Abstract
Background
Videofluoroscopic swallowing study (VFSS) is considered to be the gold standard method in assessing the risk of aspiration. Not infrequently, children who undergo VFSS are on tube feeds.
Objective
To investigate the reliability of the findings of VFSS when a nasogastric tube is in place at the time of the study.
Materials and methods
A retrospective review of VFSS covered a 6.5-year period. This review included only patients who had studies performed both with and without a nasogastric tube in place. Ninety-two studies (46 with and 46 without a nasogastric tube) were assessed in 46 children (30 boys, 16 girls) with a mean age of 6.7 months. The VFSS checklist of findings included weak sucking, incoordination, nasopharyngeal reflux, valecular and pyriform sinus pooling, penetration, aspiration and associated cough or respiratory compromise. We compared the occurrence rates of these events between studies with and without a nasogastric tube.
Results
No significant statistical difference was found in the occurrence of the different swallowing events during VFSS in the two groups. The presence of a nasogastric tube does not significantly alter the association of cough; however, it shows a moderately significant (P = 0.06) higher incidence of clinical respiratory compromise if aspiration does occur (8.5% of aspiration events).
Conclusion
The presence of a nasogastric tube does not alter the findings of VFSS; however, it might increase the incidence of respiratory compromise when aspiration is present.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The videofluoroscopic swallowing study (VFSS) is commonly used in infants and children. It is considered to be the gold standard method for assessing the risk of aspiration [1]. The main aim of VFSS is to identify the food consistencies that can be safely swallowed by the child and to guide dietary management to reduce the likelihood of aspiration. Not infrequently, infants and children with feeding difficulties who undergo VFSS are on enteral feeds via a nasogastric tube (NGT). During a 6.5-year period a total of 1,964 VFSS procedures were performed in our department, of which 113 studies (5.8%) were performed with an NGT in place. Our study investigated the reliability of VFSS findings with an NGT in place.
Huggins et al. [2] conducted VFSS in 10 normal young adults and examined the effects of an NGT on their swallowing mechanisms. They concluded that NGTs slow swallowing, but do not alter its functions, namely clearance and airway protection. They also suggested that the NGT actually prevents aspiration by stimulating earlier closure of the laryngeal vestibule. This study only determined NGT effects on normal adults and the observations were limited to the short-term effects of NGT. Hiorns and Ryan [1] in their review of current practice in paediatric videofluoroscopy considered removing the NGT before conducting VFSS unnecessary in most cases. More recently, Leder and Suiter [3] examined the effects of NGT on the incidence of aspiration in two separate groups of patients with dysphagia, one with and one without an NGT [3]. They injected liquid and puree during a fiberoptic endoscopic evaluation of swallowing (FEES) and found no statistically significant difference in aspiration status. Their population sample was heterogeneous and did not reflect subjects at age extremes such as very young patients; in addition, they did not study NGT effects in the same individual.
Our study investigates the effects of an NGT on the oral and pharyngeal phases of swallowing in infants and children with swallowing dysfunction based on a comparison between similar food consistencies given orally with both an NGT tube present and not present in the same patient.
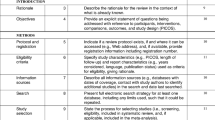
Materials and methods
Our institutionally approved review is a retrospective analysis of videofluoroscopic swallowing studies performed in a 6.5-year period (January 2002 to June 2008) using the VFSS assessment sheets completed by the radiologist at the time of the study and stored on our PACS. The actual video of the VFSS was not reviewed. Only children having studies done with and without NGTs were included. The score sheets of 92 studies were reviewed (46 children on two occasions, 30 boys and 16 girls), with each child having one study performed with and one without an NGT in place. Studies done with similar consistencies and with the closest intervals were chosen.
The findings noted on the VFSS assessment sheets included weak sucking, incoordination, nasopharyngeal reflux (NPR), valecular and pyriform sinus pooling, laryngeal penetration, tracheal aspiration and associated cough or respiratory compromise. In each child, the occurrence rates of each of the different events were estimated and compared between the studies done with and without an NGT.
The mean age of the children included in the review was 6.7 months at the time of their first study (2 weeks to 6.5 years) with 38 children (83%) being younger than 1 year of age. The time interval between the studies done with and without NGTs was 2 weeks to 18 months, with a mode of 3 months.
Most children had underlying medical conditions that might impair their swallowing mechanism, with genetic syndromes and post-cardiac and tracheo-oesophageal fistula surgery being among the commonest (Table 1).
The main indication of the second VFSS was to optimize the safest food consistency appropriate for the child’s age and nutritional and developmental status. In those having their first study done with an NGT, the study was repeated after the removal of the NGT to confirm the persistence of the findings.
The studies were conducted in conjunction with an occupational therapist and were performed on an Advantx SFX R/F unit (GE Healthcare, Waukesha, WI, USA) before January 2006, then on a pulsed fluoroscopic unit (Precision 500D; GE Healthcare, Waukesha, WI, USA) thereafter.
Results
Statistical analysis was performed using SPSS version 14.0. Table 2 summarises the results.
The mean age of patients without an NGT was 9.9 months compared to a mean age of 7.4 months for the group with an NGT (P value of 0.70).
Aspiration was found in 47 studies (51% of all studies). Twelve children had aspiration in studies done both with and without NGT, 16 children had aspiration only with an NGT and 7 only without an NGT with no significant differences noted between groups (P value = 0.22). Aspiration was silent in 40 studies (85%). In five studies, cough occurred with an NGT in place; in two studies, it occurred without an NGT (P value = 0.23). Respiratory desaturation occurred in four studies (4.3% of all studies) with all incidences occurring after aspiration (8.5%) and with an NGT in place (P value = 0.06). Three of the four patients with respiratory compromise were neonates with serious underlying medical conditions (two post-EA/TEF surgical repair and one with Cri du chat).
No significant statistical difference for laryngeal penetration was found (P = 0.34). Penetration was seen in 45 studies (49% of all studies). Eleven children had penetration in studies done both with and without an NGT, 13 had penetration with an NGT and 10 without.
Similarly, valecular and pyriform sinus pooling did not demonstrate any significant difference between the two groups (P values of 0.24 and 0.21, respectively). Nasopharyngeal reflux (NPR), incoordination and weak sucking also showed no significant statistical differences with P values of 0.38, 0.34 and 0.69, respectively.
Discussion
Feeding and respiration are fundamental activities essential for survival. These activities intersect in the upper aerodigestive tract, which represents one of the most complex neuromuscular units in the human body [4].
There are four phases of swallowing: the oral preparatory, oral, pharyngeal and oesophageal. These occur in three distinct anatomical regions, the oral cavity, pharynx and oesophagus.
VFSS (also called modified barium swallow) provides fluoroscopic evaluation of the unseen portion of swallowing. The patient is examined in a sitting or semi-sitting position and is orally given a range of fluid and food textures mixed with barium or other contrast media.
There are variable protocols regarding the correct order of presentation of the different food consistencies to be assessed. Some prefer to start with the safest consistency (puree/soft food), others prefer to start with the consistency that is least likely to cause residue after swallowing (liquids), while others prefer to start with a child’s favourite food to gain cooperation [1]. Most of the time, the texture about which there is most concern is the first to be examined.
Not infrequently, infants and children with feeding difficulties and swallowing disorders will have an NGT in place at the time of their feeding study, 5.7% of the VFSS in our experience. Most feeding tubes are made of a silastic material, which makes them smaller and softer than polypropylene gastric tubes.
Our data showed no significant statistical difference when correlating a child’s age with presence or absence of an NGT (P value of 0.70). This indicates a homogeneous age distribution and eliminates age as an effective variable.
Most abnormal swallowing events occur during the pharyngeal phase, aspiration being the most common in our series (51% of all studies) followed by penetration and valecular pooling (49% and 22%, respectively). Aspiration is defined as barium entering the airways and extending below the level of the vocal cords; the latter are marked by the inferior tips of the pyriform sinuses (Fig. 1) [5]. A nasogastric tube is thought to interfere with the anatomical integrity of the esophagus and partially obstruct its upper sphincter. It is also believed to repetitively stimulate the pharynx, causing desensitization of its reflexes and increasing the pharyngeal secretions [2, 6]. Theoretically, all of these factors would increase the incidence of aspiration; however, our data confirm Huggin’s and Leder’s results that no statistically significant effects of an NGT are found on the incidence of aspiration (P = 0.22) [2, 3]. Our study also shows that an NGT does not protect against aspiration, as Huggin’s previously suggested [2].
In our series, aspiration was silent in 85%, which is close to what is estimated in the literature (70–94%) [1]. This percentage would likely be even higher in children with neurologically based dysphagia. The presence of an NGT did not significantly alter the association of cough (P value of 0.23); however, it was associated with moderately significant (P = 0.06) higher incidence of respiratory compromise if aspiration did occur (8.5% of aspirations). Neonates and those with serious medical illnesses are at a higher risk of respiratory compromise during a VFSS. In our experience, the presence of a qualified nurse and pulse oximetry and functioning resuscitation equipment, including suctioning and oxygen delivery devices, are appropriate.
Laryngeal penetration occurs when contrast agent enters the airways, but does not extend below the level of the vocal cords. Its presence suggests incomplete airway protection. The differentiation between deep penetration and aspiration can sometimes be difficult. In our experience, it would be more common to misinterpret deep penetration as an aspiration rather than the opposite. The visualization of barium coating the upper trachea is a frequent indicator of aspiration. The presence of an NGT showed no significant statistical difference in the status of penetration (P = 0.34).
If there are difficulties in sensory awareness or problems with timing and coordination, contrast medium will remain in the pharynx during periods of airway opening. This is seen as valecular and pyriform sinus pooling, which is a high-risk situation for a delayed penetration or aspiration (Fig. 2). It was shown that the duration of both pharyngeal response and transit will increase with an NGT in place [2]. One would assume this would increase the incidence of pooling; however, no significant differences were found in our study (P values of 0.24 and 0.21 for valecular and pyriform pooling, respectively) or in Huggin’s study [2].
Children unable to elevate the soft palate (neurologically impaired) experience nasopharyngeal incoordination and reflux (Fig. 3) [7]. NGTs were shown to prolong the duration of velar elevation [2]; however, in our series there was no significant difference in the incidence of nasopharyngeal reflux in the presence or absence of an NGT (P = 0.38).
In the oral phase, the abnormality might have an anatomical aetiology such as cleft lip and palate, micrognathia or macroglossia or be related to sucking or oral motor dysfunction. The maturation of sucking and swallowing in infants can be summarized by increased sucking and swallowing rates, longer sucking bursts and larger volume per suck [4]. Preterm infants born before 34 weeks of gestational age have poor muscular tone and minimal energy reserve and lack coordination between sucking, swallowing and breathing. Children on long-term tube feeding are unused to oral feeding and might simply refuse to eat. Those with severe neurological impairment might be unable to suck or lack sufficient tongue control.
In regard to the relation between food texture and aspiration, it is widely believed that food viscosity is inversely proportional to the likelihood of aspiration [8]; however, this might not be the rule in children with underlying neurological diseases or those with valecular and pyriform sinus pooling, the latter being more common with thicker consistencies. Of the 92 studies we reviewed, only 6 studies in 4 children didn’t follow this rule. Interestingly, three of those children showed significant pooling.
Although our review suggests that NGTs do not increase the risk of aspiration, this doesn’t mean that they do not carry a higher risk for aspiration pneumonia. It is believed that the presence of an NGT predisposes a patient to contamination of the pharyngeal secretions by Gram-negative bacteria, which if aspirated can cause contamination of the lower respiratory tract [6, 9].
By comparing VFSS performed in the same individual, we tried to eliminate effects from many variables including age, sex and underlying medical condition; however, there were other factors we could not control, such as the severity of the underlying illness at times of VFSS and lack of standardised protocols in relation to consistencies, order of presentation, modalities of introduction (spoon, cup, straw, etc.) and bolus volumes. A prospective study conducting VFSS with tube-in and tube-out conditions during the same session would be the best way to negate these and other variables. Observer variations and lack of standardized terms and methodology remain a continuing problem in the interpretations of VFSS [10].
Conclusion
A nasogastric tube does not alter the findings of VFSS and does not increase the risk of aspiration; however, it might increase the incidence of respiratory compromise when aspiration is present.
References
Hiorns MP, Ryan MM (2006) Current practice in paediatric videofluoroscopy. Pediatr Radiol 36:911–919
Huggins PS, Tuomi SK, Young C (1999) Effects of nasogastric tubes on the young, normal swallowing mechanism. Dysphagia 14:157–161
Leder SB, Suiter DM (2008) Effect of nasogastric tubes on incidence of aspiration. Arch Phys Med Rehabil 89:648–651
Rogers B, Arvedson J (2005) Assessment of infant oral sensorimotor and swallowing function. Ment Retard Dev Disabil Res Rev 11:74–82
Cohen RA, Kuhn JP (2008) Larynx and cervical trachea. In: Slovis TL (ed) Caffey’s pediatric diagnostic imaging, 11th edn. Mosby, Philadelphia, pp 1068–1077
Gomes GF, Pisani JC, Macedo ED et al (2003) The nasogastric feeding tube as a risk factor for aspiration and aspiration pneumonia. Curr Opin Clin Nutr Metab Care 6:327–333
Glass RB (2008) The esophagus. In: Devos AS, Blickman JG (eds) Radiological imaging of the digestive tract in infants and children, 1st edn. Springer, New York, pp 81–107
Kuhlemeier KV, Palmer JB, Rosenberg D (2001) Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphagia patients. Dysphagia 16:119–122
Mamun K, Lim J (2005) Role of nasogastric tube in preventing aspiration pneumonia in patients with dysphagia. Singapore Med J 46:627–631
Ott J (1998) Observer variation in evaluation of videofluoroscopic swallowing studies: a continuing problem. Dysphagia 13:148–150
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alnassar, M., Oudjhane, K. & Davila, J. Nasogastric tubes and videofluoroscopic swallowing studies in children. Pediatr Radiol 41, 317–321 (2011). https://doi.org/10.1007/s00247-010-1834-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-010-1834-0