Abstract
We report a newborn with bilious vomiting and the rare combination of pyloric atresia, annular pancreas and ectopic drainage of the common bile duct into the lesser curvature of the gastric antrum. Radiologic, sonographic and percutaneous transhepatic transcholecystic cholangiographic (PTTC) findings, with surgical correlation, are presented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital variations of the extrahepatic biliary tree are common. It is rare, however, to identify ectopic drainage of the common bile duct (CBD) into regions of the gastrointestinal tract other than the second portion of the duodenum [1–3]. Pyloric atresia is another rare abnormality present in approximately 1:100,000 live births. These two conditions are discussed in the context of a patient with bilious vomiting who was found to have both abnormalities. Informed consent was obtained from the patient’s family to report this case.
Case report
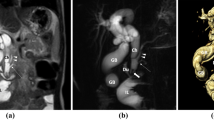
A premature girl born at 33 weeks’ gestation and weighing 2,130 g was born from a 28-year-old healthy G1P0 woman. The pregnancy was uneventful, although a routine 25-week obstetric US scan detected a prominent gastric bubble with no polyhydramnios. At birth, immediate resuscitative efforts were required and copious bilious vomiting was noted during intubation. The baby was stabilized and transferred to the neonatal intensive care unit. Abdominal plain films revealed a gastric bubble with no distal gas in the abdomen (Fig. 1). US showed a blunt-ending stomach with collapsed duodenum and transposed superior mesenteric artery and vein, suggestive of malrotation (Fig. 2). Subsequently, an upper gastrointestinal series demonstrated complete gastric outlet obstruction with no progression of contrast agent into the duodenum (Fig. 3).
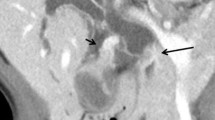
Based on the unusual findings of bilious vomiting with gastric outlet obstruction along with transposition of the superior mesenteric vessels, the baby was taken to the operating room for emergency laparotomy to ensure there was no malrotation. Operative findings included pyloric atresia with annular pancreas at the level of the pylorus, ectopic entry of the CBD into the gastric antrum, proximal jejunal diverticulum, anomalous origin of the right portal vein from the left portal vein, non-rotation and a congenital short small bowel (66 cm). A Ladd’s procedure was performed and the proximal jejunal diverticulum was excised primarily. The challenge was then to determine the best way to bypass the pyloric obstruction. Pyloroplasty was not an option because of its close proximity to the pancreas. A Roux-en-Y hepaticojejunostomy was not possible because of the short bowel. A gastrojejunostomy was performed to allow gastric emptying as well as biliary drainage. Total parenteral nutrition was started on the second day of life. Three days after surgery, the baby’s conjugated bilirubin levels began to rise and she became jaundiced. US showed normal intrahepatic biliary ducts, gallbladder sludge, and no evidence of gallstones. Eight days after surgery, a percutaneous transhepatic transcholecystic cholangiogram (PTTC) was performed to clear the biliary sludge and define the extrahepatic biliary tree. The cholangiogram demonstrated the CBD draining directly into the lesser curvature of the stomach (Fig. 4). The pancreatic duct was not visualized.
The baby had a complicated stay in hospital, primarily related to malabsorption from short bowel syndrome. She was fed semielemental formula but showed poor gut adaptation. The course was complicated with two episodes of necrotizing enterocolitis, as well as upper gastrointestinal hemorrhage, presumably from bile gastritis. The baby was discharged home at 4 months on home parenteral nutrition but was readmitted 2 weeks later with sepsis and fulminant liver failure. Despite intensive care, the baby’s condition deteriorated and she died of multiple organ failure.
Autopsy confirmed the pyloric atresia, annular pancreas, anomalous entry of the CBD into the gastric antrum, non-rotation, congenital short small bowel and cholestatic liver disease with fibrosis. No other extrahepatic biliary duct was identified.
Discussion
Ectopic drainage of the CBD is of clinical importance for a number of reasons. First, correct identification of an anomalous biliary drainage system prevents inadvertent damage of the biliary tree during operative procedures in children with bilious vomiting. Second, abnormal biliary drainage into the stomach and prolonged exposure of the gastric mucosa to bile juices has been shown to increase the risk of developing atrophic gastritis and gastric carcinoma. Finally, patients with ectopic drainage of the CBD have a higher incidence of biliary lithiasis, cholangitis, liver abscess and pancreatitis [1, 4].
Anatomic variations of the biliary tree are not uncommon; however, ectopic drainage of the CBD into regions other than the second portion of the duodenum are rare [1, 3]. During embryonic life, the liver originates from the ventral aspect of the primitive gut at the junction of the foregut and midgut, called the hepatic diverticulum. The hepatic diverticulum is divided by a transverse furrow into two portions called the pars hepatica and pars cystic. These portions eventually give rise to the liver parenchyma and gallbladder/cystic duct, respectively. The CBD originates from a common portion of the hepatic diverticulum, called the hepatic antrum [5]. Two theories are available for the explanation of an ectopic biliary duct. Bernard et al. [1] suggested that if a subdivision of the hepatic diverticulum occurs very early, the CBD would lie above the growth zone between the stomach and duodenum. The CBD would develop in this area and drain directly into the stomach [1]. Quintana and Labat [5] proposed that the development of an ectopic biliary drainage site is best explained by a random subdivision of the primary hepatic furrow, resulting always in a double CBD abnormality. In those patients with only one bile duct draining into an abnormal location, such as the duodenum or lesser curvature of the stomach (as in our patient), Quintana and Labat proposed that the other duct was obliterated during fetal life [5].
In 1968, Bockus classified the anatomic variations of the extrahepatic duct into seven types: (1) a single duct opening at the pylorus or antrum; (2) a single duct opening at the gastric fundus; (3) a single duct entering the duodenum, separate from the pancreatic duct; (4) a bifurcated duct with branches entering the duodenum; (5) a bifurcated duct with one branch entering the duodenum and the other the stomach; (6) separate ducts, with a 1-cm gap between, entering the duodenum; and (7) partition of the duct with two openings at the duodenum as described in Balbinot et al. [4]. From this classification, ectopic drainage of the CBD into the stomach presents in two ways: as a double CBD with an accessory bile duct draining to the stomach or as a single CBD draining into the stomach (extremely rare) [1, 6]. Only a handful of case reports document abnormal drainage of a single CBD into the lesser curvature of the gastric antrum [1, 5]. Kanematsu et al. [2] reviewed 56 cases of ectopic drainage in patients with the double CBD abnormality, and found that 52% drained into the duodenum, 46% drained into the stomach and 2% drained into the pancreatic duct [2]. Of those cases where the ectopic drainage of an accessory duct was into the stomach, 55% drained into the gastric body, 25% drained into the angulus (junction in the lesser curvature between the body and the antrum of the stomach) and 20% drained into the lesser curvature [1, 2].
The identification of ectopic CBD drainage has been reported using a variety of imaging modalities. These include barium meal study, US, PTTC, CT with biliscopin, endoscopic retrograde cholangiopancreatography (ERCP) and magnetic resonance cholangiopancreatography (MRCP) [6]. MRCP is the best modality as it provides information regarding the ducts and adjacent anatomy (liver, gallbladder, pancreas, bowel) in a noninvasive fashion and without radiation exposure. Unfortunately, ducts less than 1 mm in size are not well visualized with this imaging method because of poor spatial resolution of the biliary system, partial volume averaging and blur artefact caused by bowel, cardiac and respiratory motion. ERCP is also an adequate diagnostic tool when the drain orifice in the stomach can be identified. However, ERCP in neonates is challenging and technically difficult. Therefore, these methods might not be helpful and a more invasive examination such as PTTC might be necessary to define the biliary tree [7]. PTTC can be performed in neonates with a small-caliber needle, such as a 27G, significantly reducing the risk of bleeding after the procedure. Diluted nonionic iodinated contrast agent with normal saline (1:1) is used to decrease the chance of irritation of the gallbladder and biliary duct epithelium. Careful examination to prevent the injection of air is important to avoid the creation of air bubbles that could mistakenly be diagnosed as filling defects.
Other anomalies of the biliary tract and gallbladder as well as congenital duodenal anomalies (duodenal atresia, duodenal diverticulum) have been reported in association with ectopic drainage of the CBD. Gastric anomalies are not usually reported in association with ectopic CBD drainage. To the best of our knowledge, only one other case of bilious vomiting in a patient with pyloric atresia has been reported in the English language literature. This patient was slightly different from our patient as he presented with pyloric atresia, multiple associated intestinal atresias (duodenal and jejunal) and an anomalous pylorocholedochal tract, which the authors thought represented either a fistula or an ectopic accessory CBD. This patient had a normal CBD draining into the second portion of the duodenum [8]. Our patient had a single CBD draining into the stomach associated with pyloric atresia and annular pancreas, confirmed on autopsy.
In conclusion, the purpose of this case report was to review the abnormalities of ectopic bile duct drainage and to present a rare case of this entity combined with pyloric atresia. Although this finding is undoubtedly exceedingly rare, it is important to remember the possibility of ectopic bile duct drainage in the differential diagnosis of a newborn with bilious vomiting.
References
Bernard P, Le Borgne J, Dupas B et al (2001) Double common bile duct with ectopic drainage into the stomach. Case report and review of the literature. Surg Radiol Anat 23:269–272
Kanematsu M, Imaeda T, Seki M et al (1992) Accessory bile duct draining into the stomach: case report and review. Gastrointest Radiol 17:27–30
Sieber WK, Wiener ES, Chang J (1980) Double choledochus with ectopic drainage into the stomach – a rare congenital anomaly of the biliary ductal system. J Pediatr Surg 15:817–818
Balbinot RA, Gobbato A, Balbinot SS et al (2004) Double bile duct with ectopic drainage into stomach. Gastrointest Endosc 60:661–662
Quintana EV, Labat R (1974) Ectopic drainage of the common bile duct. Ann Surg 180:119–123
Amano Y, Takahashi M, Oishi T et al (2002) MR cholangiopancreatography of double common bile duct with ectopic drainage into stomach. J Comput Assist Tomogr 26:141–142
Meyers RL, Book LS, O’Gorman MA et al (2004) Percutaneous cholecysto-cholangiography in the diagnosis of obstructive jaundice in infants. J Pediatr Surg 39:16–18
Sencan A, Mir E, Karaca I et al (2002) Pyloric atresia associated with multiple intestinal atresias and pylorocholedochal fistula. J Pediatr Surg 37:1223–1224
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scheida, N., Wales, P.W., Krishnamurthy, G. et al. Ectopic drainage of the common bile duct into the lesser curvature of the gastric antrum in a newborn with pyloric atresia, annular pancreas and congenital short bowel syndrome. Pediatr Radiol 39, 66–69 (2009). https://doi.org/10.1007/s00247-008-1008-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-008-1008-5