Abstract
Background
Acoustic noise may have adverse effects, even in patients under general anesthetic.
Objective
We aimed to determine the effect of headphones on sevoflurane requirements in children undergoing general anesthesia for an MRI scan.
Materials and methods
Children scheduled for MRI were enrolled in the study. Sevoflurane was used for general anesthesia in all children. Patients were randomly divided into two groups, one to wear headphones and the other none. After reaching a predetermined end-tidal concentration, the MRI scan was initiated, and the patient was evaluated by an observer blinded to the concentration of sevoflurane. Awakening was defined as eye opening, onset of continued purposeful movement or phonation. Using the Dixon up-and-down method, each target concentration was determined by the response of the previous child in the same group.
Results
The study included 28 children undergoing MRI. There was a significant difference in ED50 between the two groups (0.92, 0.81–1.02, vs. 0.47, 0.42–0.63; P < 0.001). The times to spontaneous arm and leg movements, eye opening and discharge from the post-anesthesia care unit were significantly shorter in patients with headphones than in those without (P < 0.001). However, there was no difference in times to hospital discharge (P = 0.056).
Conclusion
Noise-concealing headphones decrease inhalational anesthetic requirements and facilitate recovery. We recommend the routine use of headphones in children undergoing an MRI scan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although (MRI) does not cause any pain, it requires the patient to remain immobile throughout the period of the scan. This scan duration is usually 15–45 min depending on the diagnostic requirements. Children unable to cooperate or stay immobile are usually sedated or given general anesthesia. Anesthetizing techniques vary from one institution to another and there is little consensus [1, 2]. Sedation is less invasive, and saves cost and time, but with sedation the rate of scan failure is high, and prematurely terminated or repeated scans have important financial consequences [1–3]. General anesthesia has distinct advantages including greater reliability and independence from the child’s level of cooperation [2]. Delayed recovery after general anesthesia wastes scanning time and thus increases costs. Clinicians choose anesthesia according to their experience or the clinical routine of the institution.
MRI scanners make acoustic noise that reaches levels of 110–130 dB [4]. This intense noise causes discomfort, and children may become anxious and frightened, causing them to move. Conventional sound absorbers such as headphones significantly reduce the acoustic noise levels and make the MRI environment more tolerable [5]. Headphones are very much under-utilized by clinicians providing sedation or general anesthesia in MRI suites. Therefore we aimed to evaluate the effect of headphones in children having general anesthesia for an MRI scan. We specifically tested the hypothesis that headphones would decrease the sevoflurane requirements to ensure immobility during MRI as evaluated by the Dixon up-and-down technique.
Materials and methods
After receiving approval from the institutional review board, children ages 1–10 years with ASA physical status 1 or 2 who were scheduled for elective MRI under general anesthesia were enrolled and evaluated in the study. The study was performed at the Gulhane Military Hospital during 2007–2009. Written informed consent was obtained from the parents of the each participant. The MRI scanner used was a Philips Intera (Philips Healthcare, Best, The Netherlands), and the sequences used were T2 turbo spin-echo, T2 FLAIR, T1 turbo spin-echo, diffusion-weighted and 3-D T1 turbo field echo, with bandwidths in the range 60–80 mm, a slew rate of 80 mT/m/ms and noise levels of 18.1–24.1 dB. Prior to the procedure, the child’s medical history was taken and a general medical examination was performed. Children with no significant medical problems and no contraindications to general anesthesia were included in the study. Children with an abnormal airway, reactive airway disease, chronic respiratory disease, or a history of upper respiratory tract infection in the preceding 2 weeks were excluded. Children with a history of heart diseases, or congenital head and neck anomalies were also excluded.
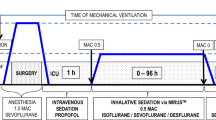
Children were not premedicated before anesthesia. Sevoflurane 8% (vaporizer setting) was given to induce anesthesia under assisted controlled ventilation for 2 min, and when adequate anesthesia had been established an intravenous route was opened on the hand. The entire sedation procedure was carried out with an MRI-compatible anesthesia machine (Lamtec 880; Pneupac, Luton, UK), and standard monitoring consisted of a five-lead ECG, noninvasive blood pressure, pulse oximetry and end-tidal CO2 monitoring. Pulse oximetry and capnography (Datex-Ohmeda S5; Datex-Ohmeda Division, Instrumentarium Corp., Helsinki, Finland) were monitored from the outset and throughout the procedure. Respiratory gases were also followed (Millennia 3,155 MVS; In Vivo Research, Orlando, FL).
The children were randomly divided into two groups using a system of sealed envelopes. Group 1 received headphones (MRI non-magnetic Noise Guard headset RA-1002, providing 25 dB of noise attenuation), and group 2 did not receive headphones. A mixture of sevoflurane, oxygen and air at 5 l/min was maintained with spontaneous respiration via a face mask (Plasti-med Pediatric, Istanbul, Turkey) and an anesthetic circuit. The inspired sevoflurane was adjusted to aim for a predetermined end-tidal concentration through the face mask under spontaneous respiration to maintain sedation. This anesthesia technique was used in a recent study [6]. The target end-tidal concentration was determined by the Dixon up-and-down method. Once the target end-tidal concentration had been achieved and had remained stable for at least 10 min, the MRI scan was initiated, and the child was evaluated by an observer blinded to the concentration of sevoflurane. Awakening was defined as eye opening, onset of continued purposeful movements or phonation at any time after the time-point of reaching the target end-tidal concentration, up until the MRI procedure was completed. Using the Dixon up-and-down method each target concentration was determined by the response of the previous child in the same group. If the previous child had awakened, the target concentration was set at 0.2% higher than the previous target. If the previous child had not responded then the target was set 0.2% lower. In each group the initial concentration was set at 1.2% according to our preliminary evaluations. Sevoflurane was stopped 2 min before completion of imaging in all patients.
Heart rate, mean arterial pressure, hemoglobin oxygen saturation (SpO2) and degree of sedation were recorded every 5 min from the time of induction until leaving the scanner. Additional anesthetic needs, time to first spontaneous arm or leg movement, time to spontaneous eye opening, time to achieve criteria for discharge from the post-anesthesia care unit (PACU), hospital discharge time and complications (nausea, vomiting, agitation, laryngospasm, bronchospasm, desaturation defined as SpO2 <90%) were also recorded.
The ED50 values for MAC-awake (the minimum alveolar, or end-expiratory, concentration of an inhaled anesthetic at which 50% of patients do not show an appropriate response to command) in the two groups were estimated using the probit model. The hypothesis that there will be a difference between the ED50 estimates for the two groups was tested using the testnl command in Stata 10 (StataCorp, College Station, TX). This is a Wald-type test of smooth nonlinear hypotheses about the estimated parameters.
Previous MAC-awake studies using the up-and-down technique have demonstrated only small degrees of variation. Therefore it was assumed that it would be enough to determine the level consistently for five changes in each direction. The sample size was calculated as 13 patients per group based on an effect size d of 1.5 in ED50 score, an α error of 0.05, and a minimum power 95% in a two-tailed test. Groups were compared using the Mann-Whitney U test or chi-square test. A P value <0.05 was considered as statistically significant.
Results
Included in the study were 28 children undergoing MRI procedures. There were 14 boys and 14 girls, ranging in age from 15 months to 8 years. Both groups were comparable in terms of patient characteristics (Table 1). Indications for MRI were an intraabdominal mass, spine problems (spina bifida, cauda equina, evaluation following spine surgery), acute hematogenous osteomyelitis and diplopia. No child experienced clinically significant hemodynamic changes during the study. There were no statistically significant differences between groups regarding ASA physical status, duration of the MRI procedure, anesthesia time, hemodynamic variables, respiration rate, end-tidal CO2 or SpO2 throughout the study period.
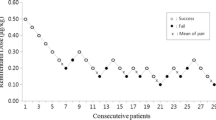
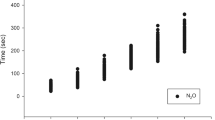
The up/down progression of children with headphones and without is shown in Fig. 1 and a photograph of a child wearing headphones is shown in Fig. 2. The calculated ED50 values for MAC-awake in each group are shown in Table 1. There was a significant difference in ED50 between the two groups (P < 0.001).
End-tidal sevoflurane concentrations in patients with and without headphones derived using the Dixon up-and-down technique. The squares represent individual patients, with the black squares representing a positive response (movement) and the white squares representing no response. Five consecutive responses were accepted as the anesthetic requirement for MRI. MAC Minimum alveolar concentration, X-axis Consecutive patient
Times to spontaneous arm and leg movements, eye opening and discharge from recovery were significantly shorter in children with headphones than in those without (P < 0.001; Table 1, Fig. 1). However, there was no difference in times to hospital discharge (P = 0.056). None of the patients experienced clinically significant hemodynamic changes or complications during the study. Patients did not require airway, endotracheal intubation or a laryngeal mask airway.
Discussion
In this study the wearing of very basic noise-concealing headphones during MRI scans led to decreases in the amount of inhalation anesthetics required to keep the children immobile, and the times to recovery from anesthesia (eye opening, spontaneous movement) and discharge from the PACU were also shorter in children wearing the headphones. However, the times to discharge from hospital were not different between children with and without headphones.
Acoustic noise produced by MRI scans is very disturbing and loud. When an MRI system is in use, electric current pulses through the gradient coil to create a magnetic field that interacts with the unit’s static magnetic field. This interaction causes the gradient coil’s support structure to vibrate, generating the disturbing acoustic noise. New MRI machines with higher strength (more powerful gradients) have even louder acoustic noise levels than older generation machines [4, 7]. The amount of acoustic noise produced by an MRI scanner is equivalent almost to a rock concert or gun shot. The Occupational Safety and Health Administration has set guidelines for dangerous sound levels, beginning at 90 dB and not exceeding 105 dB [8, 9]. This is basically similar or in some cases lower than the acoustic noise generated by an MRI machine. Considering the duration of MRI scans some precautions are needed to mitigate the deleterious effects of the acoustic noise on the patient. This kind of loud acoustic noise can induce tinnitus, hypertension and tachycardia [10–12]. In children this is even more important since the noise may cause the child to move, leading to the scan being paused or even stopped. Prolonging the scan process causes loss of valuable scan time and increases costs.
MRI-compatible headphones and even video systems have been utilized to decrease the need for sedation, but these have had limited success [13]. The use of an MRI simulator and also making the environment more child-friendly have helped children tolerate the process [14, 15]. However, children younger than a certain age still require sedation or general anesthesia. In this study, we used general anesthesia with a previously defined technique using a noninvasive method (a face mask) to maintain anesthesia. In a previous study [6], we demonstrated that this technique provides adequate anesthesia in spontaneously breathing patients without complications and is the anesthetic technique of choice for MRI at our institution. This technique allows early recovery and discharge, improving the turn-over time in the MRI suite. In our previous study [6], different concentrations of sevoflurane were evaluated with the same anesthetic technique. In the previous study, the group receiving a high concentration of sevoflurane (1.5%) had a recovery time similar to that in the no-headphone group in this study. However, the headphone group in this study had a significantly shorter recovery time (53 vs. 32 s). The use of headphones decreased the amount of sevoflurane needed to keep patients immobile.
Dixon’s up-and-down method is a commonly used technique for determining anesthetic requirements [16, 17]. Assessing dose responses in the evaluation of the effects of a drug is very common, and conventional techniques usually require substantially higher numbers of subjects. The up-and-down technique has been demonstrated to yield similar results with far fewer subjects [16]. This technique uses a unit-sequential method of testing; the level of the variable under study is raised or lowered depending on the outcome of the previous test. Sequential design methods for binary response variables are used to determine the concentration or dose associated with the 50% point along the dose–response curve, and the up-and-down method of Dixon and Mood is now commonly used in anesthesia research. Many anesthesia studies in which this technique has been used have also used logistic or probit regression analysis of the data as a sensitivity or backup analysis using commonly available logistic or probit regression software [16, 17]. To decrease the number of subjects required for this study we also used this well-established technique.
There are number of limitations in this study. The most important limitation was the blinding process. Although the sevoflurane vaporizers were covered to conceal the allocated concentration according to the Dixon up-and-down technique, we were unable to blind headphone use. An independent observer blinded to group and concentration of sevoflurane evaluated the patients. The observer was also not aware of the primary aim of the study. We believe that these precautions provided significant blinding. An important concern may be that headphones were not used in the control group, that this could have been considered unethical. However, we made sure that the children in this group received adequate anesthesia and were comfortable through the procedure.
Conclusion
We demonstrated a significant reduction in sevoflurane requirements in children undergoing an MRI scan using simple acoustic noise-concealing headphones. This reduction led to earlier recovery and a decrease in the time spent in the PACU. We would recommend the routine use of headphones in children undergoing an MRI scan.
References
Schulte-Uentrop L, Goepfert MS (2010) Anaesthesia or sedation for MRI in children. Curr Opin Anaesthesiol 23:513–517
Serafini G, Zadra N (2008) Anaesthesia for MRI in the paediatric patient. Curr Opin Anaesthesiol 21:499–503
Beauve B, Dearlove O (2008) Sedation of children under 4 weeks of age for MRI examination. Paediatr Anaesth 18:892–893
Hattori Y, Fukatsu H, Ishigaki T (2007) Measurement and evaluation of the acoustic noise of a 3 Tesla MR scanner. Nagoya J Med Sci 69:23–28
Harned RK 2nd, Strain JD (2001) MRI-compatible audio/visual system: impact on pediatric sedation. Pediatr Radiol 31:247–250
Oğurlu M, Orhan ME, Bilgin F et al (2010) Efficacy of different concentrations of sevoflurane administered through a face mask for magnetic resonance imaging in children. Paediatr Anaesth 20:1098–1104
McJury M, Shellock F (2000) Auditory noise associated with MR procedures: a review. J Magn Reson Imaging 12:37–45
Occupational Safety and Health Administration (OSHA) Occupational noise exposure, 29 CFR, Part 1910.95 (1988)
Food and Drug Administration (1988) Magnetic resonance diagnostic device: panel recommendation and report on petitions for MR reclassification. Federal Register 53:7575–7579
Brummett RE, Talbot JM, Charubas P (1988) Potential hearing loss resulting from MR imaging. Radiology 169:3539–3540
Quirk ME, Letendre A, Ciottone RA et al (1989) Anxiety in patients undergoing imaging. Radiology 170:463–466
Brennan SC, Redd WH, Jacobsen PB et al (1988) Anxiety and panic during magnetic resonance scans. Lancet 2:512
Lemaire C, Moran GR, Swan H (2009) Impact of audio/visual systems on pediatric sedation in magnetic resonance imaging. J Magn Reson Imaging 30:649–655
Raschle NM, Lee M, Buechler R et al (2009) Making MR imaging child’s play – pediatric neuroimaging protocol, guidelines and procedure. J Vis Exp (29),e1309. doi:10.3791/1309
de Bie HM, Boersma M, Wattjes MP et al (2010) Preparing children with a mock scanner training protocol results in high quality structural and functional MRI scans. Eur J Pediatr 169:1079–1085
Davidson AJ, Wong A, Knottenbelt G et al (2008) MAC-awake of sevoflurane in children. Paediatr Anaesth 18:702–707
Hui MT, Subash S, Wang CY (2011) The 50% and 95% effective doses of desflurane for removal of the classic laryngeal mask airway in spontaneously breathing anaesthetised adults. Anaesthesia 66:274–277
Conflicts of interest
The authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oğurlu, M., Orhan, M.E., Çinar, S. et al. Effect of headphones on sevoflurane requirement for MRI. Pediatr Radiol 42, 1432–1436 (2012). https://doi.org/10.1007/s00247-012-2463-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-012-2463-6