. Reported CT findings in adults include circumferential colonic wall thickening and ascites [11, 16], long-segment thickening from the ascending to the descending colon [17] and mucosal fold thickening and the “araneid-limb-like” sign in the ascending and transverse colon [12]. In addition, colonic inflammation has been noted as a feature of other eosinophilic gastrointestinal diseases. One series documenting the imaging findings in eosinophilic gastroenteritis included fluoroscopic barium studies in ten patients, which showed mucosal edema or thickening of the small-intestinal wall, partial gastric outlet obstruction and narrowing of the lumen of the terminal ileum [18].
Our study was limited in that it was a retrospective review, and not all children diagnosed with EC underwent CT evaluation, possibly biasing our findings. Our patient sample size was small. Our MRE protocol is not optimized to evaluate the colon. The MRE protocol includes oral but not rectal contrast agent administration, and no contrast agent was present in the colon on any of the examinations. This, in combination with a susceptibility artifact from air within the colon, significantly limited evaluation of the colon. This might explain why not all the MRE examinations detected pathological changes. If MRE findings are to be considered in future studies, either rectal contrast agent or oral contrast agent with a longer delay to imaging might be necessary.
One child in our series (patient 4) had an unusual pattern with predominant rectal involvement, extensive colonic pneumatosis, moderate volume ascites and moderate pleural effusions. This constellation of findings is suggestive of serosal involvement. This child had eosinophilic infiltration of the mucosa and submucosa, but because only pinch mucosal biopsies were obtained, serosal involvement could not be confirmed.
We found a range of CT colonic and extracolonic findings in our seven patients with EC. However, in five of the seven children, the predominant colonic segment involved was the cecum or ascending colon with less severe or no involvement of the more distal colon. In addition, the small bowel was either normal or involved to a lesser degree than the colon in all of these children. This is in distinction to the typical findings in Crohn disease and ulcerative colitis. In Crohn disease, there is typically segmental involvement of the colon with predominant involvement of the terminal ileum. In ulcerative colitis, there is rectal involvement with variable continuous upstream colonic involvement.
Conclusion
In the clinical context of a child presenting with bloody stools and abdominal pain, if the CT examination reveals predominant right colonic wall thickening with relative sparing of the terminal ileum, EC should be included in the differential diagnosis along with inflammatory and infectious colitis. Further studies are needed to confirm these findings because this is a small case series.
References
Rothenberg ME (2004) Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol 113:11–28
Klein NC, Hargrove RL, Sleisenger MH et al (1970) Eosinophilic gastroenteritis. Medicine (Baltimore) 49:299–319
Clouse RE, Alpers DH, Hockenbery DM et al (1992) Pericrypt eosinophilic enterocolitis and chronic diarrhea. Gastroenterology 103:168–176
Velchuru VR, Khan MA, Hellquist HB et al (2007) Eosinophilic colitis. J Gastrointest Surg 11:1373–1375
Shin WG, Park CH, Lee YS et al (2007) Eosinophilic enteritis presenting as intussusception in adult. Korean J Intern Med 22:13–17
Box JC, Tucker J, Watne AL et al (1997) Eosinophilic colitis presenting as a left-sided colocolonic intussusception with secondary large bowel obstruction: an uncommon entity with a rare presentation. Am Surg 63:741–743
Fraile G, Rodriguez-Garcia JL, Beni-Perez R et al (1994) Localized eosinophilic gastroenteritis with necrotizing granulomas presenting as acute abdomen. Postgrad Med J 70:510–512
Minciu O, Wegmann D, Gebbers JO (1992) Eosinophilic colitis – an unusual cause of acute abdomen. Case report and literature review. Schweiz Med Wochenschr 122:1402–1408
Ong GY, Hsu CC, Changchien CS et al (2002) Eosinophilic gastroenteritis involving the distal small intestine and proximal colon. Chang Gung Med J 25:56–61
Kravis LP, South MA, Rosenlund ML (1982) Eosinophilic gastroenteritis in the pediatric patient. Clin Pediatr (Phila) 21:713–717
Okpara N, Aswad B, Baffy G (2009) Eosinophilic colitis. World J Gastroenterol 15:2975–2979
Anuradha C, Mittal R, Yacob M et al (2012) Eosinophilic disorders of the gastrointestinal tract: imaging features. Diagn Interv Radiol 18:183–188
d’Almedia M, Jose J, Oneto J et al (2008) Bowel wall thickening in children: CT findings. Radiographics 28:727–746
Karmazyn B, Werner EA, Rajaie B et al (2005) Mesenteric lymph nodes in children: what is normal? Pediatr Radiol 25:774–777
Wiesner W, Kocher TH, Heim M et al (2002) CT findings in eosinophilic enterocolitis with predominantly serosal and muscular bowel wall infiltration. Belg J Radiol 85:4–6
Gaertner WB, MacDonald JE, Kwaan MR et al (2011) Eosinophilic colitis: University of Minnesota experience and literature review. Gastroenterol Res Pract 2011:857508
Chen YJ, Lin YF, Hsieh TY et al (2010) Eosinophilic colitis. Dig Liver Dis 42:230
Lee CM, Changchien CS, Chen PC et al (1993) Eosinophilic gastroenteritis: 10 years experience. Am J Gastroenterol 88:70–74
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brandon, J.L., Schroeder, S., Furuta, G.T. et al. CT imaging features of eosinophilic colitis in children. Pediatr Radiol 43, 697–702 (2013). https://doi.org/10.1007/s00247-012-2615-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-012-2615-8