Abstract
We report the CT and MR characteristics of a newborn with a rare, complex malformation characterised by a large rhinopharyngeal and oropharyngeal enterogenous cyst, associated with an osseous defect of the basiocciput, called canalis basilaris medianus (CBM). A partial herniation of the bulb was demonstrated through the bony defect on the midline. The enterogenous cyst occupied the rhinopharynx and oropharynx, narrowing the pharyngeal lumen and making it difficult for the introduction of an orotracheal tube.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Canalis basilaris medianus (CBM) is an uncommon variant or mild anomaly of the basiocciput, as first described by Grubber in 1880 [1].
It consists of a well-defined channel originating on the intracranial surface of the basiocciput in the midline, very close to the anterior rim of the foramen magnum [2].
We report the case of a newborn with a complete inferior CBM associated to a rhino-oropharyngeal enterogenous cyst, diagnosed in the first month of life by MRI evaluation and CT scan.
Case report
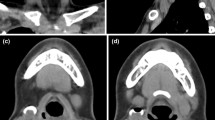
A 1-month-old girl was admitted to the Department of Paediatrics of our institute with a history of growth retardation and vomiting at the end of every feed. During hospitalisation, new symptoms such as nystagmus, serious crisis of desaturation and bradycardia appeared. A nasotracheal intubation was necessary. The procedure was difficult because of a pearly white, translucent and hard-elastic mass occupying pharyngeal lumen. Urgent MRI and CT scans were performed. MRI examination (Magnetom Sensation 1.5 T; Siemens, Erlangen, Germany) was performed with sagittal and axial images, T1-weighted, T2-weighted and PD-weighted spin-echo (SE) and fast spin-echo (FSE) sequences. We also obtained multiplanar reconstruction gradient echo (MPR-GE) T1-weighted and half-Fourier acquired single-shot turbo spin-echo (HASTE) T2-weighted sequences. MRI showed a median, lengthened, large osseous defect, situated on the basiocciput. Through the bony defect, a partial herniation of the bulb was identified on axial images and even more on the sagittal ones. A large cystic lesion with a coexisting water signal occupied the rhinopharynx and oropharynx, narrowing the pharyngeal lumen and making it difficult for nasotracheal tube introduction. The cyst had a close relationship of contiguity with the endotracheal tube (Fig. 1). The child underwent a multislice CT (Somatom Sensation 16 multi-row detector; Siemens, Erlangen, Germany) scan for a better evaluation of the bone structures. The CT scan confirmed a wide osseous defect involving the basiocciput. The transverse diameter of the posterior fossa was mildly reduced (Fig. 2). Finally, the newborn was operated upon using a transoral approach, at the Neurosurgery Department of G. Gaslini Children’s Hospital. A huge enterogenous cyst was found and excised at surgery.
MR examination performed after nasotracheal intubation. High-resolution sagittal (a, b) and axial (c, d) FSE T2-weighted images. A large, hyperintense cystic lesion (asterisk) occupies the oropharynx and rhinopharynx, showing a close relationship with the endotracheal tube (black arrow). Note the partial herniation of the medulla oblongata through the bone defect (white arrow)
Following resection, a fistula with a diameter of 1 mm was noted in the posterior pharyngeal wall. It was closed by suturing. No active cerebrospinal fluid (CSF) leakage was seen with the Valsalva manoeuvre. No correction of the bone defect was performed.
The child tolerated the procedure well, without sequelae and she is developing normally.
Discussion
CBM is an uncommon anomaly, consisting of a defined osseous channel placed in the intracranial surface of the basiocciput in the midline [1]. It can be considered as a partial failure of the normal ossification process of the basiocciput, which normally involves up to 15 separate enchondral and intramembranous ossification centres [2, 3]. The first modern studies about CBM anatomical variants are those of Currarino [1]. According to Currarino’s studies, Jaquemin et al. [2] described six varieties of CBM, three complete (superior, inferior and bifurcated) and three incomplete (thin, long channel through post-sphenoid and basiocciput, superior recess within the basiocciput and inferior “foveola pharyngica” recess) (Fig. 3). The complete type of CBM is characterised by the presence of a complete channel that runs through the basiocciput with connection between intracranial and extracranial structures.
Frequently, the presence of a complete osseous skull defect is associated with recurrent meningitis. Our patient never presented this condition.
The origin of CBM is unclear. The first pathogenetic hypothesis is the persistence and the enlargement of emissary veins’ canal in postnatal life (vascular hypothesis). A second theory supposes the persistence, in extrauterine life, of canalis chordae or notochord and its remnants [2]. According to this hypothesis, an impaired notochord development (induction defect) or the presence of notochord remnants would be responsible for bad basiocciput development [4]. This hypothesis is corroborated by the direct contact at the basiocciput, during the 4th–5th gestational weeks, between the notochord and the endoderm of the embryonic pharynx [2].
Our case can be considered as an inferior complete CBM that configures an abnormal communication between pharynx and endocranial structures, associated with a partial herniation of bulb. The newborn also had a huge cystic lesion occupying the rhinopharyngeal and oropharyngeal lumen. The range of neuroradiological hypotheses included a basioccipital meningoencephalocele, according to the bulb herniation, an enterogenous cyst, because of lengthened appearance of the lesion, an epidermoid cyst or huge Tornwaldt’s cyst or thyroglossal duct cyst [5].
Histological examination, performed by histochemical and immunohistochemical staining, showed a rare enterogenous cyst (Fig. 4).
Microphotograph of the cyst wall and its contents. Although distorted by the cauterisation, gland-like structures (a) and an epithelial lining (b) are recognisable. The epithelium is composed of pseudostratified columnar cells reminiscent of the respiratory mucosa (a haematoxilin and eosin, 200×; b haematoxilin and eosin, 400×)
The term “enterogenous cyst” was first used by Harriman to describe cysts previously known as neuroenteric, endodermal, epithelial, broncogenic or foregut cysts [6]. They are considered congenital anomalies of endodermal origin and are generally localised in the mediastinum, abdominal cavity and rarely in the spinal canal or skull. Very rare reports describe the possibility of an intracranial localisation of an enterogenous cyst at the cerebellopontine angle cistern or at the craniovertebral junction [7].
To explain the possible intracranial localisation, Graziani and coworkers suggested that an enterogenous cyst, colloid cyst and Rathke cleft cyst could originate from Seessel’s pouch, a diverticulum of the primitive foregut that in humans usually regresses and disappears.
Enterogenous cysts were classified by Wilkins and Odom [7] according to histological characterisation of their wall and to the presence or absence of specific components of respiratory or gastrointestinal tracts. Our case showed a gastro-intestinal and respiratory epithelium, denoting an enterogenous type A cyst.
To our knowledge, our case is the first reported in the literature with an histologically proven association between a complete CBM and a pharyngeal enterogenous cyst.
Another case was recently reported by Lohman et al. [8]. They describe, in an adult, a malformation characterised by an incomplete CBM associated with a circumscribed, asymptomatic, rhinopharyngeal cystic lesion. The patient did not undergo surgery and, consequently, a histological characterisation of the cyst nature was not performed.
Concluding, our case demonstrates that the failure of a single embryogenic step at 3rd–4th gestational week, involving substantially the nothocord, could explain both macroscopic malformations of the skull base and pharynx.
References
Currarino G (1988) Canalis basilaris medianus and related defects of the basiocciput. AJNR 9:208–211
Jaquemin C, Bosley TM, Saleh M (2000) Canalis basilaris medianus: MRI. Neuroradiology 42:121–123
Kuta AJ, Laine FJ (1993) Imaging the sphenoid bone and basiocciput: anatomic considerations. Semin Ultrasound CT MR 14:146–159
Tortori-Donati P, Cama A, Fondelli MP et al (1996) Cephaloceli. In: Tortori-Donati P, Taccone A, Longo M (eds) Malformazioni cranio-encefaliche. Neuroradiologia. Edizioni Minerva Italica, Torino, pp 107–124
Robson CD (2003) Cysts and tumors of the oral cavity, oropharynx, and nasopharynx in children. Neuroimaging Clin N Am 13:427–442, ix
Balasubramaniam S, Tyagi DK, Sawant HV (2011) Intramedullary enterogenous cyst of the conus medullaris presenting as lower limb pain. J Craniovertebr Junct Spine 2:46–48
Marchionni M, Smith C, Eljamel MS (2008) Intracranial enterogenous cyst extending into both supratentorial and infratentorial compartments: case report and review of the literature. Skull Base 18:213–216
Lohman BD, Sarikaya B, McKinney AM et al (2011) Not the typical Tornwaldt’s cyst this time? A nasopharyngeal cyst associated with canalis basilaris medianus. Br J Radiol 84:e169–e171
Acknowledgements
We would like to thank the Neurosurgery team of G. Gaslini Children’s Hospital, Genova, Italy, directed by professor Armando Cama.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morabito, R., Longo, M., Rossi, A. et al. Pharyngeal enterogenous cyst associated with canalis basilaris medianus in a newborn. Pediatr Radiol 43, 512–515 (2013). https://doi.org/10.1007/s00247-012-2513-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-012-2513-0