Abstract
Background
The radiologic evaluation of Hirschsprung disease is well described in the literature. However, there is a paucity of literature describing the appearance of the neo-rectum and colon after repair, specifically describing findings in patients with poor functional outcome, which would suggest the need for reoperation.
Objective
We describe findings on contrast enema and correlate them with surgical findings at reoperation in children with poor functional outcome after primary repair for Hirschsprung disease who suffer from bowel dysfunction that can manifest with either soiling or obstructive symptoms such as enterocolitis.
Materials and methods
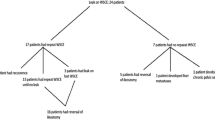
Children were identified from our colorectal surgery database. At the time of abstract submission, 35 children had contrast enemas prior to reoperation. Additional children continue to present for evaluation. The majority of children included in the study had their primary repair performed elsewhere. The initial procedures included: Duhamel (n = 11), Soave (n = 20) or Swenson (n = 3). One child had undergone a primary Soave repair and subsequently had a Swenson-type reoperation but continued to have a poor outcome. One child’s initial surgical repair could not be determined. Images were reviewed by a staff pediatric radiologist and a pediatric radiology fellow.
Results
Findings encountered on contrast enema in these children include a distal narrowed segment due to stricture or aganglionic/transitional zone segment (8), dilated/hypomotile distal segment (7), thickened presacral space due to compressing Soave cuff (11), dilated Duhamel pouch (8), active enterocolitis (3) and partially obstructing twist of the pull-through segment (1).
Conclusion
Multiple anatomical and pathological complications exist that can lead to bowel dysfunction in children after repair of Hirschsprung disease. Little recent literature exists regarding the radiographic findings in children. We had the opportunity to review a substantial series of these children, describe the contrast enema findings in these difficult cases and correlate them with operative findings. Radiologic evaluation is key to assessing such patients; it defines the potential anatomical problem with the pull-through and facilitates surgical planning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most radiologists, both general and pediatric-trained, are knowledgeable about the assessment of Hirschsprung disease on a contrast enema when a neonate fails to pass meconium or presents with difficulty passing stools. The radiographic assessment of children with Hirschsprung disease who have a poor functional outcome following their surgical repair is less well studied in the radiology literature. In this review, we evaluated a series of children who had a poor functional outcome after primary surgical repair of Hirschsprung disease and who subsequently presented to our Colorectal Center with symptoms we deemed needing surgical intervention. We describe contrast enema findings of these children and correlate them with operative findings.
Materials and methods
After obtaining IRB approval, we conducted a retrospective review of all reoperations in children with Hirschsprung disease from July 2004 to July 2009. Children were identified from our hospital’s surgical database. The radiology records of these children were reviewed to identify those who had a contrast enema performed prior to reoperation in our department. Thirty-four children were identified as fitting these parameters. One child had been reoperated on twice, yielding 35 enema-surgery pairs for review. The children’s clinical records, including operative findings and pathology results, were obtained. Children were categorized by the operative technique of previous repair: Swenson, Soave or Duhamel. When the child had undergone multiple prior operations for the repair of Hirschsprung disease, they were assigned to the category of their most recent operation. The contrast enemas were reviewed by two pediatric radiologists, one fellow and one staff member. When possible, gross surgical photographs of the findings were obtained to correlate with the enema findings. Pathology results were reviewed for the presence of retained aganglionic bowel or transition zone. The enemas were evaluated for the presence of a narrowed or stenotic distal segment, thickened or obstructing Soave cuff denoted by presacral thickening, dilated or impacted Duhamel pouch, twisting of the distal pull-through segment, dilated/immotile distal colonic segment or findings suggesting active enterocolitis. If the child had multiple enemas, the most recent study preceding the last operation was evaluated. All enemas were performed in our department.
The enemas performed on this patient population utilized water-soluble, ionic, iodinated contrast, CystoConray II, 17.2 % (Mallinckrodt/medical, St Louis, MO, USA). Non-balloon tip, infant/child size rectal tubes were used. A supine scout radiograph of the abdomen and pelvis was performed prior to the enema. Standard views obtained included initial left lateral fluoroscopic view of the rectum and sigmoid colon obtained during maximal distension, fluoroscopically monitoring during filling so as not to under- or overdistend the distal colon. Next, a frontal fluoroscopic spot view of the optimally distended rectosigmoid colon was obtained in the supine position. The colon was then filled just to the cecum with the child in the prone position and contrast filling discontinued. Retrograde filling of the small intestine is deemed a suboptimal finding since it may obscure colonic findings. An abdominal radiograph including the entire colon was then performed. The child was then allowed to spontaneously evacuate as much as possible; then the final, post-evacuation radiograph of the entire abdomen was obtained. If the child was unable to evacuate the contrast effectively, the colon was drained as much as possible to avoid complications related to slightly hyperosmotic contrast remaining in the colon, namely, dehydration.
Results
Of the 34 children, 26 were male and 8 female. The children’s ages ranged from 17 months to 15 years, 7 months, with a mean of 5 years, 7 months. Children were classified by previous operative repair: 3 Swenson repairs, 20 Soave repairs and 11 Duhamel repairs. One child’s initial repair could not be determined. Enema findings included distal rectal narrowing in 8 (Fig. 1), dilated/immotile distal colonic segment in 7 (Fig. 2), thickening of the presacral space/presumed Soave cuff in 11 (Figs. 3 and 4), dilated/impacted perirectal bowel segment/Duhamel pouch in 8 (Figs. 5 and 6), a fixed twisted pull-through segment causing narrowing in 1 (Fig. 7) and active enterocolitis in 3 (Fig. 8). Pathology revealed that 8 cases with radiographic distal narrowing had retained aganglionic bowel or transition zone pathology (excluding Duhamel procedures in which a retained aganglionic pouch is intentional).
Post Swenson pull-through with pathologically proven retained aganglionic segment in a 1-year-old boy. a. Frontal fluoroscopic spot image shows narrowing of the distal colon relative to the more proximal segment (arrows). b Lateral fluoroscopic spot image shows similar findings of a transition from a narrow, short distal rectal segment compared to adjacent proximal segment. c Gross surgical photo of colon during reoperation after initial Swenson pull-through. Note small caliber of distal segment and caliber change (arrows), a nice correlation with enema findings
Example of massive dilation in the distal remaining bowel after primary repair of Hirschsprung disease in a 5-year-old boy. This dilated distal segment is immotile/hypomotile, leading to an inability to stool. Note the colon proximal to the dilated segments is of relatively normal caliber. Often, this segment is impacted with stool, too large to be evacuated spontaneously, requiring manual disimpaction
Obstructing Soave cuff in a 2-year-old boy. a Frontal fluoroscopic spot image shows circumferential narrowing of distal segment with prominent “shoulder” transition to distended proximal colon. b Lateral fluoroscopic spot image shows circumferential narrowing of distal segment with prominent “shoulder” (dotted lines) transition to distended proximal colon and widening of the presacral space
Obstructing Soave cuff in a 1-year-old boy. a Frontal overhead view of full colon from contrast enema shows narrowed distal segment. b Lateral fluoroscopic spot view from contrast enema shows widening of the presacral space and narrowed distal segment. c Gross surgical photo during repair shows thickened rim of tissue at the distal end of the mobilized colon representing the area of narrowed pull-through (black arrows) due to the obstructing retained cuff (white arrows)
Impacted Duhamel pouch in an 8-year-old boy. a Lateral fluoroscopic spot image from contrast enema shows large Duhamel pouch with fecal impaction. b Frontal post enema image from contrast enema shows large Duhamel pouch with fecal impaction. c Gross surgical photo shows the appearance of the distended pouch, which correlates nicely with the enema findings
Twisted pull-through segment in a 5-month-old boy. a Frontal fluoroscopic spot image shows narrow distal pull-through segment. b Lateral fluoroscopic spot image shows narrow distal pull-through segment, which appears twisted. c Gross surgical photo shows greater than 180-degree twist in distal bowel
Discussion
In 1888, Harald Hirschsprung, a Danish pediatrician, first described this disease in two unrelated boys who died from chronic severe constipation and abdominal distention resulting in congenital megacolon [1]. Hirschsprung disease is a congenital disorder characterized by the absence of intramural enteric ganglia of the myenteric and submucosal plexuses along a variable length of intestine. Characteristically, it involves the distal colon and a variable length of contiguous proximal colon; in some cases it can involve the entire colon and, in rare cases, the entire intestinal tract. Patients with Hirschsprung disease usually have difficulty stooling, leading to abdominal distention. This typically starts at birth. The radiologic work-up for symptoms of difficulty stooling includes a contrast enema. The classic finding that suggests Hirschsprung disease on enema is smaller caliber of the rectum as it relates to the sigmoid colon. When this finding is present, confirmation of the diagnosis is made by rectal biopsy, which characteristically demonstrates the absence of ganglion cells and hypertrophied nerves. During operative treatment for Hirschsprung disease, serial biopsies are performed progressing proximally in the colon until the level of normal colonic histology is attained. The diseased colon is either completely or partially removed, with the anal canal and sphincter mechanism preserved. The more proximal “normal” bowel is then pulled through to the anal canal. Repair can be completed in a single operation or in a staged procedure with interval colostomy if the child is very ill with enterocolitis. Three dominant surgical procedures exist for repair of Hirschsprung disease: Soave, Swensen and Duhamel. Today, the repair can be done transanally or with the assistance of laparoscopy.
The guiding principles utilized by our Colorectal Center in evaluating patients surgically treated for Hirschsprung disease are: (1) they should stool spontaneously and (2) they should be able to remain clean and dry [2]. When there is a poor outcome after surgical treatment of Hirschsprung disease and these goals are not achieved, the major clinical symptoms come in two forms, soiling or obstruction. Abdominal bloating or distension and often recurrent bouts of enterocolitis and failure to thrive may be due to partial obstruction to colonic emptying. Soiling may result from anatomically induced impaction or from an injury to the anal canal or sphincters. Patients undergo an extensive clinical work-up with thorough clinical history and physical examination including a detailed history of current and past stooling patterns. They undergo an examination of the area of surgery under anesthesia by experienced colorectal surgeons and a rectal biopsy to evaluate for the presence of residual Hirschsprung disease histology. They also undergo a preoperative contrast enema, the results of which are discussed here.
The three classic surgical techniques for the repair of Hirschsprung disease are the Swenson, Soave and Duhamel procedures. All are predicated on removing or bypassing the distal aganglionic segment of colon. All have undergone various modifications from their original description and they are presented here as a basic overview.
In 1948, Orvar Swenson defined his original technique of open resection of the distal segment of diseased colon: full thickness dissection of the distal rectum with primary anastomosis of the more dilated proximal portion near the anal sphincter [3]. Originally, this required open laparotomy, but various improvements have allowed for laparoscopic and transanal approaches to this technique. The transanal Swenson pull-through is the favored procedure at our hospital because it is the only technique that removes all aganglionic bowel (Fig. 9). It is the typical surgery performed for reoperation of Hirschsprung disease [2].
Schematic diagram of the Swenson pull-through, which involves full thickness dissection of the distal rectum resulting in little or no significant widening of the presacral space (black arrows) on the lateral rectal view on contrast enema (Diagram courtesy of Glenn Minano, Cincinnati Children’s Hospital)
The Duhamel procedure, first described in 1956, involves partial resection of the aganglionic bowel with side-to-side anastomosis between the proximal normal colon and the defective aganglionic rectal segment (Fig. 10); this technique utilized a portion of the retained aganglionic pouch for absorptive capacity [4]. In 1966, Franco Soave described the technique of performing a partial circumferential mucosal/submucosal dissection of the distal aganglionic bowel and pulling the functional segment through the lumen of the distal aganglionic segment [5] (Fig. 11). Some portion of the distal aganglionic segment, of variable thickness, remains as a cuff surrounding the pull-through segment. This technique can be performed open (transabdominally) or via transanal approach.
Schematic diagram of Duhamel pull-through, which involves partial resection of the aganglionic bowel with side-to-side anastomosis between the proximal normal colonic segment (black arrowheads) and the defective aganglionic rectal segment (black arrows) (Diagram courtesy of Glenn Minano, Cincinnati Children’s Hospital)
Schematic diagram of Soave pull-through, which involves performing a partial circumferential mucosal/submucosal dissection of the distal aganglionic bowel (black arrows) and pulling the functional segment through the lumen of the distal aganglionic segment. Some portion of the distal aganglionic segment remains as a cuff surrounding the pull-through segment, appearing as variable widening of the presacral space on the lateral view (arrowheads) at contrast enema (Diagram courtesy of Glenn Minano, Cincinnati Children’s Hospital)
A satisfactory appearance of the distal colon on contrast enema after successful Hirschsprung repair is shown in Fig. 12; and the findings include absence of a distal transition zone, no presacral widening, absence of enterocolitis and fairly good clearance of contrast from the colon after spontaneous evacuation.
Soave procedure for primary repair of Hirschsprung disease in a 9-year-old girl. a Image shows lateral rectal view. Except for slightly incomplete distention of the distal rectum, the image demonstrates a satisfactory postoperative appearance. There is no significant presacral widening and no abnormal transition zone. b AP view of the neorectum again shows no abnormal transition zone. c AP view of entire colon filled and distended with contrast shows no significant transition zone and a normal configuration with normal haustra. d AP view of entire colon after spontaneous evacuation. There is satisfactory clearance of contrast and stool with some residual, a normal finding
Retained aganglionosis or transition zone
Each of these techniques can work well, but each, too, can have a poor functional outcome resulting in difficult stooling. The etiology of the poor functional result can be similar across each of the three operations, although there are specific reasons for poor outcome that can be ascribed to each of the techniques.
Each of the above described surgical techniques for repair of Hirschsprung disease can be complicated by incomplete resection of the aganglionic bowel during initial repair. This can result in a retained segment of aganglionic bowel or transition zone, resulting in functional bowel obstruction similar to the original pathophysiology of Hirschsprung disease. This result was found in eight of our patients. Pathologically, this was either due to absence of ganglion cells or to the presence of transition zone pathology demonstrated by the presence of ganglion cells but with accompanying hypertrophic nerves greater than 50 μm. In transition zone bowel, ganglion cells are present, but they may not be present around the entire circumference at this level or they may be present but have dysplastic innervation [6, 7]. A retained aganglionic segment may be suspected on enema if there is continued narrowing of the distal bowel segment with transition to proximal dilation, analogous to the altered rectosigmoid ratio in the initial diagnosis of Hirschsprung disease (Fig. 1). This is particularly common in the patient with recurrent episodes of enterocolitis after their pull-through. It is important to note that the site of radiologic transition zone does not correlate exactly with the pathological transition zone [8]. Therefore, good surgical technique involves resection somewhat higher than the radiologic and pathological level.
Dilated distal segment
Alternatively, the outcome of either of the surgical techniques may result in the distal remaining colon (or even the entirety of the remaining colon) becoming massively dilated and flaccid. These dilated segments are essentially immotile, which also leads to the inability to stool (Fig. 2).
Retained Soave cuff
The Soave procedure results in an aganglionic cuff of rectum surrounding the “normal,” pull-through bowel lumen. The length and thickness of this cuff is variable and depends on the specific surgeon’s technique. If the cuff was not adequately split or scars down, it can circumferentially narrow the distal bowel lumen and cause functional obstruction at the level of the cuff. This is evident on the enema by narrowing of the distal most segment and widening of the presacral space on the lateral views of the distal colon (Figs. 3 and 4). Often, there is an abrupt caliber change from the extrinsic compression, demonstrating a “shoulder” appearance.
Obstructing Duhamel pouch
The Duhamel segment, the distal aganglionic colon that is connected side-to-side to the normal pull-through segment, can stretch over time and become quite dilated, impacted with stool, and can attain a pouch-like configuration. This dilated, stool-filled pouch can then exert a mass effect, causing impingement upon the functional lumen, obstructing evacuation (Figs. 5 and 6).
Twisted pull-through
In one child, we observed a kinked, stenotic appearance of the distal pull-through segment (Fig. 7). At operation, this child was found to have a fixed, greater than 180-degree twist of the distal pull-through segment. This is a rare occurrence but has been reported in other series [9, 10].
Recurrent enterocolitis is a potential presenting symptom in undiagnosed Hirschsprung disease as well as in children who have been surgically repaired. The exact etiology of recurrent enterocolitis in children with Hirschsprung disease is still unknown but clearly relates to stasis, leading to bacterial overgrowth and then to secretory diarrhea. Enterocolitis is known to be a cause of significant morbidity and mortality in children with Hirschsprung disease [11–13]. If a child is known or suspected to have active enterocolitis, contrast enema is not performed. However, in three asymptomatic children, enema findings suggestive of enterocolitis were detected (Fig. 8). In these cases, the ordering clinicians were contacted to evaluate the children before they were discharged from the radiology department.
Certainly, when children present with bowel dysfunction after primary repair, nonoperative management strategies exist and are the preferred treatment [14, 15]. However, repeat pull-through operations have proven to be effective in improving stooling patterns for these children when less-invasive treatments are ineffective [1, 16–18]. Reoperations are particularly valuable for reparable anatomical and pathological problems as described in this report.
Some important technical aspects to our enema technique, which may or may not be utilized routinely elsewhere, warrant comment. First, it is important to obtain initial scout radiographs of the abdomen and pelvis to demonstrate the degree of fecal impaction. In addition, it is vital to obtain lateral filling images of the distal colon with maximal distension of the rectum (or whatever distal bowel remains). Underdistention will overestimate the presacral thickness potentially associated with a Soave cuff, and overestimate the degree of caliber change, overdiagnosing possible retained aganglionosis. In this regard, true lateral views (confirmed when there is overlapping of the femoral heads) of the distal segment will allow evaluation of the presacral space whereas degrees of obliquity will obscure findings in this location. Secondly, balloon tip catheters are not used as they may obscure a transition zone in the distal colonic segment in the region of the pull-through and could theoretically cause bowel perforation if a balloon is inflated blindly in the region of a distal narrowing or stricture [19]. Finally, enemas in our department are performed using CystoConray II 17 % iodinated contrast, which has an osmolality of approximately 400 mOsm/L. Slightly hyperosmotic contrast relative to body fluids is utilized to help clean out the colon due to the well-known effect of hyperosmotic fluid shift [20]. Anecdotally, there has been at least one child who had an enema-related complication due to dehydration after prolonged exposure to a hyperosmolar enema solution. This was a child who evacuated the colon poorly and required daily colonic irrigation at home. For that reason, in children who cannot spontaneously evacuate the majority of the contrast after a reasonable attempt, the colon is drained of as much of the enema fluid as is possible even if this requires insertion of a Foley catheter and removal of fluid by syringe.
Conclusion
We have described and shown a variety of contrast enema findings that were correlated with operative findings in children presenting with poor functional outcome after primary repair of Hirschsprung disease requiring reoperation. A better understanding of the types of surgical repair and possible complications is important for radiologists who are assessing these children. The cases presented will hopefully help radiologists detect subtle findings on contrast enemas, which will promote consultation and assessment of these symptomatic patients by our surgical colleagues for potential reoperation.
References
Hirschsprung H (1888) Stuhlträgheit neugeborener infolge von dilatation und hypertrophic des colons. Jb Inderheilk 27:1
Levitt MA, Dickie B, Peña A (2010) Evaluation and treatment of the patient with Hirschsprung disease who is not doing well after a pull-through procedure. Semin Pediatr Surg 19:146–153
Swenson O, Bill A (1948) Resection of the rectum and rectosigmoid with preservation of the sphincter for benign spastic lesions producing megacolon. Surg 24:212–220
Duhamel B (1956) Une nouvelle opération pour le mégacolon congénital: L’abaissement rétrorectal et trans-anal du colon, et son application possible au traitement de quelques autres malformations. Press Méd 64:2249–2250
Soave F (1964) A new surgical technique for treatment of Hirschsprung’s disease. Surg 56:1007–1014
White F, Langer J (2000) Circumferential distribution of ganglion cells in the transition zone of children with Hirschsprung disease. Pediatr Dev Pathol 3:216–222
Kobayashi H, Hirakawa H, Surana R et al (1995) Intestinal neuronal dysplasia is a possible cause of persistent bowel symptoms after pull-through operation for Hirschsprung’s disease. J Pediatr Surg 30:253–257
Jamieson DH, Dundas SE, Belushi SA et al (2004) Does the transition zone reliably delineate aganglionic bowel in Hirschsprung’s disease? Pediatr Radiol 34:811–815
Langer JC, Durrant AC, de la Torre L et al (2003) One-stage transanal Soave pullthrough for Hirschsprung disease: a multicenter experience with 141 children. Ann Surg 238:569–583
Obermayr F, Szavay P, Beschorner R et al (2009) Outcome of transanal endorectal pull-through in patients with Hirschsprung’s disease. Eur J Pediatr Surg 19:220–223
Marty T, Seo T, Matlak M et al (1995) Gastrointestinal function after surgical correction of Hirschsprung’s disease: long-term follow-up in 135 patients. J Pediatr Surg 30:655–658
Vieten D, Spicer R (2004) Enterocolitis complicating Hirschsprung’s disease. Semin Pediatr Surg 13:263–272
Elhalaby EA, Coran AG, Blane CE et al (1995) Enterocolitis associated with Hirschsprung’s disease: a clinical-radiological characterization based on 168 patients. J Pediatr Surg 30:76–83
Bischoff A, Levitt MA, Bauer C et al (2009) Treatment of fecal incontinence with a comprehensive bowel management program. J Pediatr Surg 6:1278–1284
Keshtgar AS, Ward HC, Clayden GS et al (2003) Investigations for incontinence and constipation after surgery for Hirschsprung’s disease in children. Pediatr Surg Int 19:4–8
Schweizer P, Berger S, Schweizer M et al (2007) Repeated pull-through surgery for complicated Hirschsprung’s disease–principles derived from clinical experience. J Pediatr Surg 42:536–543
Teitelbaum DH, Coran AG (2003) Reoperative surgery for Hirschsprung’s disease. Semin Pediatr Surg 12:124–131
Pena A, Elicevik M, Levitt MA (2007) Reoperations in Hirschsprung disease. J Pediatr Surg 42:1008–1014
de Feiter PW, Soeters PB, Dejong CH (2006) Rectal perforations after barium enema: a review. Dis Colon Rectum 49:261–271
ACR manual on contrast media version 7 (2010) Contrast media in children. Available via http://www.acr.org/SecondaryMainMenuCategories/quality_safety/contrast_manual/Children.aspx. Accessed 17 June 2010
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garrett, K.M., Levitt, M.A., Peña, A. et al. Contrast enema findings in patients presenting with poor functional outcome after primary repair for Hirschsprung disease. Pediatr Radiol 42, 1099–1106 (2012). https://doi.org/10.1007/s00247-012-2394-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-012-2394-2