Abstract
Background
Examinations using ionizing radiation are frequently used in the evaluation of disease activity in children affected by idiopathic inflammatory bowel disease (IBD).
Objective
To develop an MR imaging protocol without the need for fluoroscopic insertion of an enteral tube and to assess the disease activity in children with IBD.
Materials and methods
Included in the study were 37 children (22 girls and 15 boys; age range 7–15 years, mean 11.67 years) with IBD who underwent MR imaging of the small bowel. Of these 37 children, 32 had Crohn disease and 5 had indeterminate colitis. A water solution containing herbal fibres was administered orally or through a nasogastric tube. Patients were imaged on a 1.5-T MR scanner with T1-weighted and Τ2-weighted sequences followed by a dynamic study using 3-D T1-W images after intravenous administration of gadolinium.
Results
The percentage enhancement of the bowel wall was significantly increased in patients with abnormal C-reactive protein (CRP) values compared to patients with CRP values in the normal range (P<0.001). A relatively weak but significant correlation between percentage enhancement of the bowel wall and CRP values was noted during all phases of enhancement.
Conclusion
This MR imaging protocol is a safe and well-tolerated method for evaluating disease activity and extraintestinal manifestations of IBD in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The most common inflammatory bowel disease (IBD) in children is Crohn disease (CD), which is a chronic inflammatory process involving periods of exacerbation and remission, predominantly affecting the small bowel. Follow-through barium examination or conventional enteroclysis are considered the gold standards for radiological examination of the small bowel in patients with suspected or known CD, as they carry a high negative predictive value and allow identification of even subtle mucosal abnormalities.
However, the above methods suffer from two major disadvantages: (1) limited information regarding the extramural mesenteric extension of the disease, and (2) exposure of the patient to radiation, mostly at a young age [1]. MRI has changed the way we assess the small bowel because of the functional information and soft-tissue contrast it can provide, the direct multiplanar imaging capabilities, and the lack of ionizing radiation [2], and, as a result, MR enteroclysis is considered an optimal first-line technique for small-bowel visualization [3]. Moreover, the bowel wall enhancement provided by gadolinium-based agents allows assessment of inflammatory disease activity [4], a factor of great importance as it could alter disease management.
Currently, there is no approved standard protocol for the evaluation of disease activity and in daily clinical practice a multidisciplinary approach including clinical scoring (CD activity index), biological indices (white blood cell count, erythrocyte sedimentation rate [ESR], CRP), and endoscopic and radiological examination is used alone or in combination to monitor disease activity [5]. The purpose of our study was to develop an MR imaging protocol for the assessment and follow-up of small-bowel abnormalities in children suffering from CD, without the need for fluoroscopy and bowel intubation, and to analyse its efficacy in the evaluation of disease activity in correlation with well-established biological markers and activity indices.
Materials and methods
Study population
Included in the study were 37 children (22 girls and 15 boys; age range 7–15 years, mean age 11.67 years). The patients were referred to our department for MR imaging of the small bowel for indeterminate colitis (5 children) or known CD (32 children) proven by histology. At the time of the study, all patients had a clinical exacerbation, with symptoms ranging widely from mild nonspecific abdominal discomfort and dyspepsia to frequent bloody diarrhoea and weight loss.
Laboratory assessment, including measurement of CRP and ESR, was performed during the month prior to the MRI examinations. Within this same time-scale patients were clinically scored for disease activity using the paediatric CD activity index (PCDAI).
All parents gave their informed consent prior to their child’s inclusion in the study. The study protocol was approved by the ethics committee of our hospital.
MR imaging
The cleansing preparation of the small bowel consisted of a low-residue diet from 3 days prior to the examination (ample fluids, no milk products) and nil-by-mouth on the day of the examination. In children who were acutely ill, or could not cooperate, a nasogastric tube was placed and a total amount of 2.5 l of water solution containing 0.1 g per kg body weight of herbal fibres (psyllium) was infused manually over the 4 h prior to MR examination in order to opacify and distend the bowel lumen. In the majority of patients, oral administration of an identical volume of the above solution over a period of 4 h was generally well tolerated. This contrast medium has the property of retaining large amounts of water, up to 20 to 30 times its own volume, thus providing adequate distension. It also exhibits biphasic properties, demonstrating low signal intensity (SI) on T1-W MR images and high SI on T2-W images.
Subsequently, the patients were transferred to the MRI suite and were placed in the prone position. This position is recommended as exerting mild pressure to the anterior abdominal wall and facilitating separation of small-bowel loops, while decreasing the scanning volume and thus the number of coronal sections to be acquired. All examinations were performed on a 1.5-T MR scanner (Intera, release 11: Philips, Best, The Netherlands) with a phased-array coil. Hyoscine bromide (0.1 mmol per kg body weight; Buscopan, Boehringer Ingelheim, Germany) was administered intravenously to decrease peristalsis in the small bowel and prolong distension of the small bowel.
The following pulse sequences were used: single-shot turbo spin-echo (HASTE) with fat saturation (TR 860 ms; TE 80 ms; slice thickness 5 mm; flip angle 90°) in both coronal and axial planes; coronal thin-slice fat-suppressed 3-D T2-bFFE (TR 4.4 ms; TE 1.4 ms; slice thickness 1.5 mm; flip angle 20°); coronal fat-suppressed 3-D T2-bTFE (TR 4.3 ms; TE 1.2 ms; slice thickness 3/1.5 mm; flip angle 20°); and coronal and axial T2-bFFE (TR 4.7 ms; TE 2.3 ms; slice thickness 3 mm; flip angle 60°). A dynamic study was performed after intravenous administration of gadolinium (0.1 mmol per kg body weight) followed by 20 ml of a 0.9% saline solution, with coronal thin-slice 3-D TFE T1-W fat-suppressed sequences in arterial (AP), portal venous (PP) and interstitial (EP) phases (TR 4.8 ms; TE 1.4 ms; slice thickness 3/1.5 mm; flip angle 20°). In all sequences the field-of-view ranged from 300 mm to 400 mm depending on the body habitus of the child. Evaluation late after contrast medium administration was performed with coronal (slice thickness 3 mm) and axial (4 mm) 3-D TFE (THRIVE) sequences (TR 3.6 ms; TE 1.8 ms; flip angle 10º) to examine the whole abdomen.
The total examination time for MR imaging ranged from 20 to 25 min.
Image analysis
All the images were reviewed by one experienced radiologist who was unaware of the results of the clinical assessment and other laboratory tests, including the endoscopic findings. Images were quantitatively and qualitatively analysed for the identification of luminal narrowing, and transmural and extraintestinal manifestations of CD. Quantitative evaluation was performed on a dedicated off-line workstation to minimize errors in measurement. Quantitative evaluation included bowel wall thickening (if there was a parietal diameter of >3 mm) and increased uptake in the bowel wall after intravenous injection of contrast medium. Pathological bowel wall enhancement was defined as increased intensity on gadolinium-enhanced T1-W images compared with the surrounding equivalent structures at visual inspection. Mural uptake of contrast medium in affected areas was compared with the contrast medium uptake in the bowel wall of normal-appearing adjacent bowel loops with optimal distension. The quantitative analysis was conducted by placing regions of interest on the affected and normal-appearing bowel wall and measuring SI. SI measurements were recorded for each patient on MR images obtained before and after contrast medium administration for all phases (arterial, portal venous and equilibrium) of the dynamic study.
For quantitative evaluation of contrast enhancement of the bowel wall, the percentage contrast enhancement was defined as: %CE = [(SI bowel postcontrast − SI bowel precontrast)/SI bowel precontrast] × 100.
Patients were divided into two groups on the basis of CRP values. In group A, CRP was ≥10 mg/l, indicating active disease, and in group B CRP was <10 mg/l, indicating inactive disease.
Qualitative evaluation included identification of bowel-wall oedema, ulcerations, fibrofatty proliferation, lymphadenopathy, bowel stenosis, intraperitoneal free fluid, fistula and abscess. Fibrofatty proliferation was readily recognized on T2-W images as abundant bright mesenteric fat containing low-SI linear structures, corresponding to small mesenteric vessels. Lymphadenopathy was defined as lymph nodes with a short-axis diameter of >5 mm in the mesentery, or >1 cm in the retroperitoneum. Bowel stenosis was present if there was constant luminal narrowing, preceded by prestenotic dilatation.
PCDAI values were available in 32 patients. In 21 patients, the PCDAI was ≥11 and the disease was considered active, while in the remaining 11 patients, the PCDAI was <11 and the disease was considered inactive. CRP and ESR were available in all patients and were considered abnormal if they were more than 10 mg/l and 15 mm/h, respectively.
Statistical analysis
Student’s t-test was used to assess the statistical significance of the differences between mean %CE values of patients with abnormal CRP values and patients with CRP values in the normal range. Correlations between %CE and CRP, PCDAI and ESR values were tested using Spearman’s nonparametric test. P values <0.05 were considered significant in all tests.
Results
None of the patients required sedation. The intraluminal contrast medium distribution was evaluated as homogeneous and optimal distension of the bowel loops was observed in all patients and all sequences.
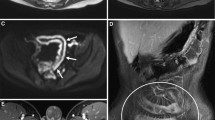
MRI demonstrated nonconstricted bowel lumen in 33 patients, and stenosis with prestenotic dilatation in 3 patients in the terminal ileum (Fig. 1) and in 1 patient in the mid-transverse colon (Fig. 2). Enlarged mesenteric lymph nodes were found in 13 patients and creeping fat was noted in 14 patients. Free intraperitoneal fluid was observed in four patients, while no abscesses or fistulae were visible. In five patients a patent ileocaecal valve was evident, with imaging findings consistent with back-wash ileitis in one (Fig. 3). Wall thickness ranged from 2.5 mm to 12 mm (mean 5.95 mm), while the length of diseased segments ranged from 2 cm to 80 cm (mean 21.2 cm). In all patients with increased enhancement of thickened bowel wall, oedema was also present on T2-W sequences as linear areas of intramural high SI. Deep ulcers were seen in the large bowel in one patient with ulcerative colitis, while superficial ulcers were not prospectively identified.
A 14-year-old girl with CD. a Coronal T2-W image shows loss of haustral folds in the mid transverse colon, oedema and wall thickening, as well as moderate lumen stenosis. b Coronal T1-W image obtained after gadolinium administration during the equilibrium phase, shows mild enhancement of the bowel wall, consistent with chronic changes of the inflammatory disease
PCDAI values ranged from 2.5 to 42.5 (mean 17.81). Percentage contrast enhancement did not correlate with PCDAI in any phase during the dynamic study.
Overall, CRP values ranged from 0.2 to 108 mg/l with a mean of 14.8 mg/l. The percentage contrast enhancement values in enhancing segments were significantly greater in patients with abnormal CRP values than in patients with CRP values in the normal range on arterial-phase images (302±134% vs. 180±124%, P=0.0038), portal-phase images (372±149% vs. 227±113%, P<0.001), and equilibrium-phase images (363±160% vs. 211±106%, P<0.001). Relatively weak but significant correlations between %CE and CRP values were noted during the arterial phase (r=0.51, P=0.0011), portal phase (r=0.50, P=0.0015) and equilibrium phase (r=0.48, P=0.0026). ESR values ranged from 12 mm/h to 112 mm/h (mean 52.8 mm/h). Percentage contrast enhancement did not correlate with ESR values during any phase of enhancement. Analytical data are presented in Table 1.
Discussion
CD is a chronic inflammatory disease of the bowel that has a relapsing and remitting course. Disease activity assessment is important in the evaluation of relapse and response to therapy. Clinical evaluation of CD activity is routinely performed as a measure of response to drug therapy [6]. This often young population with a chronic disease must be evaluated frequently to assess disease activity.
Certain imaging findings have been previously described that represent characteristics of active inflammation of the small bowel, such as bowel-wall oedema, ulcerations, increased mesenteric vascularization, increased enhancement of the bowel wall, and mesenteric lymph nodes [7]. In the same study, but in a limited number of patients (n=13), the degree of contrast enhancement on T1-W spoiled gradient-echo images after gadolinium administration was increased in patients with active rather than inactive disease, but differences were not statistically significant. Inactive disease is characterized by absence of abnormality (i.e. optimal distension of bowel loops, healthy peristalsis, and no stenosis) or bowel-wall thickening with relatively low SI representing fibrosis with limited, homogeneous contrast enhancement [8]. In another study, Maccioni et al. [9] found a good statistical correlation between the biological activity and bowel-wall enhancement, wall hyperintensity on T2-W images, and T2 hyperintensity of fibrofatty proliferation on fat-suppressed images.
In the current study, we showed that the %CE of the bowel wall did not correlate with PCDAI values. Other studies have reported similar results. In a study of 82 adult patients, Schunk et al. [10] found that CDAI, which is considered to indicate CD activity, showed no correlation with the contrast-enhanced MRI findings, and accordingly MRI seems to be superior to these markers in terms of the recording of CD activity. In the same study, CRP showed a weak correlation with the MRI findings, while in our study, %CE in all dynamic phases was correlated with CRP values. To our knowledge, there are few studies in the literature on MR imaging of the small bowel in the paediatric population [11–13]. We found only one study by Laghi et al. [14] concerning the evaluation of disease activity with MRI. This group found a strong correlation between a semiquantitative score (reflecting bowel-wall contrast enhancement and thickening) and PCDAI in CD patients. However, bowel-wall contrast enhancement was qualitatively evaluated and based on visual inspection, rather than objective, quantitative measurements.
The lack of correlation may represent the largely subjective nature of the clinical activity indices and differences in patients’ perception and reporting. Our study, like most of the previously mentioned studies, suffered therefore from a major limitation. Disease activity may be definitively evaluated only by histology, which is impossible to obtain in all patients, especially from lesions in the small bowel. Therefore, most studies rely on CDAI or PCDAI, which are subjective indices. The CDAI was developed in 1976 [15] by the National Cooperative Crohn Disease Study and redefined in 1979 [16]. The CDAI reflects the degree of illness more closely than the degree of disease activity [17]. However, CDAI is largely based on subjective symptoms and complaints, and accordingly has been considered controversial since its introduction. In children, clinical evaluation of disease activity may be even more subjective due to incomplete cooperation, and this explains, in our opinion, the observed lack of correlation between PCDAI and %CE values, while in contrast, %CE values were correlated with CRP, which is a more objective marker of inflammation. We believe that disease activity can be determined by assessment of the degree of bowel wall enhancement. It is conceivable that the more severe the inflammation, the more the bowel wall enhances. The physiological mechanism for increased enhancement of inflamed tissues is by increased perfusion and increased capillary permeability [4, 18]. A further issue potentially influencing the contradictory results between ESR, CRP and disease activity as expressed by PCDAI in our population is the reported relatively poor sensitivity and specificity of CRP (41% and 78%, respectively) and of ESR (52% and 78%, respectively) in the assessment of IBD [19].
All studies agree that optimal, longstanding and homogeneous distension of the small bowel lumen is obligatory for correct radiological interpretation and in order to avoid false-negative and false-positive conclusions. However, there is no consensus about the technique for optimal small-bowel distension. In many studies, nasojejunal tube placement under fluoroscopic guidance is the usual technique for small-bowel preparation. According to these studies, confident, detailed evaluation of pathology of the small intestine requires consistently adequate luminal distension, which can be guaranteed only by intubation [20], as oral administration cannot provide sufficient distension and the accuracy of wall thickness measurements is therefore rather questionable [21]. However, this procedure of intubation and positioning of the catheter constitutes the most challenging aspect of the entire procedure and can be a very unpleasant or almost intolerable manoeuvre for both the patient and the radiologist [22]. More recently, studies have shown satisfactory small-bowel distension using different oral contrast media without oral intubation as compared with conventional enteroclysis [23]. Our protocol involves no exposure to radiation, as the water suspension is administered orally or through a nasogastric tube in uncooperative children. This procedure prolongs bowel preparation, but is well tolerated by paediatric patients, with excellent distension quality and results comparable to those of other studies, in terms of luminal distension without the need for fluoroscopy. The safety of this method is of value in CD, since many patients are young and of childbearing potential and require serial examinations.
Reports in the literature describe numerous oral contrast media suitable for use with MRI, including mannitol and sorbitol water solutions, iron oxide and barium sulphate suspensions, ispaghula husk or locust bean gum, planta ovata and pineapple juice [24–28]. Based on their pattern of SI in T1-W and T2-W imaging, oral contrast media are divided into so-called positive (increase in SI in T1-W and T2-W imaging) and negative (decrease in SI in T1-W and T2-W imaging) contrast media. In order to distend the small bowel, we used a water solution containing herbal fibres (psyllium), which is an isosmotic biphasic contrast agent appearing as low SI on T1-W images and high SI on T2-W images. Moreover, by using psyllium fibres instead of other hypertonic contrast agents such as mannitol, we avoided excessive diarrhoea as a side-effect of the procedure, which is an important issue in children. This substance is commonly used in the food industry as a thickening agent and has the property of retaining large amounts of water (up to 20–30 times its own volume). Our patients were placed in the prone position, a position that exerts mild pressure on the anterior abdominal wall, thus facilitating separation of the small bowel loops and decreasing the volume of peritoneal cavity to be imaged and thus the number of coronal sections to be acquired.
A possible limitation of this study was that patient selection may have been biased, as we did not enrol patients in remission, and thus no results were available from this group for comparison. Our patients, however, were symptomatic with a wide range of severity of symptoms when MRI was performed.
In 11 patients, MR imaging findings altered the therapeutic strategy, since endoscopic and histological findings in the large bowel were inconclusive for the type or severity of disease. Nine patients had a change of treatment: involvement of the terminal ileum was observed in eight with steroids added to their treatment, while one did not have imaging findings consistent with active disease, so the referring paediatric gastroenterologists decided to reduce the dose of steroids. Overall in two children with indeterminate colitis, we noted marked changes indicating ulcerative colitis rather than CD. These findings included exclusive involvement of the colon with sparing of the small bowel and total loss of haustral folds. On the basis of these findings, the diagnosis of ulcerative colitis was reinforced and total colectomy was suggested to the parents.
Conclusion
The MR imaging protocol that we have proposed is a feasible, well-tolerated imaging technique in children permitting assessment of disease extent, activity and extraluminal manifestations without the use of ionizing radiation.
References
Umschaden HW, Szolar D, Gasser J et al (2000) Small-bowel disease: comparison of MR enteroclysis images with conventional enteroclysis and surgical findings. Radiology 215:717–725
Maglinte DD, Siegelman ES, Kelvin FM (2000) MR enteroclysis: the future of small-bowel imaging? Radiology 215:639–641
Wiarda BM, Kuipers EJ, Houdijk LP et al (2005) MR enteroclysis: imaging technique of choice in diagnosis of small bowel diseases. Dig Dis Sci 50:1036–1040
Shoenut JP, Semelka RC, Magro CM et al (1994) Comparison of magnetic resonance imaging and endoscopy in distinguishing the type and severity of inflammatory bowel disease. J Clin Gastroenterol 19:31–35
Korman U, Kurugoglu S, Ogut G (2005) Conventional enteroclysis with complementary MR enteroclysis: a combination of small bowel imaging. Abdom Imaging 30:564–575
Kettritz U, Isaacs K, Warshauer DM et al (1995) Crohn's disease. Pilot study comparing MRI of the abdomen with clinical evaluation. J Clin Gastroenterol 21:249–253
Gourtsoyiannis N, Papanikolaou N, Grammatikakis J et al (2004) Assessment of Crohn's disease activity in the small bowel with MR and conventional enteroclysis: preliminary results. Eur Radiol 14:1017–1024
Wiarda BM, Kuipers EJ, Heitbrink MA et al (2006) MR enteroclysis of inflammatory small-bowel diseases. AJR 187:522–531
Maccioni F, Viscido A, Broglia L et al (2000) Evaluation of Crohn disease activity with magnetic resonance imaging. Abdom Imaging 25:219–228
Schunk K, Kern A, Oberholzer K et al (2000) Hydro-MRI in Crohn's disease: appraisal of disease activity. Invest Radiol 35:431–437
Applegate KE, Maglinte DD (2008) Imaging of the bowel in children: new imaging techniques. Pediatr Radiol 38(Suppl 2):S272–S274
Magnano G, Granata C, Barabino A et al (2003) Polyethylene glycol and contrast-enhanced MRI of Crohn's disease in children: preliminary experience. Pediatr Radiol 33:385–391
Toma P, Granata C, Magnano G et al (2007) CT and MRI of paediatric Crohn disease. Pediatr Radiol 37:1083–1092
Laghi A, Borrelli O, Paolantonio P et al (2003) Contrast enhanced magnetic resonance imaging of the terminal ileum in children with Crohn's disease. Gut 52:393–397
Best WR, Becktel JM, Singleton JW et al (1976) Development of a Crohn's disease activity index. National Cooperative Crohn's Disease Study. Gastroenterology 70:439–444
Best WR, Becktel JM, Singleton JW (1979) Rederived values of the eight coefficients of the Crohn's Disease Activity Index (CDAI). Gastroenterology 77:843–846
Singleton JW (1987) Clinical activity assessment in inflammatory bowel disease. Dig Dis Sci 32:42S–45S
Shoenut JP, Semelka RC, Silverman R et al (1993) Magnetic resonance imaging in inflammatory bowel disease. J Clin Gastroenterol 17:73–78
Canani RB, de Horatio LT, Terrin G et al (2006) Combined use of noninvasive tests is useful in the initial diagnostic approach to a child with suspected inflammatory bowel disease. J Pediatr Gastroenterol Nutr 42:9–15
Gourtsoyiannis N, Papanikolaou N, Grammatikakis J et al (2002) MR enteroclysis: technical considerations and clinical applications. Eur Radiol 12:2651–2658
Gourtsoyiannis NC, Papanikolaou N (2005) Magnetic resonance enteroclysis. Semin Ultrasound CT MR 26:237–246
Schreyer AG, Seitz J, Feuerbach S et al (2004) Modern imaging using computer tomography and magnetic resonance imaging for inflammatory bowel disease (IBD) AU1. Inflamm Bowel Dis 10:45–54
Reittner P, Goritschnig T, Petritsch W et al (2002) Multiplanar spiral CT enterography in patients with Crohn's disease using a negative oral contrast material: initial results of a noninvasive imaging approach. Eur Radiol 12:2253–2257
Hiraishi K, Narabayashi I, Fujita O et al (1995) Blueberry juice: preliminary evaluation as an oral contrast agent in gastrointestinal MR imaging. Radiology 194:119–123
Lauenstein TC, Schneemann H, Vogt FM et al (2003) Optimization of oral contrast agents for MR imaging of the small bowel. Radiology 228:279–283
Low RN, Francis IR (1997) MR imaging of the gastrointestinal tract with i.v. gadolinium and diluted barium oral contrast media compared with unenhanced MR imaging and CT. AJR 169:1051–1059
Patak MA, Froehlich JM, von Weymarn C et al (2001) Non-invasive distension of the small bowel for magnetic-resonance imaging. Lancet 358:987–988
Rubin DL, Muller HH, Young SW (1992) Formulation of radiographically detectable gastrointestinal contrast agents for magnetic resonance imaging: effects of a barium sulfate additive on MR contrast agent effectiveness. Magn Reson Med 23:154–165
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alexopoulou, E., Roma, E., Loggitsi, D. et al. Magnetic resonance imaging of the small bowel in children with idiopathic inflammatory bowel disease: evaluation of disease activity. Pediatr Radiol 39, 791–797 (2009). https://doi.org/10.1007/s00247-009-1272-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-009-1272-z