Abstract
Background
CT scans of the brain, sinuses and petrous bones performed as the initial imaging test for a variety of indications have the potential to expose the eye-lens, considered among the most radiosensitive human tissues, to a radiation dose. There are several studies in adults discussing the reduction of orbital dose resulting from the use of commercially available bismuth-impregnated latex shields during CT examinations of the head.
Objective
To evaluate bismuth shielding-induced artefacts and to provide suggestions for optimal eye-lens shielding in paediatric head CT.
Materials and methods
A bismuth shield was placed over the eyelids of 60 consecutive children undergoing head CT. Images were assessed for the presence and severity of artefacts with regard to eye-shield distance and shield wrinkling. An anthropomorphic paediatric phantom and thermoluminescence dosimeters (TLDs) were used to study the effect of eye lens-to-shield distance on shielding efficiency.
Results
Shields were tolerated by 56/60 children. Artefacts were absent in 45% of scans. Artefacts on orbits, not affecting and affecting orbit evaluation were noted in 39% and 14% of scans, respectively. Diagnostically insignificant artefacts on intracranial structures were noted in 1 case (2%) with shield misplacement. Mean eye-lens-to-shield distance was 8.8 mm in scans without artefacts, and 4.3 mm and 2.2 mm in scans with unimportant and diagnostically important artefacts, respectively. Artefacts occurred in 8 out of 9 cases with shield wrinkling. Dose reduction remained unchanged for different shield-to-eye distances.
Conclusion
Bismuth shielding-related artefacts occurring in paediatric head CT are frequent, superficial and diagnostically insignificant when brain pathology is assessed. Shields should be placed 1 cm above the eyes when orbital pathology is addressed. Shield wrinkling should be avoided.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Increasing awareness of the association between radiation-induced health detriment and levels of childhood radiation has renewed the interest in modification of techniques during paediatric CT [1]. CT scans of the brain, sinuses and petrous bones performed as the initial imaging test for a variety of indications, including trauma, suspected tumour, complicated infectious and inflammatory conditions, as well as suspected congenital abnormalities have the potential to expose the eye-lens, considered among the most radiosensitive human tissues [2, 3]. The eyes of children are more radiosensitive than previously considered, with significantly smaller threshold values for ophthalmologically detectable lens opacities causing cataract when compared to adults [4]. In particular, there is evidence of both cortical and posterior subcapsular cataract at doses somewhat lower than expected among A-bomb survivors and a group of children treated for skin haemangioma [5, 6]. Therefore, regarding paediatric head CT, every effort should be made towards appropriate and meticulous application of the “as low as reasonably achievable” (ALARA) principle, by reducing eye-lens doses without compromising diagnostic quality.
There are several studies in adults discussing the reduction of orbital dose resulting from the use of commercially available bismuth-impregnated latex shields during CT examinations of the head [7–11] and paranasal sinuses [12] that show differences in dose reduction factors, ranging from 18% to 50%, depending on the technique and material applied. There are few studies in children discussing dose reduction to the eye-lens due to bismuth shielding that revealed significant dose reduction ranging from 31% to 42% during brain and sinus scanning, while dose reduction was <1% during scanning with eye-sparing technique [13, 14]. In these dosimetric studies, most investigators briefly mention lack of diagnostically important artefacts, while two studies in adult sinus and brain CT, conducted a profile analysis on the CT density below the shield and found a statistically significant increase in noise [8–10, 12–16].
To our knowledge, extensive appreciation and grading of artefacts due to the presence of orbital bismuth shields in paediatric CT and proposals for artefact reduction resulting in suggestions on how bismuth latex shields should be used in children are not available in the literature. The aim of the current study was to assess the feasibility of application of shields and associated artefacts in a large cohort of children referred for head CT scans and to provide guidelines for optimal eye-lens shielding in children undergoing head CT with regard to elimination of artefacts and benefit from eye-lens dose reduction.
Materials and methods
Patient study
This study was in compliance with the Health Insurance Portability and Accountability Act and was approved by the Institutional Review Board of our institution. Patient’s guardians consented to the placement of shields during CT scanning. A commercially available bismuth shield (AttenuRad Radioprotective Garments, F&L Medical Products, Vandergrift, PA, USA) was placed over the eyelids of 60 consecutive children, age 5 weeks to 16 years (mean 6.8 years), referred for a medically indicated CT scan involving lens exposure. Shielding was possible in 56 children. Folded, sterile gauzes were interposed between the shield and the child’s closed eyelids for sanitary purposes (Fig. 1).
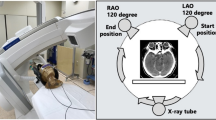
Scans were performed in a Siemens Somatom Sensation 16-slice CT scanner (Siemens, Forchheim, Germany) applying paediatric head protocols with reduced mAs, according to the manufacturer’s recommendations. Scans performed with a shield included 47 CT scans of the brain, 26 of which with sequential and 21 with spiral scanning techniques, 3 petrous bone scans, 5 sinus scans and 1 orbital scan; the latter 9 included the eye area, were performed with a spiral technique and were named limited spiral scans. The parameters of the scans were recorded and are listed in Table 1. Spiral scans of the brain required more effective mAs compared to limited spiral scans due to the need to eliminate posterior fossa artefacts in the former.
Assessment of artefacts
Artefacts were qualitatively assessed with a 5-point scale by two radiologists in consensus on soft-tissue window/levels, accordingly: 0 = no perceptible artefacts, I = artefacts restricted on the orbital areas, not considered to affect certainty for the evaluation or exclusion of orbital abnormality, II = artefacts on orbits, extending to intracranial structures, not considered to affect certainty for the evaluation or exclusion of orbital and intracranial abnormality, III = artefacts restricted on the orbital areas, considered to affect certainty for the evaluation or exclusion of orbital abnormality and IV = artefacts on orbits extending to intracranial structures, considered to affect certainty for the evaluation or exclusion of orbital and intracranial abnormality.
The distance lens-to-shield was measured on the images for each eye and the mean distance was recorded for each scan. Wrinkling of the shield was also assessed on the CT images as gross, moderate and no wrinkling.
Phantom study
To investigate the effect of distant versus direct shielding over the eyes on eye-lens dose reduction, a paediatric anthropomorphic phantom (Atom Phantoms, Cirs Norfolk, VA, USA) and thermoluminescence dosimeters (TLDs) were used. The head of the above phantom contains simulated intracranial structures, cranial bones and sinuses consistent with the head of a 5-year-old child. The phantom was subjected to four types of eye-exposing brain CT scans. These types included scanning performed without any shielding and scanning performed with shielding over 1, 2 and 4 interposed folded gauzes that elevated the shield away from the eyes by 0.5, 1 and 2 cm, respectively. Before each scan, two appropriately calibrated TLDs (TLD-100 3x3x0.9-mm chips, Harshaw, WI, USA) were placed on each eye. Scans were repeated 10 times for each type, to reduce the statistical error of the TLD readings. The mean dose of the four TLDs was considered as the eye-lens dose.
Results
Shielding was not possible in four children: 3 children ages 2, 3 and 3.5 years old refused the shield and one sedated 9-month-old child kept waking up upon shield placement and was finally scanned unshielded. Scanning with a shield was successfully completed in 56 children.
Absence of appreciable artefacts was noted in 25 scans (44.6%, Fig. 2). Artefacts were seen in 31 children (55.4%), type I in 22 (39.3%), and type II in 1 case with a cranially misplaced shield (1.8%) and type III in eight scans (14.3%). There were no artefacts classified as type IV. Type I artefacts were seen as mild increase in density over the anterior surface of the orbits (Fig. 3), while type III artefacts were seen as significant increase in density of superficial tissues, considered to affect the confidence for normality and for exclusion of haemorrhage or retinoblastoma on soft-tissue window settings (Fig. 4). All types of artefacts were considerably or totally eliminated on bone window settings (Figs. 2, 3 and 4).
CT scan of a 21-month-old boy with congenital cataract bilaterally, scanned to exclude retinoblastoma and bleeding. a Scout. The shield (arrow) is visible over the eyes. b Axial scan. There is absence of appreciable artefacts, despite the presence of the shield while the orbits and the lenses are well appreciated. c On bone window settings, there are no appreciable artefacts
Type I artefacts on CT brain images. a Axial scan through the orbits on soft-tissue window settings shows artefacts as increase in superficial orbital density (arrowheads). Note some horizontal streakiness at the level of the anterior border of sphenoid bones (arrow), considered to represent anterior fossa artefact, enhanced by the presence of the shield. Overall the orbital globes are confidently appreciated as normal. b Axial scan through the same level on bone window settings. Orbital artefacts are eliminated. There is moderate wrinkling of the shield at its left outer aspect
Type II artefacts on CT brain images. a Axial scan through the orbits on soft-tissue window settings. Type II artefacts are seen as significant increase in superficial orbital density behind the shield (arrowheads). The orbital globes cannot be confidently appreciated as normal. b Axial scan through the same level in bone window settings. The orbital artefacts are eliminated in this window and appreciation of the right lens (arrowhead) is feasible
The eye-lens-to-shield distance ranged from 1 mm to 23 mm (mean 8.8 mm) in scans with no artefacts, from 0 mm to 15 mm (mean 4.3 mm) in scans with type I artefacts and from 0 mm to 4 mm (mean 1.1 mm) in scans with type III artefacts. In the case with artefact at the anterior cranial fossa the distance was 11 mm. Distant shielding (a shield ≥10 mm away from the eyes) was performed in 17 children, in 12 children (70.6%) there were no artefacts, in 4 (23.5%) there were type I artefacts, in 1 child there were type II artefacts. Type III artefacts were absent in cases with distant shielding. Direct shielding (a shield ≤2 mm away from the eyes) was performed in 23 children, in 16 (69.6%) there were artefacts, type I in 10 and type III in 6. Intermediate shielding (a shield >2 mm and <10 mm away from the eyes) was performed in 16 children, in 10 (62.5%) there were artefacts, type I in 8 and type III in 2.
Artefacts were identified in 8 out of 9 scans (88.9%) where wrinkling occurred. Wrinkling of the shield was moderate (Fig. 2) in 7 scans, exhibiting type I artefact in 6 and type III in 1. Gross wrinkling was noted in 2 scans, both exhibited type III artefacts (Fig. 5). Artefacts were present in 21 out of the 47 scans (44.7%) where there was no appreciable wrinkling.
Axial CT scan through the orbits using soft-tissue window settings. The shield is severely wrinkled due to positioning of lateral pads for immobilization of this neonate’s head prior to the position of the shield. Type II artefacts are seen as increase in superficial orbital density behind the shield (arrowheads), considered to affect the evaluation of the orbital structures
All scans were thought to contain diagnostic information for the report (Fig. 6). Sino-nasal, orbital (Fig. 7) and mastoid pathology was adequately displayed. Coronal reconstructions were performed and exhibited no artefacts over the areas of interest. There were neither repeats of scans because of the shields nor lack of confidence in the diagnoses.
Axial CT scan through the skull base using soft-tissue window settings. There is an arachnoid cyst situated at the right middle fossa. Type I artefacts are seen as increase in superficial orbital density up to the level of the anterior border of the sphenoid bone (arrowhead) and are considered not to affect the diagnosis
a Scout view of a 9-month-old infant investigated for craniosynostosis, showing the shield (arrow). b Volume-rendered image following deletion of the pixels containing the shield, elegantly exhibits synostosis of the right coronal suture (arrow) with resulting orbital deformity, flattening of the adjacent forehead and scoliosis of the face
The factor of dose reduction when the shield was placed directly over the eyes of the paediatric phantom simulating a 5-year-old child was 32%. When the shield was placed 0.5 cm, 1 cm, and 2 cm away from the eyes of the same phantom, factors of dose reduction were 32%, 30% and 29%, respectively.
Discussion
The present study was motivated by the lack of data regarding thorough artefact evaluation following eye-lens bismuth shielding in children undergoing head CT and the possibility of their reduction, especially when investigating orbital pathology. The application of bismuth shields over the eyes of children undergoing CT that could potentially involve eye-lens exposure was generally feasible in a large cohort of children. Artefacts in the form of increase in density below the shield were frequently encountered, could be eliminated using bone window/level settings and were considered to be not significant and not affecting the diagnosis of intracranial pathology. In the single case with artefacts over the anterior cranial fossa, this increase in superficial density was considered the result of cranial displacement of the shield; therefore the shield, if correctly positioned over the eyes, is applicable in all cases when intracranial pathology is assessed. Our results are in accordance with dosimetric studies noting the presence of superficial orbital artefacts, only mentioning that shielding results in no diagnostic information loss [8–10, 12–15]. Paediatric radiologists have been trained to reduce tube current without reduction in the reader’s confidence [17]. Similarly, familiarization with bismuth-related artefacts by radiologists could play a role in accepting their presence routinely on paediatric head CT scans. Quantitative appreciation of the increase in orbital density, extending on average 10 mm beneath the shield has been demonstrated in adult studies, indicating a potential drawback of the shield when performing quantitative perfusion studies [12, 15]. These tests are, however, rarely performed in children.
When orbital morphology was particularly looked at, artefacts due to bismuth shielding considered to affect certainty for normality or exclusion of lesions were seen in 14.3% of scans in our series and in 26.1% of scans following placement of the shield directly (0–2 mm) over the eyes. The distance of the shield to the eyes appeared to play a role in the frequency and severity of artefacts, with practically fewer and less important artefacts when the shield was elevated ≥10 mm away from the eyes. This is in contrast with the guidelines of shield placement provided by Hopper [15], suggesting a tight seal over the nose without an air gap, using the adhesive material of the shield, in order to prevent the shield from overlying the orbital bone rim. Increasing the distance between the shield and the organ examined has been applied during scanning of the neck and chest, to increase rigidity of the shield. This increase in distance reduced artefacts and noise [9, 18, 19]. To our knowledge, such a technique has not been recommended for brain scanning either in adults, or in children. Our results suggest that increasing the lens-to-shield distance by 1 cm or more results in no or infrequent, diagnostically unimportant artefacts. Factors of dose reduction with distal shielding 0.5-, 1- and 2 cm away from the eyes were 32%, 30% and 29% respectively. When compared with the 32% of dose reduction following direct shielding, the application of distal shielding is justified when fine morphologic changes are looked for in the proximity of the shield [13]. Similar insignificant impact on measured doses has been shown in the application of spacers during adult chest and neck scanning [19]. In practice, artefacts that could affect the diagnosis of orbital pathologies could be eliminated by the interposition of two sterile gauzes between the eyes and the shield, without significantly compromising the protection provided by the shield. Two unfolded gauzes between the eyes and the shield correspond to approximately 1 cm between the eyes and the shield. Such indications in children would potentially include orbital trauma, retinoblastoma, inflammatory and other space-occupying lesions of the orbits.
In our study, artefacts were present in 83.3% of scans with wrinkling of the shield. Shield angulations, wrinkling, the presence of air gaps between the eyes and the shield and the presence of the shield over the bony orbital rim have been mentioned to cause artefacts on adult brain scans, although no numerical data are provided on the occurrence of artefacts in relation to the above conditions [8, 15]. In adults, positioning of the shield is considered simple, because the size of the shield is designed for adult orbital size. This is not true for neonates and infants, whose head size results in excess length of the shield. Two cases of gross shield wrinkling in neonates resulted in diagnostically important artefacts. Therefore, radiographers should take care to stretch the shield and place it flat over the child’s eyes, independently of the head size, also making sure that the shield is interposed between the primary beam and the eye lens.
Eye-sparing techniques have been known to result in lower doses to the eye lens in adult patients undergoing head CT, compared to single application of bismuth shielding and direct exposure of the lens [20, 21]. This has been also confirmed in children; therefore eye-sparing technique remains the most efficient measure of protection to the lens [10, 13]. This is the reason why radiographers should not, by any means, be distracted from employing eye-sparing techniques during paediatric head CT knowing that bismuth shields add protection to the eye lens. Moreover, it is with the eye-sparing technique that the eye-lens dose reduction factor due to the shield is small and therefore shielding is not necessary. With spiral scanning, due to z overscanning, an additional layer of tissue above and below the area to be imaged in also exposed with a strong possibility of direct eye-lens exposure despite planning of a strictly eye-sparing technique during spiral brain CT [22]. Consequently, sequential scanning is preferred over spiral scanning for paediatric brain CT at our institution, in order to ensure minimal exposure of the eye lens.
This study has focused only on the feasibility of orbital shielding in children, the incidence and significance of shield-related artefacts and the effect of shield elevation on eye-lens dose reduction and artefact elimination. We did not study the effect of modern tube current modulation on dose reduction. Individual tube current modulation has been increasingly applied as a tool to decrease dose and is considered superior to in-plane shielding in adults [16, 23, 24]. However, the dose reduction achieved with tube current modulation in neonates and young children has been found to be lower than that obtained for adults [25, 26]. Other authors recognize the potential of tube current increase due to shields [14]. However, it has been shown that Z-axis automatic tube current modulation combined with shielding slightly further reduces thyroid radiation dose during adult neck CT and during paediatric chest CT [23, 27]. Further studies are required to determine the optimal use or omission of orbital bismuth shielding during paediatric head CT using modern automatic tube current modulation with regard to dose reduction and artefact significance.
In our department, upon request for a CT scan, MRI instead of CT is recommended, regarded as the maximum means for radiation protection. In cases where CT is considered absolutely indicated, the CT practice following this study has been changed accordingly: the test is vetted, sequential scanning with an eye-sparing technique remains the technique of choice for routine paediatric brain CT and shields are not applied. In cases of spiral scanning, sinus scans and whenever the orbital structures are expected to be partly or totally included in the primary beam, shields are placed unwrinkled on the child’s eyes with one unfolded, sterile gauze interposed between the eyes and the shield. In case the clinical question focuses on orbital pathology, distant shielding is preferred and the eye-lenses are protected by placing a shield unwrinkled on the child’s eyes, with two unfolded, interposed sterile gauzes.
Conclusion
Orbital shielding during paediatric head CT is feasible in the vast majority of children. The eye-sparing technique remains the most efficient measure of protection to the lens, while in cases of spiral scanning, sinus scans and whenever the orbital structures are expected to be partially or totally included in the primary beam, shields should be placed on the patient’s eyes. Readers should be familiar with artefacts related to the bismuth shield that are frequent, restricted to the orbital areas and considered diagnostically insignificant when brain abnormalities are looked for. Shields should be placed 1 cm above the eyes when orbital pathology is particularly addressed in order to reduce the possibility of potentially significant artefacts without compromising the protective use of shields. Wrinkling of the shield is considered a cause of increased shield-related artefacts and should be meticulously avoided.
References
Brenner D, Elliston C, Hall E et al (2001) Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR 176:289–296
International Commission on Radiological Protection (1990) Recommendations of the international commission on radiological protection. In: ICRP Publication 60. Ann ICRP 21:1–3, Pergamon, Oxford
National Research Council (1990) Health effects exposure to low levels of ionizing radiation, BEIR V. National Academy, Washington
Merriam GR Jr, Focht EF (1957) A clinical study of radiation cataracts and the relationship to dose. Am J Roentgenol Radium Ther Nucl Med 77:759–785
Minamoto A, Taniguchi H, Yoshitani N et al (2004) Cataracts in atomic bomb survivors. Int J Radiat Biol 80:339–345
Hall P, Granath F, Lundell M et al (1999) Lenticular opacities in individuals exposed to ionizing radiation in infancy. Radiat Res 152:190–195
McLaughlin DJ, Mooney RB (2004) Dose reduction to radiosensitive tissues in CT. Do commercially available shields meet the users’ needs? Clin Radiol 59:446–450
Hopper KD, Neuman JD, King SH et al (2001) Radioprotection to the eye during CT scanning. AJNR 22:1194–1198
Colombo P, Pedroli G, Nicoloso M et al (2004) Evaluation of the efficacy of a bismuth shield during CT examinations. Radiol Med 108:560–568
Keil B, Wulff J, Schmitt R et al (2008) Protection of eye lens in computed tomography—dose evaluation on an anthropomorphic phantom using thermo-luminescent dosimeters and Monte-Carlo simulations. Rofo 180:1047–1053
Kim S, Yoshizumi TT, Frush DP et al (2009) Dosimetric characterization of bismuth shields in CT: measurements and Monte Carlo simulations. Radiat Prot Dosim 133:105–110
Hein E, Rogalla P, Klingebiel R et al (2002) Low-dose CT of the paranasal sinuses with eye lens protection: effect on image quality and radiation dose. Eur Radiol 12:1693–1696
Perisinakis K, Raissaki M, Theocharopoulos N et al (2005) Reduction of eye lens radiation dose by orbital bismuth shielding in pediatric patients undergoing CT of the head: a Monte Carlo study. Med Phys 32:1024–1030
Mukundan S Jr, Wang PI, Frush DP et al (2007) MOSFET dosimetry for radiation dose assessment of bismuth shielding of the eye in children. AJR 188:1648–1650
Hopper KD (2002) Orbital, thyroid and breast superficial radiation shielding for patients undergoing diagnostic CT. Semin Ultrasound CT MR 23:423–427
Geleijns J, Salvadó Artells M, Veldkamp WJ et al (2006) Quantitative assessment of selective in-plane shielding of tissues in computed tomography through evaluation of absorbed dose and image quality. Eur Radiol 16:2334–2340
Shah R, Gupta AK, Rehani MM et al (2005) Effect of reduction in tube current on reader confidence in paediatric computed tomography. Clin Radiol 60:224–231
Fricke BL, Donnelly LF, Frush DP et al (2003) In-plane bismuth breast shields for pediatric CT: effects on radiation dose and image quality using experimental and clinical data. AJR 180:407–411
Hohl C, Wildberger JE, Süss C et al (2006) Radiation dose reduction to breast and thyroid during MDCT: effectiveness of an in-plane bismuth shield. Acta Radiol 47:562–567
Yeoman LJ, Howarth L, Britten A et al (1992) Gantry angulation in brain CT: dosage implications, effect on posterior fossa artifacts, and current international practice. Radiology 184:113–116
Heaney DE, Norvill CA (2006) A comparison of reduction in CT dose through the use of gantry angulations or bismuth shields. Australas Phys Eng Sci Med 29:172–178
Tzedakis A, Damilakis J, Perisinakis K et al (2005) The effect of z overscanning on patient effective dose from multidetector helical computed tomography examinations. Med Phys 32:1621–1629
Leswick DA, Hunt MM, Webster ST et al (2008) Thyroid shields versus z-axis automatic tube current modulation for dose reduction at neck CT. Radiology 249:572–580
Smith AB, Dillon WP, Lau BC et al (2008) Radiation dose reduction strategy for CT protocols: successful implementation in neuroradiology section. Radiology 247:499–506
Papadakis AE, Perisinakis K, Damilakis J (2007) Angular on-line tube current modulation in multidetector CT examinations of children and adults: the influence of different scanning parameters on dose reduction. Med Phys 34:2864–2874
Papadakis AE, Perisinakis K, Damilakis J (2008) Automatic exposure control in pediatric and adult multidetector CT examinations: a phantom study on dose reduction and image quality. Med Phys 35:4567–4576
Coursey C, Frush DP, Yoshizumi T et al (2008) Pediatric chest MDCT using tube current modulation: effect on radiation dose with breast shielding. AJR 190:W54–W61
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raissaki, M., Perisinakis, K., Damilakis, J. et al. Eye-lens bismuth shielding in paediatric head CT: artefact evaluation and reduction. Pediatr Radiol 40, 1748–1754 (2010). https://doi.org/10.1007/s00247-010-1715-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-010-1715-6