Abstract
Hemangiomas, which are usually found in the skin, are extremely rare in an intradural location. An unusual case of capillary hemangioma intimate to the cauda equina is discussed. This entity has not previously been reported in the pediatric or adolescent population to the best of our knowledge, although it has been reported in adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemangiomas, usually seen as reddish-purple lesions in the skin or mucosa of the head and neck, are extremely rare in the central and peripheral nervous system. Histologically these lesions are characterized by lobules of capillary-sized vessels lined by flattened epithelium, supplied by a feeding vessel. Thoracic and lumbar intradural hemangiomas that have been described thus far have occurred in adults, mostly the middle-aged or elderly. Accurate recognition is important to raise the possibility of a highly vascular lesion prior to surgery. We discuss the clinical presentation of this lesion in a young adult, which was mostly similar to other spinal intradural tumors in this region, as well as with the imaging, surgical and histologic findings.
Case report
A 17-year-old boy presented with progressive low back pain, which radiated to the medial aspect of the knee and became progressively worse over 3–4 months to the extent that he could not sleep lying supine. He had significant constipation, which was ameliorated by cathartics. Although urinary symptoms were not reported, he had had encopresis as a child. Physical examination revealed limited flexion of the back to about 15–20°. He had clinical findings of S1 radiculopathy and diminished cremasteric on the left. No focal motor weakness or sensory deficits were observed in the lower extremities.
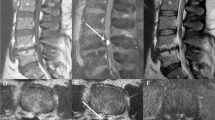
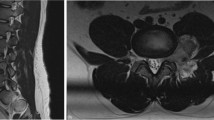
MRI revealed a well-demarcated intrathecal mass at L2–L3 nearly filling the thecal sac and splaying the nerve roots of the cauda equina. This measured approximately 2.1 cm craniocaudally, and 1.4 cm in the transverse and 1.3 cm in the AP dimensions. The mass did not extend through the neuroforamina nor expand the bony canal. The lesion was nearly isointense to the conus on T1-W images and was mildly hyperintense to the conus on T2-W images (Fig. 1). There was intense, homogeneous enhancement after contrast agent administration (Fig. 2). The conus medullaris and the distal filum terminale appeared unremarkable.
The patient had L2, L3 laminectomy with intradural exploration and gross total resection of the tumor. The mass was purplish and extremely vascular with almost cystic sinusoid-like vessels on the surface, which nearly filled the entire cross-sectional diameter of the canal at this level. There was a nerve root exiting from cephalad that was intimate to the mass and virtually indistinguishable. The nerve root needed to be transected.
The gross resected specimen was a lobulated mass partially covered by a smooth red surface. Histology revealed a proliferation of capillaries and vascular lumina lined by a single row of flat endothelial cells. A few areas of fibrosis were present. The proximal nerve root margin was an unremarkable myelinated nerve. These findings were consistent with a capillary hemangioma (Fig. 3).
Discussion
Capillary hemangiomas that are superficial lesions may arise from the blood vessels of the cauda equina nerve roots, the inner surface of the dura or pial surface of the cord. The histologic appearance of this lesion is quite similar to that of capillary hemangiomas of the central nervous system previously reported and distinct from those of vascular malformations or other vascular neoplasms [1, 2]. In one such case series of capillary hemangiomas of the central nervous system, the endothelial cells from these lesions demonstrated no positive staining for erythrocyte glucose transporter (GLUT-1), a selective marker for infantile hemangioma [2]. Spinal intradural capillary hemangiomas are very rare and fewer than 30 cases have been described so far, almost all of them in older adults. Amongst these, even fewer occurred in proximity to the cauda equina [3–6]. In the thoracic region, these intradural hemangiomas can have both intramedullary and extramedullary components [7]. Rare cases of capillary hemangioma disseminated in an intramedullary location and in a purely extradural location have also been reported [8].
The previously described intradural capillary hemangiomas have mostly a similar imaging appearance to that described here [1, 4]. These lesions are either hyperintense or of intermediate signal on T1-W sequences and moderately hyperintense on T2-W sequences. Intense, homogeneous enhancement was a notable feature seen in all the lesions described. There may be enlarged draining perimedullary veins, although we did not observe this feature [1]. The presence of such enlarged veins or small flow voids may raise the possibility of an extremely vascular tumor, such as hemangioblastoma, paraganglioma or even vascular malformations, though not necessarily a hemangioma. In such cases, preoperative spinal arteriography or MR angiography can be considered.
The most common differentials for an enhancing intradural tumor of the cauda equina in this age group are the myxopapillary variant of ependymoma and schwannoma. Myxopapillary ependymomas are mucoid tumors that have a distinct predilection for the conus medullaris or filum terminale and are thought to arise from the ependymal glia of the filum terminale. Cysts are a common feature in these lesions. The “cap sign,” a rim of extreme hypointensity at the poles of the tumor on T2-W images, results from hemorrhage and hemosiderin deposition. This finding is common in ependymomas and also in other highly vascular tumors such as paragangliomas or hemangioblastomas. Schwannomas also intensely enhance after contrast agent administration and not infrequently show cystic change or necrosis. Paragangliomas, frequently found in the cauda equina, are rare in this age group, as are meningiomas. Enhancing lesions from sarcoidosis, drop metastases and lymphoma can be seen in this region, but are rarely solitary. Hemangioblastomas are usually intramedullary lesions and are more common in the thoracic and cervical regions. In the absence of additional features such as cysts, hemorrhage, dilated feeding vessels or flow voids, these other lesions are virtually indistinguishable from capillary hemangiomas.
In conclusion, capillary hemangioma can be considered as one of the rare differentials when a homogeneously enhancing intradural extramedullary mass is seen. Hemangiomas, despite the rarity of occurrence in this location, need to be recognized because of the risk of hemorrhage in addition to a mass effect that may result in neurologic compromise.
References
Abdullah DC, Raghuram K, Phillips CD et al (2004) Thoracic intradural extramedullary capillary hemangioma. AJNR 25:1294–1296
Abe M, Misago N, Tanaka S et al (2005) Capillary hemangioma of the central nervous system: a comparative study with lobular capillary hemangioma of the skin. Acta Neuropathol 109:151–158
Kim KJ, Lee JY, Lee SH (2006) Spinal intradural capillary hemangioma. Surg Neurol 66:212–214
Choi BY, Chang KH, Choe G et al (2001) Spinal intradural extramedullary capillary hemangioma: MR imaging findings. AJNR 22:799–802
Holtzman RN, Brisson PM, Pearl RE et al (1999) Lobular capillary hemangioma of the cauda equina. J Neurosurg 90:239–241
Mastronardi L, Guiducci A, Frondizi D (1997) Intraneural capillary hemangioma of the cauda equina. Eur Spine J 6:278–280
Shin JH, Lee HK, Jeon SR et al (2000) Spinal intradural capillary hemangioma: MR findings. AJNR 21:954–956
Badinand C, Morel N, Kopp VA et al (2003) Dumbbell-shaped epidural capillary hemangioma B. AJNR 24:190–192
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ganapathy, S., Kleiner, L.I., Mirkin, L.D. et al. Intradural capillary hemangioma of the cauda equina. Pediatr Radiol 38, 1235–1238 (2008). https://doi.org/10.1007/s00247-008-0947-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-008-0947-1