Abstract
Background
T2-weighted fast spin-echo imaging (T2-W FSE) is frequently degraded by motion in pediatric patients. MR imaging with periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER) employs alternate sampling of k-space to achieve motion reduction.
Objective
To compare T2-W PROPELLER FSE (T2-W PROP) with conventional T2-W FSE for: (1) image quality; (2) presence of artefacts; and (3) ability to detect lesions.
Materials and methods
Ninety-five pediatric patients undergoing brain MRI (1.5 T) were evaluated with T2-W FSE and T2-W PROP. Three independent radiologists rated T2-W FSE and T2-W PROP, assessing image quality, presence of artefacts, and diagnostic confidence. Chi-square analysis and Wilcoxon signed rank test were used to assess the radiologists’ responses.
Results
Compared with T2-W FSE, T2-W PROP demonstrated better image quality and reduced motion artefacts, with the greatest benefit in children younger than 6 months. Although detection rates were comparable for the two sequences, blood products were more conspicuous on T2-W FSE. Diagnostic confidence was higher using T2-W PROP in children younger than 6 months. Average inter-rater agreement was 87%.
Conclusion
T2-W PROP showed reduced motion artefacts and improved diagnostic confidence in children younger than 6 months. Thus, use of T2-W PROP rather than T2-W FSE should be considered in routine imaging of this age group, with caution required in identifying blood products.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
T2-weighted (T2-W) sequences are a standard part of brain MRI protocols and are critical for detection and characterization of pathology as well as delineation of normal structures. The fast spin-echo (FSE) technique is a commonly used method for reducing scan time relative to conventional spin-echo (CSE) without sacrificing diagnostic information [1, 2]. However, T2-W FSE sequences still require a scan time in the range of 2 to 3 min, which is long enough to incur substantial artefacts in pediatric patients, who are prone to motion. Sedation and anesthesia, which are not without risk, are often used in MR imaging of infants and young children to reduce motion and to generate images of diagnostic quality [3]. However, if additional means for reducing motion artefact can be employed, sedation and anesthesia might not be necessary. Traditionally, radiologists have focused on decreasing motion artefact by reducing the scan time, which can be accomplished by shortening the echo time, increasing the sampling rate and reducing echo train length. However, such techniques (e.g., single-shot FSE, SSFSE) often suffer blurring and other artefacts that reduce image quality and decrease lesion detection [4–7].
MR imaging with periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER or PROP), which was introduced by Pipe [8] in 1999, uses a different strategy, reducing in-plane rotation and translational head motion by alternate sampling of k-space. PROP acquires multiple echo trains in a rotating, partially overlapped fashion with concentric blades that rotate through the center of k-space. Sampling the center of k-space many times in this fashion can itself improve artefact suppression. In addition, motion correction can be performed, as data within the central region can be compared between blades, and data can be transposed to an estimated stationary position before final reconstruction if motion has occurred. Forbes et al. [9] in 2003 showed that T2-W PROP achieves similar motion reduction to SSFSE in pediatric brain imaging for evaluation of ventriculomegaly, and noted that T2-W PROP provides improved parenchymal detail. As mentioned above, SSFSE is, however, prone to blurring, and thus an inferior image quality, in a similar manner to conventional T2-W FSE. In addition, the aforementioned study did not evaluate the performance of T2-W PROP in diagnosis of brain pathologies that were more subtle than ventriculomegaly.
A more recent study evaluated the use of PROP in T2-W fluid-attenuated inversion recovery (FLAIR) imaging at 3 T in a series of adults, but only evaluated its influence on ghosting, pulsation, and Gibbs artefacts and general image quality, without looking at lesion detectability. The study showed a general reduction in artefacts and equal or better image quality in the majority of cases in comparison to standard T2-W FLAIR [10]. The most current investigation of PROP evaluated its usefulness at 1.5 T with contrast-enhanced T1-W imaging of the brain in children, and showed a reduction in motion and pulsation with no loss of diagnostic information [11]. But the diagnostic reliability of T2-W PROP has not been compared with that of conventional T2-W FSE imaging, arguably one of the most essential sequences in brain imaging, in a large pediatric population.
We compared the image quality of T2-W PROP with that of conventional T2-W FSE in a population of children in a clinical setting, assessing general image quality, motion and other artefacts as well as its influence on radiologists’ ability to detect lesions, diagnostic confidence and time required to review images. Our hypothesis was that T2-W PROP would provide superior diagnostic information and anatomic detail, improving diagnostic confidence without increasing time to review the images, and that it could routinely replace conventional T2-W FSE in pediatric examinations, especially in young infants (<6 months of age) not undergoing anesthesia, and that T2-W PROP might be preferred over conventional T2-W FSE because of decreased motion artefacts.
Materials and methods
The procedures followed Stanford institutional guidelines and the study was approved by the Institution Review Board, and was in accordance with the ethical standards of the Declaration of Helsinki.
Patients
A total of 95 consecutive patients who were undergoing brain MRI at our institution were prospectively enrolled in this study and evaluated. These patients ranged in age from 0 days to 23 years (Fig. 1). One-third of the patients underwent general anesthesia during imaging. Patients were imaged for a variety of clinical indications, including prematurity, pre- and postoperative tumor evaluation, developmental delay, congenital anomalies, seizures, epilepsy, neurofibromatosis, headache, infection, stroke, vascular malformations, ventriculomegaly, and macrocephaly (Table 1).
Imaging parameters
MRI studies were performed at 1.5 T (Signa, GE Healthcare, Milwaukee, WI) and, depending on patient size and age, either an eight-channel head-spine array or a four-channel head coil (both MR Devices) was used for signal reception. Images were obtained in the axial plane with scan parameters that varied slightly between infants and children because of differing sizes. For infants, T2-W FSE images were acquired with TR 4 s, TE 110.4 ms, number of excitations (NEX) 2, slice thickness 4 mm with no gap, echo train length (ETL) 8, receiver bandwidth (RBW) 41 kHz, matrix 288×192 reconstructed at 512×512, and field of view (FOV) 200 mm. T2-W PROP images were acquired with TR 4.1 s, TE 112 ms, NEX 1.5, slice thickness 4 mm with no gap, ETL 24, RBW 195 kHz, matrix 480×480 reconstructed at 512×512, and FOV 200 mm. For children, T2-W FSE images were acquired with TR 5.6 s, TE 104 ms, NEX 1, slice thickness 5 mm with a 1.5-mm gap, ETL 17, RBW 162 kHz, matrix 256×192 reconstructed at 256×256, and FOV 220 mm. T2-W PROP images were acquired with TR 7.5 s, TE 92 ms, NEX 1.5, slice thickness 5 mm with a 1.5-mm gap, RBW 390 kHz, ETL 24, matrix 256×256 reconstructed at 256×256, and FOV 220 mm. T2-W FSE scans were obtained first, followed by T2-W PROP, in addition to other sequences determined by the patients’ clinical presentations. T2-W FSE and T2-W PROP sequence scan times were comparable, and ranged between 2 and 3 min.
Image assessment
Three independent radiologists (E.R., M.V.K. and A.T.V.) with 2–6 years experience in pediatric neuroradiology evaluated the MR imaging studies for all patients on a PACS workstation (Centricity, GE Healthcare). Final diagnosis was made by a senior pediatric neuroradiologist (P.D.B.) using all clinical and imaging material (including previous examinations if available), which served as the ground truth for the study. T2-W PROP and T2-W FSE images were viewed separately on different occasions and then later evaluated in a side-by-side comparison. The radiologists rated the images on a scale from 1 (barely acceptable or very unsure of diagnosis) to 10 (outstanding quality, no artefacts, or absolutely sure of diagnosis) for perceived overall quality, severity of artefacts (including motion and blurring), and diagnostic confidence, noting the number of lesions detected and commenting on the types of lesions detected (e.g., hypointense blood product vs. T2 hyperintense lesions).
Images of outstanding quality (score 10) had virtually no motion artefact (including pulsation), sharp depiction of anatomy, including gray and white matter structures and, in abnormal cases, clear definition of intracranial lesions. Images with scores in the range 7–9 were still of good quality with minimal motion and depicted lesions well, but demonstrated either pulsation or mild blurring. Images with scores in the range 4–6 were somewhat degraded by artefacts, including motion, but were still interpretable, and those with scores below 4 were not easily interpretable. Diagnostic confidence was considered 100% for scores of 10 and was proportionally lower for each rating below 10. Each radiologist commented on the perceived time to read images from each of the sequences (as compared with a typical non-motion degraded T2-W FSE image), and, when comparing the two sequences, noted whether they thought T2-W PROP would change the clinical treatment for the patient.
Statistics
Pearson’s chi-squared and Wilcoxon’s signed ranks tests were used to assess the radiologists’ ratings. The Fisher exact test was used to compare the results between patients with normal findings and those with abnormalities seen on MR imaging. Population-averaged generalized estimating equation (PA-GEE) regressions of image quality score and motion artefacts on method (T2-W FSE or T2-W PROP), anesthesia (present or absent), and age (<6 months or ≥6 months) were performed, with subject-clustering as the variable. An exact Kolmogorov-Smirnov test was used to compare ages of patients having MR imaging with and without anesthesia. Interobserver variability was rated using Kendall’s coefficient of concordance. All statistical analyses were done with Stata Release 9.2 (Stata, College Station, TX).
Results
The mean age of the patients was 5 years 4 months and ages ranged from 0 days to 23 years (Fig. 1). The 31 patients who underwent general anesthesia during imaging had a mean age of 3 years 11 months and ranged in age from 6 days to 14 years. The age distribution of the group undergoing anesthesia differed significantly from that of those not undergoing anesthesia (P < 0.001, Fig. 2). Prematurity (16%) was the most common indication for MR imaging, followed by posttreatment tumor evaluation (15%), developmental delay (10%), congenital anomalies (7%) and seizures (6%). Other less frequent indications included primary evaluation of neoplasms, neurofibromatosis, headache, infection, stroke, vascular malformations, ventriculomegaly, and macrocephaly. Of the 95 patients, 19 (20%) had normal findings on MRI. Those children with abnormalities on MRI demonstrated a combination of large imaging lesions (e.g., structural anomalies, ventricular dysmorphism or enlargement, strokes, resection cavities, catheter tracts, and diffuse white matter abnormalities) and focal lesions (e.g., neurofibromatosis 1 spots, foci of hemorrhage seen especially in premature infants, tumor deposits, and other nonspecific focal T2 lesions).
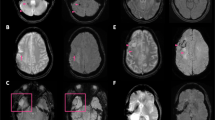
Compared with T2-W FSE images, T2-W PROP images demonstrated significantly better quality (P < 0.009) and reduced motion artefacts (P < 0.0001), with greater high-quality and fewer low-quality ratings in each category (Fig. 3). There was no tendency to higher detection rates with one sequence over the other (in 98% of 11,479 ratings T2-W PROP images showed identical lesion detection to T2-W FSE images). Although overall anatomic detail and T2 lesion visibility were similar between the sequences (Fig. 4), blood products showing increased susceptibility were observed to be more conspicuous on the T2-W FSE images than on the T2-W PROP images in all 12 cases where they occurred (Fig. 5).
T2-W FSE vs. T2-W PROP. Scoring distribution across raters for (a) diagnostic confidence, (b) motion artefacts, and (c) overall image quality. Despite the improved image quality and reduced motion artefacts, diagnostic confidence was rated only marginally better if all patients (including older patients without motion) were evaluated (see text)
Conventional T2-W FSE image (a) shows a similar degree of motion and similar image quality to the T2-W PROP image (b) in a 4-year-old girl with a diagnosis of neurofibromatosis 1. Anatomic detail, including gray–white differentiation, and demonstration of posterior fossa NF-1 spots (arrows) are not significantly different between the images
Conventional T2-W FSE images (a, b) show significantly greater motion artefact than T2-W PROP images (c, d) in a premature infant imaged at full-term-corrected gestational age. Although anatomic detail, including gray–white differentiation, is better delineated with T2-W PROP, susceptibility from focal hemorrhage is less well seen (arrows)
Multivariate regression analysis indicated that older patients had higher image quality than younger patients (P < 0.001). The use of general anesthesia produced nominally better image quality and motion artefact scores overall, but these differences were not statistically significant (P < 0.144 and P < 0.115, respectively). This result is surprising but is likely related to the inherent bias of selecting patients prone to greatest motion for general anesthesia in the first place; infants younger than 6 months were less likely to undergo anesthesia (6% vs. 47%, P = 0.0001), as is typical in clinical practice (because of the bundle-and-feed method available for settling these infants during imaging) and showed greater motion artefacts than patients older than 6 months (P < 0.001). The distribution of motion rating scores among patients younger than 6 months, between 6 and 48 months, and older than 48 months, with and without anesthesia, is shown in Fig. 6 and highlights the greater benefit of T2-W PROP in young children not undergoing anesthesia.
Distribution of scores of motion artefacts (ranging from 10 no motion to 0 marked motion) for patients younger than 6 months, between 6 months and 48 months, and older than 48 months, with and without anesthesia. The benefit of T2-W PROP is more evident in the patients not undergoing anesthesia, but slightly higher ratings are still seen with T2-W PROP in those undergoing anesthesia
T2-W PROP showed improvements over T2-W FSE in both image quality (P < 0.001) and motion artefacts (P < 0.001); this was especially evident in infants younger than 6 months (Fig. 7).
T2-W FSE vs. T2-W PROP. Effects of anesthesia and patient age. a T2-W PROP images showed reduced motion artefacts relative to T2-W FSE images regardless of patient age or use of anesthesia. Greatest motion artefact reduction was obtained with T2-W PROP in infants <6 months age not undergoing general anesthesia. b Raters scored overall quality of T2-W PROP images as better than T2-W FSE images in infants younger than 6 months of age, but scores were similar in children older than 6 months
Diagnostic confidence was only marginally better for T2-W PROP than for conventional T2-W FSE (P < 0.017) in the patient population as a whole (Fig. 3). However, diagnostic confidence was significantly higher for T2-W PROP than for T2-W FSE in infants younger than 6 months (P < 0.001, Fig. 8). The use of T2-W PROP was considered unlikely to have altered management in any of the children imaged (only 1 of 287 responses) and was generally not considered to have affected image read-out time (69% of 287 responses were “no effect”). Nevertheless, among those who indicated an effect, 68% of responses were that T2-W PROP reduced read-out time (P < 0.001, two-sided exact binomial test).
No significant difference was found in results obtained in patients with normal MR imaging studies as compared to those with abnormal findings (P < 0.061).
On average, inter-rater agreement was 87% and never fell below 75% for any of the subtests administered. For image quality ratings, Kendall’s coefficient of concordance was 0.47 (0.38–0.57) for T2-W PROP and 0.60 (0.49–0.71) for T2-W FSE. For motion artefact ratings, the coefficients of concordance were similar at 0.49 (0.37–0.60) for T2-W PROP and 0.62 (0.51–0.73) for T2-W FSE. The highest agreement in ratings was seen between readers 2 and 3 (E.R. and A.T.V.), and the lowest agreement between readers 1 and 3 (M.V.K. and A.T.V.). Readers 2 and 3 tended to give higher ratings for image quality for T2-W PROP than reader 1, whereas the opposite was observed for image-quality ratings for T2-W FSE (Fig. 9).
Agreement in ratings of image quality among readers for (a) T2-W PROP and (b) T2-W FSE. Quality ratings for reader 1 are represented on the x-axis, whereas readers 2 (o) and 3 (+) are shown on the y-axis. Reader 1 tended to give higher ratings for T2-W FSE image quality and lower ratings for T2-W PROP compared to ratings given by readers 2 and 3
Discussion
In children, motion is particularly common during MR imaging and often leads to the use of general anesthesia, with its inherent risks, to acquire images of diagnostic quality. If motion artefacts can be reduced, then the use of anesthesia for pediatric MR imaging might be decreased. Furthermore, a certain amount of motion is present even in patients with adequate anesthesia (e.g., from ventilation and blood flow), and even children undergoing general anesthesia for MR imaging may benefit from motion artefact reduction strategies although to a lesser degree than those not receiving anesthesia.
Traditional approaches to reducing motion in MR imaging have involved decreasing image acquisition time with consequent decrease in image quality, loss of signal to noise, reduced anatomic detail and decreased lesion detection [4–7]. Consequently, such techniques (e.g., SSFSE) are used only in cases where patient motion is severe and these techniques can be expected to provide only limited diagnostic information. T2-W PROP reduces motion using alternate methods of k-space data collection, providing motion reduction similar to or even better than SSFSE (since motion during the quite lengthy FSE readout cannot be corrected) but improved signal-to-noise, giving this technique the potential to serve as a standard method of T2-W imaging [8, 9].
We performed a comparative evaluation of T2-W FSE and T2-W PROP in terms of image quality and diagnostic yield in a consecutive series of patients ranging in age from 0 days to 23 years. Compared with T2-W FSE, T2-W PROP resulted in images of significantly better quality and with reduced motion artefacts. Lesion detection rates were not significantly different between the two sequences. We conclude from these findings that T2-W PROP offered sufficient diagnostic information that it may be substituted for conventional T2-W FSE in pediatric studies. In our study population, diagnostic confidence was only marginally better with the use of T2-W PROP overall, but was significantly better with the use of T2-W PROP in patients under 6 months of age (who were less likely to undergo general anesthesia). Of note, patients less than 6 months of age also showed a greater degree of motion overall when compared with older patients. We conclude from this finding that not all pediatric patients may benefit from routine substitution of T2-W PROP for T2-W FSE, and we identified a potential patient population (those under 6 months age) who likely would benefit from routine use of T2-W PROP instead of T2-W FSE. We also conclude that T2-W PROP was not of great benefit in patients requiring anesthesia to tolerate MR imaging. Other patients in whom T2-W PROP may be helpful are those who might be expected to have motion for specific reasons related to their clinical presentation. For example, at our institution we now routinely use T2-W PROP in patients with deep brain stimulators who require the stimulator to be turned off to undergo MR imaging and often have uncontrollable spasms during imaging.
One of the readers (M.V.K.) expressed a preference for T2-W FSE over T2-W PROP in cases where motion was average or better. In addition, a different reader (A.T.V.) noted that T2-W PROP images were sometimes less sharp than T2-W FSE images, even in cases where motion artefacts were minimal. It is conceivable that in the absence of motion, radiologists would have an overall preference and greater comfort level for interpreting T2-W FSE compared with T2-W PROP images given greater experience interpreting T2-W FSE images. Alternatively, the quality of T2-W PROP images in the absence of motion might be slightly lower than the quality of T2-W FSE images given greater emphasis on collection of data at the center of k-space, and thus considerably less emphasis on high spatial frequency data. This reduction in high-frequency data can be particularly evident at the margins of the brain parenchyma and can cause blurring of the cortex. However, the extra high spatial frequency data are of low intensity, and this extra contour information is of no benefit if there is even the subtlest motion, as detail is easily lost without motion correction. It might, therefore, be prudent to retain the T2-W FSE sequence in imaging protocols for older or particularly cooperative patients who are able to remain still.
Some pediatric neuroradiologists prefer CSE imaging over FSE for assessment of myelination. Because of differences in magnetization transfer, CSE imaging shows greater contrast to noise in the unmyelinated brain than FSE, and white matter can appear slightly more myelinated on T2-W FSE images relative to CSE images [12]. However, no significant difference in diagnostic information (including myelination) has been shown between FSE and CSE for pediatric brain imaging, and FSE acquisition time is 67–75% shorter [2, 13]. At our institution we have replaced CSE with FSE imaging for all pediatric studies given this practical consideration. In this study, we did not specifically compare T2-W PROP and T2-W FSE for determination of myelination, but included this as part of our diagnostic analysis where relevant. To our knowledge, no one has evaluated T2-W PROP with respect to determination of myelination, and this is an area of future interest.
Although almost the same readout-bandwidths were used for both sequences, all readers observed that blood products were slightly less conspicuous on T2-W PROP images than on T2-W FSE images. Although T2*GRE sequences are primarily used for identification of blood products, this sequence is not always included in all imaging protocols. Thus, radiologists sometimes depend on the T2-W FSE sequence to show signs of prior hemorrhage or mineralization. One potential explanation for this reduced sensitivity might be that PROP data are acquired radially, and thus any off-resonance distortions are “smeared out” across all angles as compared to regular Cartesian acquisitions. In a similar fashion, signal from lipids can be expected to be smeared in all radial directions and water–fat shift artefacts might not be as evident on T2-W PROP images as on T2-W FSE images. Radiologists should be aware of this potential in diagnosis of potentially fat-containing lesions, such as dermoids and teratomas. Further studies are warranted to investigate the degree and nature of this difference in sensitivity for blood products.
Our study had several limitations. Direct comparison of the sequences was limited by variability in patient motion during MR imaging studies. We assumed a similar degree of patient motion between the two consecutive sequences, which might not always have been the case. Furthermore, approximately one-third of the patients were imaged under general anesthesia. Because we did not scan the same patients twice with and without anesthesia, we cannot state whether T2-W PROP would indeed have reduced the need for anesthesia in these patients. The use of anesthesia in this number of patients also likely reduced our sensitivity for detecting the advantage of T2-W PROP, as motion was slightly reduced (although not achieving statistical significance). For this reason, we evaluated the results in the subgroup of infants younger than 6 months, as these young patients were unlikely to undergo anesthesia and yet were prone to motion due to their age.
As our sample represented our typical patient population, there were relatively few patients with small (less than 5 mm) lesions, limiting our ability to exactly measure differences in detection of these lesions. However, a large range of pediatric patient ages and diagnoses were included, and the cases were a realistic representation of a specialized pediatric neuroimaging practice. The evaluation of image quality and motion artefacts was subjective, with some variability in responses demonstrated by the different readers, and with a preference shown by one of the readers relative to the other two for T2-W FSE. This reflects clinical practice, where radiologists often have different preferences for particular imaging strategies and ultimately imaging protocols are influenced by individual preferences. Finally, the inherent limitation of T2-W PROP should be recognized. Although it considerably reduces motion artefact, like all retrospective forms of motion correction it is not immune to through-plane motion, which can be a more significant problem in young infants. Therefore, even if T2-W PROP is used there can still be residual motion artefacts from such motion and prospective techniques for adapting the orientation of the image plane to motion during image acquisition remain an area for investigation.
Conclusion
Our study compared the performance of the T2-W PROP sequence and the T2-W FSE sequence in a practical clinical setting in a large number of pediatric patients referred for brain imaging for a wide variety of indications, the diagnosis of which generally requires a superior ability to delineate anatomic and pathologic detail than that offered by SSFSE. We showed that T2-W PROP can be expected to provide sufficient diagnostic information to replace standard T2-W FSE in children undergoing MR imaging of the brain. Patients younger than 6 months are most likely to benefit from the motion reduction and consequent improved image quality offered by T2-W PROP, whereas standard T2-W FSE is preferred in older children, who are less prone to motion (unless there is a specific a priori expectation of motion, e.g., deep brain stimulators). Caution is required in using T2-W PROP to identify blood products or chemical shift artefact as well as myelination, and further studies of this difference in detection are required.
References
Thorpe JW, Halpin SF, MacManus DG et al (1994) A comparison between fast and conventional spin-echo in the detection of multiple sclerosis lesions. Neuroradiology 36:388–392
Engelbrecht V, Malms J, Kahn T et al (1996) Fast spin-echo MR imaging of the pediatric brain. Pediatr Radiol 26:259–264
American Academy of Pediatrics (1992) Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures. Pediatrics 89:1110–1115
Sugahara T, Korogi Y, Hirai T et al (1997) Comparison of HASTE and segmented-HASTE sequences with a T2-weighted fast spin-echo sequence in screening evaluation of the brain. AJR 169:1401–1410
Mittal TK, Halpin SF, Bourne MW et al (1999) A prospective comparison of brain contrast characteristics and lesion detection using single-shot fast spin-echo and fast spin-echo. Neuroradiology 41:480–486
Ba-Ssalamaha A, Schick S, Heimberger K et al (2000) Ultrafast magnetic resonance imaging of the brain. Magn Reson Imaging 18:237–243
Ge Y, Korogi Y, Sugahara T et al (2001) Comparison between EPI and HASTE for ultra-fast MR imaging of the human brain. Neuroradiology 43:1046–1055
Pipe JG (1999) Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med 42:963–969
Forbes KP, Pipe JG, Karis JP et al (2003) Brain imaging in the unsedated pediatric patient: comparison of periodically rotated overlapping parallel lines with enhanced reconstruction and single-shot fast spin-echo sequences. AJNR 24:794–798
Wintersperger BJ, Runge VM, Biswas J et al (2006) Brain magnetic resonance imaging at 3 Tesla using BLADE compared with standard rectilinear data sampling. Invest Radiol 41:586–592
Alibek S, Adamietz B, Cavallaro A et al (2008) Contrast-enhanced T1-weighted fluid-attenuated inversion-recovery BLADE magnetic resonance imaging of the brain: an alternative to spin-echo technique for detection of brain lesions in the unsedated pediatric patient? Acad Radiol 15:986–995
Shaw DW, Weinberger E, Astley SJ et al (1997) Quantitative comparison of conventional spin echo and fast spin echo during brain myelination. J Comput Assist Tomogr 21:867–871
Ahn SS, Mantello MT, Jones KM et al (1992) Rapid MR imaging of the pediatric brain using fast spin-echo technique. AJNR 13:1169–1177
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vertinsky, A.T., Rubesova, E., Krasnokutsky, M.V. et al. Performance of PROPELLER relative to standard FSE T2-weighted imaging in pediatric brain MRI. Pediatr Radiol 39, 1038–1047 (2009). https://doi.org/10.1007/s00247-009-1292-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-009-1292-8