Abstract
Background
Microsusceptibility changes in the brain are well known to correspond with microbleeds or micrometal fragments in adults, but this phenomenon has not been explored well in children.
Objective
To assess imaging and clinical characteristics of children with multiple foci of microsusceptibility changes using susceptibility-weighted imaging (SWI).
Materials and methods
Between 2006 and 2008, 12 children with multiple foci of microsusceptibility on SWI without corresponding abnormal signal on conventional MRI were identified and were retrospectively assessed.
Results
The locations of foci of microsusceptibility included the cerebral white matter, basal ganglia, brainstem and cerebellar white matter, without any clear systematic anatomic distribution. CT (n = 5) showed no calcification at the locations corresponding to the microsusceptibility on SWI. Conventional MR imaging showed white matter volume loss (n = 5), delayed myelination (n = 2), acute infarction (n = 1), chronic infarction (n = 1), meningitis (n = 1), slight signal abnormality in the white matter (n = 1) and no abnormal findings (n = 1). Follow-up SWI (n = 3) showed no change of the microsusceptibility foci. Interestingly, all children had a history of heart surgery under extracorporeal circulation for congenital heart disease.
Conclusion
Multiple foci of microsusceptibility can be seen in the brain on SWI in children with congenital heart disease who underwent heart surgery with extracorporeal circulation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With the advent of modern MR imaging techniques, microsusceptibility changes in the brain have been recognized. Major causes of these microsusceptibility changes were considered to be microbleeds related to microangiopathy, moyamoya disease, anticoagulant therapy, angiitis and diffuse axonal injury [1–11]. Another cause was reported to be microscopic embolic metal fragments from prosthetic heart valves [12, 13]. Several investigators reported that identifying microbleeds was of importance because it could be an increased risk factor for cerebral bleeding or lacunar stroke [2, 14–16]. Causes and clinical significance of microsusceptibility changes have been investigated well in adults. To our knowledge, however, the imaging and clinical characteristics of microsusceptibility changes in children have not been well established.
Recently, susceptibility-weighted imaging (SWI) has been introduced as a highly sensitive method for the visualization of substances with susceptibility effects such as blood, iron, calcification and air. The SWI sequence is a high-spatial-resolution, three-dimensional, fast low-angle shot MR imaging, technique with phase-postprocessing [17–20]. SWI demonstrates substances with susceptibility effects as signal loss. Recent studies reported the detectability of microbleeds on SWI to be higher than that on T2*-weighted imaging advocating the use of the former when searching for microsusceptibility changes [5, 21]. The aim of this study was to assess imaging and clinical characteristics of children with multiple foci of microsusceptibility changes in the brain on SWI that were not visualized on conventional MR imaging.
Materials and methods
Patients
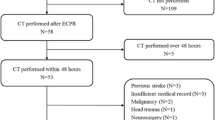
Institutional review board approval and informed consent were waived for this retrospective study. Between June 2006 and May 2008, all children (age ≤18 years) who were suspected of having intracranial haemorrhage or in whom intracranial haemorrhage needed to be ruled out, underwent MR imaging including SWI at our institute. MR images of all these children were assessed by either of two experienced board-certified paediatric neuroradiologists on the same day of scanning. Cases with multiple foci of microsusceptibility changes in the brain on SWI without corresponding abnormal signal on conventional MR imaging were included. Cases were excluded when abnormal signal was also visualized on conventional MR imaging at the location that corresponded with the area of signal loss on SWI, i.e., if a corresponding area with high signal intensity was seen on T1-weighted images (e.g., due to haemorrhage) or low signal intensity on T2-weighted images (e.g., due to haemosiderin, metal or calcification).
This approach was chosen because the present study focused on microsusceptibility changes rather than gross susceptibility changes that are also visible on conventional MR sequences. Twelve cases (8 boys, 4 girls; age range 0–5 years, mean age 12.7 months) in whom foci of microsusceptibility changes were only noted on SWI were included. Their images and clinical data were retrospectively assessed.
MR imaging
All scanning was done using a 1.5-T MR unit (Avanto, Siemens, Erlangen, Germany) with a 33 mT/m maximum gradient capability and a maximum slew rate of 125 mT/m/ms. Scanning was performed with a combination of high-resolution surface coils for neonates and infants and a head coil for older children. Sedating agents were used when necessary. The routine MR imaging protocol included axial T1-W spin-echo, axial, and sagittal or coronal T2-W fast spin-echo and axial diffusion-weighted imaging (DWI). Imaging parameters varied depending on the child’s development and head size [22]. The imaging parameters used were: T1-W spin-echo, TR 485—523 ms, TE 9.3–11 ms, one signal acquired; T2-W fast spin-echo, TR 4,530—5,360 ms, TE 110—140 ms, one signal acquired; DWI, TR 5,000 ms, TE 94 ms, two signals acquired, generalized autocalibrating partially parallel acquisition (GRAPPA) 2, diffusion gradients, b = 0 and 1,000 s/mm2. Other parameters were as follows: field of view, 141–167 × 150–200 mm; matrix size, 119–144 × 192–256; slice thickness, 5 mm with a 1-mm intersection gap.
SWI consisted of a strongly susceptibility-weighted, low-bandwidth (80 Hz/pixel), 3-D, fast low-angle shot sequence with first-order flow compensated in all three orthogonal directions. Since poorer visualization of the venous system had been observed in neonates and infants compared with older children on standard SWI sequence (unpublished data), we used a longer TE for neonates and infants to obtain more susceptibility effect. The parameters for SWI were: TE 69 ms, TR 60 ms for neonates, TE 59 ms, TR 50 ms for infants and TE 49 ms, TE 40 ms for children older than 12 months; flip angle 20°; slice thickness 1.3–2 mm; field of view 150 × 200–250 mm; matrix size 130–150 × 256; GRAPPA 2; acquisition time approximately 4–5 min. SWI was created using the magnitude and phase images. The normalized phase mask was multiplied four times against the original magnitude image [17, 18]. Finally, a minimum-intensity projection was done over contiguous two or three sections to display approximately 4-mm-thick transverse images.
Additional planes and sequences, such as fluid-attenuated inversion-recovery (FLAIR) and contrast-enhanced T1-W images, were obtained depending on the disease.
Data analysis
MR images were retrospectively evaluated by two experienced board-certified paediatric neuroradiologists by using a picture archiving and communication system (Synapse, Fuji Medical Systems, Tokyo, Japan) that was routinely used to view images. The evaluations were done by consensus between two radiologists. Microsusceptibility changes on SWI (i.e. microsignal loss) were defined as small round lesions with signal loss without continuity to surrounding vascular structures. Assessment of SWI was done with all the continuous images on the image viewer and anatomic locations of microsignal loss noted. Areas with microsignal loss but without a distinct discrimination between the signal loss and adjacent veins were excluded. CT images were assessed for the presence or absence of calcification at the location corresponding to the signal loss on SWI, if available. Conventional T1- and T2-W MR images were also reviewed to assess pre- and co-existing brain disease or abnormalities. In children who had serial SWI examinations, SWI and conventional MR images were reviewed to assess any signal change at the location corresponding to signal loss on the initial SWI.
Medical records of all children were systematically reviewed with regard to the presence of neurologic or systemic diseases and clinical history.
Results
The children’s symptoms that prompted MR imaging included fever (n = 1), weakness of the extremities (n = 1), follow-up examination of chronic infarction (n = 1), lack of physical activity after episode of fever (n = 1), developmental delay (n = 1) and baseline study after heart surgery (n = 7). The age distribution was 0–1 years (n = 9), 1 year (n = 1), 2 years (n = 1), and 5 years (n = 1).
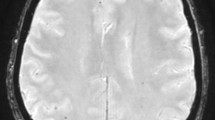
The locations of foci of microsignal loss included the cerebral white matter, basal ganglia, brainstem, and cerebellar white matter (Table 1). No apparent systematic anatomic distribution of microsignal loss on SWI was observed (Fig. 1). In five children, CT was performed between 0 and 52 days before or between 8 and 22 days after the MR examination. CT showed no calcification at the locations corresponding to the areas of signal loss on SWI in all five cases.
Two-year-old boy with hypoplastic left heart syndrome who underwent Fontan and Norwood surgery with extracorporeal circulation. a Axial SWI shows multiple foci of dotted signal loss (arrows). b T2- and c T1-W images show no abnormal signal at the location corresponding to the area of signal loss on SWI
Conventional MR findings included white matter volume loss (n = 5), delayed myelination (n = 2), acute infarction (n = 1), chronic infarction (n = 1), meningitis (n = 1) and slight signal abnormality in the white matter (n = 1) and no abnormal findings (n = 1). In two children with infarction, foci of microsignal loss were found in both normal and infarcted areas (Fig. 2). In one child with meningitis, MR images showed bilateral subdural effusion and SWI showed multiple foci of microsignal loss in the brain parenchyma (Fig. 3). In the child with slight signal abnormality in the white matter, slight hypersignal was observed in the deep white matter of both parietal lobes on T2-W images, whereas foci of signal loss on SWI were found in another location.
Eleven-month-old girl with partial anomalous pulmonary venous connection and atrial defect who underwent repair surgery and closure of the atrial septal defect. MR imaging was performed on the second day of acute cerebral infarction, which occurred 5 days after heart surgery. a Axial SWI shows multiple foci of microsignal loss (arrows). b Axial T2- and c T1-W images show acute infarction in the bilateral middle cerebral arterial territories (arrowheads). Note that foci of signal loss on SWI are found in both the normal and infarcted areas
Eight-month-old boy with meningitis. MR imaging was performed 2 months after Rastelli operation with atrial ventricular septal defect. a Axial SWI shows multiple foci of microsignal loss (arrows). b T2-W and (c) contrast-enhanced T1-W images show bilateral subdural effusion (arrowheads). Images show no abnormal signal at the location corresponding to the area of signal loss on SWI
Three children had follow-up MR examinations (4 weeks, 5 weeks and 9 months after the initial SWI, respectively). Follow-up SWI showed no changes in foci of signal loss. Follow-up conventional MR images showed no new lesions at the locations corresponding to the areas of signal loss on the initial SWI.
Interestingly, all children had a history of heart surgery under extracorporeal circulation for congenital heart disease. They underwent the operation between 6 and 1,630 days before the MR examination. Their congenital heart disease included hypoplastic left heart syndrome (n = 3), total anomalous pulmonary venous connection (n = 2), partial anomalous pulmonary venous connection and atrial septal defect (n = 1), atrial and ventricular septal defect (n = 1), complete transposition of great arteries (n = 1), corrected transposition of great arteries and pulmonary atresia (n = 1), double outlet right ventricle (n = 1), tetralogy of Fallot (n = 1) and pulmonary atresia (n = 1). Two children had been receiving anticoagulant therapy (warfarin) for 1 and 2 years after heart surgery, respectively. Co-existing abnormalities included chromosomal abnormalities [trisomy 21 (n = 1), 22q deletion (n = 1)] and asplenia (n = 1).
Discussion
It is well known that multiple foci of microsusceptibility changes can be observed in adults. Our study demonstrates that similar findings can be seen in children. In children, relatively small foci of bleeding have been reported to occur in cases of trauma, vasculitis and infection [19]. However, in our series the children did not have a history of hypertension, angiitis or trauma. In addition, none of the children had sickle cell disease. Although minor trauma may not be completely ruled out in our series, it should be noted that microbleeds can be seen in the frontal white matter or parieto-temporal-occipital gray or white matter in most children with diffuse axonal injury, while several regions including the thalamus, brainstem, cerebellum and basal ganglia are less affected in this condition [19]. This distribution of microbleeds in diffuse axonal injury is different from that in our series. Furthermore, there was no characteristic pattern with respect to the location of microsusceptibility changes; this suggests that the microsusceptibility changes on SWI in this series were not related to a specific brain circulation or disorder, but rather to a systemic origin. Interestingly, all children in this series had congenital heart disease and had undergone heart surgery with extracorporeal circulation. We are therefore the first to speculate that there may be a relation between microsusceptibility changes on SWI and a history of heart surgery with extracorporeal circulation. Since anticoagulants were used during surgery, we speculate that multiple foci of microsusceptibility changes on SWI in this series may be a result of microbleeds due to increased bleeding tendency.
Several investigators reported that intraparenchymal haemorrhage occured in approximately 30% of neonates and infants who had undergone heart surgery, based on findings at US examination or conventional MR imaging [23–25]. Although detailed imaging findings were not described in these reports, the haemorrhage that was seen in their cases might be different from the microsusceptibility changes seen in our series. Nevertheless, their reports suggest that intraparenchymal haemorrhage may occur in a certain population of neonates and infants after heart surgery and support our speculation that microsusceptibility changes may be due to microbleeds that occurred during or after heart surgery.
In the current study the onset of microsusceptibility changes is unknown. Furthermore, although we did not include cases with abnormal signal on T1-and T2-W sequences, we cannot exclude the possibility of pre-existing disease such as microemboli at the sites of microsusceptibility changes in some cases. In one child, multiple foci of microsusceptibility changes were found on SWI more than 4 years after heart surgery. This child had been receiving anticoagulants for 2 years after heart surgery and might have been under conditions of bleeding tendency for a relatively long period. Currently, there are no data concerning the time for the microsusceptibility changes to appear on SWI after microbleeding. In a child with meningitis in our series, we cannot exclude the cause of microsusceptibility to be microbleeds related to intracranial inflammation.
Another possible explanation for the microsusceptibility changes on SWI may be small migrating metallic agents, such as fragments of suction tube, entering the vascular system during operation. However, susceptibility artefacts of metal are often larger than those of microbleeds and may be seen on conventional MR images [12]. This suggests metal is a less likely cause of the dotted signal loss on SWI. Nevertheless, we cannot completely exclude the possibility that micrometal may be the cause of microsusceptibility changes in this series.
It is very unlikely that the microsusceptibility changes that were seen in this study are due to air or calcium. Generally, air can be identified as hyposignal on conventional T1- and T2-W images, but this was not the case in our series. Furthermore, the presence of air could also be ruled out because follow-up SWI showed no changes in signal loss. CT showed no calcification in the corresponding area, though it should be mentioned that CT was not performed simultaneously with MR imaging.
This study had several limitations. First, it was a retrospective study including a relatively low number of cases. Nevertheless, all consecutive children who underwent MR imaging for the detection or exclusion of intracranial microsusceptibility foci in a period of almost 2 years were reviewed in order to minimise selection bias. Second, since this was a retrospective study, the timing of the imaging scans varied depending on the child’s status. Third, the number of serial SWI scans and the interval follow-up SWI scans in this study were insufficient to provide more insight into the signal changes of microsusceptibility in time. Fourth, imaging parameters varied among children depending on age and size. Therefore, although a relation between multiple foci of microsusceptibility changes and heart surgery with extracorporeal circulation was suggested in our series, a larger prospective study (e.g., a prospective study in which MRI with SWI is performed before and after heart surgery with extracorporeal circulation) or case-control study is needed to confirm our findings and to provide more definitive insight into the causes of microsusceptibility changes in the brains of children on SWI. Furthermore, the clinical significance of these microsusceptibility changes in terms of neurological symptoms or development should be determined in a follow-up study. Fifth, cases were excluded when abnormal signal was also visualized on conventional MR imaging at the location that corresponded to the area of signal loss on SWI. As mentioned previously, this approach was chosen because the present study focused on microsusceptibility changes rather than gross susceptibility changes that are also visible on conventional MR sequences. However, it might be interesting, for example, for future studies to investigate T1 hyperintense lesions (that may be related to either haemorrhage or ischaemia) using SWI. Nevertheless, this was beyond the scope of the present study.
Conclusion
Multiple foci of microsusceptibility changes can be seen in the brain on SWI in children with congenital heart disease who underwent heart surgery with extracorporeal circulation.
References
Roob G, Lechner A, Schmidt R et al (2000) Frequency and location of microbleeds in patients with primary intracerebral hemorrhage. Stroke 31:2665–2669
Kato H, Izumiyama M, Izumiyama K et al (2002) Silent cerebral microbleeds on T2*-weighted MRI: correlation with stroke subtype, stroke recurrence, and leukoaraiosis. Stroke 33:1536–1540
Naka H, Nomura E, Wakabayashi S et al (2004) Frequency of asymptomatic microbleeds on T2*-weighted MR images of patients with recurrent stroke: association with combination of stroke subtypes and leukoaraiosis. AJNR 25:714–719
Fazekas F, Kleinert R, Roob G et al (1999) Histopathologic analysis of foci of signal loss on gradient-echo T2*-weighted MR images in patients with spontaneous intracerebral hemorrhage: evidence of microangiopathy-related microbleeds. AJNR 20:637–642
Mori N, Miki Y, Kikuta K et al (2008) Microbleeds in moyamoya disease: susceptibility-weighted imaging versus T2*-weighted imaging at 3 Tesla. Invest Radiol 43:574–579
Kikuta K, Takagi Y, Nozaki K et al (2007) Histological analysis of microbleed after surgical resection in a patient with moyamoya disease. Neurol Med Chir (Tokyo) 47:564–567
Ishikawa T, Kuroda S, Nakayama N et al (2005) Prevalence of asymptomatic microbleeds in patients with moyamoya disease. Neurol Med Chir (Tokyo) 45:495–500
Kikuta K, Takagi Y, Nozaki K et al (2005) Asymptomatic microbleeds in moyamoya disease: T2*-weighted gradient-echo magnetic resonance imaging study. J Neurosurg 102:470–475
Vernooij MW, Haag MD, van der Lugt A et al (2009) Use of antithrombotic drugs and the presence of cerebral microbleeds: the Rotterdam Scan Study. Arch Neurol 66:714–720
Tong KA, Ashwal S, Holshouser BA et al (2003) Hemorrhagic shearing lesions in children and adolescents with posttraumatic diffuse axonal injury: improved detection and initial results. Radiology 227:332–339
Santhosh K, Kesavadas C, Thomas B et al (2009) Susceptibility weighted imaging: a new tool in magnetic resonance imaging of stroke. Clin Radiol 64:74–83
van Gorp MJ, van der Graaf Y, de Mol BA et al (2004) Bjork-Shiley convexoconcave valves: susceptibility artifacts at brain MR imaging and mechanical valve fractures. Radiology 230:709–714
van Gorp MJ, de Mol BA, Bakker CJ et al (2003) Black holes on MR images of the brain of patients with Bjork-Shiley heart valves: additional observation in three cases. AJNR 24:512–514
Nighoghossian N, Hermier M, Adeleine P et al (2002) Old microbleeds are a potential risk factor for cerebral bleeding after ischemic stroke: a gradient-echo T2*-weighted brain MRI study. Stroke 33:735–742
Wardlaw JM, Lewis SC, Keir SL et al (2006) Cerebral microbleeds are associated with lacunar stroke defined clinically and radiologically, independently of white matter lesions. Stroke 37:2633–2636
Ueno H, Naka H, Ohshita T et al (2008) Association between cerebral microbleeds on T2*-weighted MR images and recurrent hemorrhagic stroke in patients treated with warfarin following ischemic stroke. AJNR 29:1483–1486
Reichenbach JR, Venkatesan R, Schillinger DJ et al (1997) Small vessels in the human brain: MR venography with deoxyhemoglobin as an intrinsic contrast agent. Radiology 204:272–277
Haacke EM, Xu Y, Cheng YC et al (2004) Susceptibility weighted imaging (SWI). Magn Reson Med 52:612–618
Tong KA, Ashwal S, Obenaus A et al (2008) Susceptibility-weighted MR imaging: a review of clinical applications in children. AJNR 29:9–17
Haacke EM, Mittal S, Wu Z et al (2009) Susceptibility-weighted imaging: technical aspects and clinical applications, part 1. AJNR 30:19–30
Akter M, Hirai T, Hiai Y et al (2007) Detection of hemorrhagic hypointense foci in the brain on susceptibility-weighted imaging clinical and phantom studies. Acad Radiol 14:1011–1019
Barkovich AJ, Kjos BO, Jackson DE Jr et al (1988) Normal maturation of the neonatal and infant brain: MR imaging at 1.5 T. Radiology 166:173–180
Tavani F, Zimmerman RA, Clancy RR et al (2003) Incidental intracranial hemorrhage after uncomplicated birth: MRI before and after neonatal heart surgery. Neuroradiology 45:253–258
Krull F, Latta K, Hoyer PF et al (1994) Cerebral ultrasonography before and after cardiac surgery in infants. Pediatr Cardiol 15:159–162
Mahle WT, Tavani F, Zimmerman RA et al (2002) An MRI study of neurological injury before and after congenital heart surgery. Circulation 106:I109–114
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Niwa, T., Aida, N., Takahara, T. et al. Imaging and clinical characteristics of children with multiple foci of microsusceptibility changes in the brain on susceptibility-weighted MRI. Pediatr Radiol 40, 1657–1662 (2010). https://doi.org/10.1007/s00247-010-1665-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-010-1665-z