Abstract
Background
Mediastinal aortic vascular anomalies are relatively common causes of extrinsic central airway narrowing in infants with respiratory symptoms. Surgical correction of mediastinal aortic vascular anomalies alone might not adequately treat airway symptoms if extrinsic narrowing is accompanied by intrinsic tracheomalacia (TM), a condition that escapes detection on routine end-inspiratory imaging. Paired inspiratory–expiratory multidetector CT (MDCT) has the potential to facilitate early diagnosis and timely management of TM in symptomatic infants with mediastinal aortic vascular anomalies.
Objective
To assess the technical feasibility of paired inspiratory–expiratory MDCT for evaluating TM among symptomatic infants with mediastinal aortic vascular anomalies.
Materials and methods
The study group consisted of five consecutive symptomatic infants (four male, one female; mean age 4.1 months, age range 2 weeks to 6 months) with mediastinal aortic vascular anomalies who were referred for paired inspiratory–expiratory MDCT during a 22-month period. CT angiography was concurrently performed during the end-inspiration phase of the study. Two pediatric radiologists in consensus reviewed all CT images in a randomized and blinded fashion. The end-inspiration and end-expiration CT images were reviewed for the presence and severity of tracheal narrowing. TM was defined as ≥50% reduction in tracheal cross-sectional luminal area between end-inspiration and end-expiration. The presence of TM was compared to the bronchoscopy results when available (n = 4).
Results
Paired inspiratory–expiratory MDCT was technically successful in all five patients. Mediastinal aortic vascular anomalies included a right aortic arch with an aberrant left subclavian artery (n = 2), innominate artery compression (n = 2), and a left aortic arch with an aberrant right subclavian artery (n = 1). Three (60%) of the five patients demonstrated focal TM at the level of mediastinal aortic vascular anomalies. The CT results were concordant with the results of bronchoscopy in all patients who underwent bronchoscopy (n = 4).
Conclusion
Paired inspiratory–expiratory MDCT is technically feasible for evaluating TM in symptomatic infants with mediastinal aortic vascular anomalies and has the potential to facilitate prompt diagnosis and treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mediastinal aortic vascular anomalies are a relatively common cause of extrinsic central airway narrowing in infants with respiratory symptoms. Surgical decompression or resection of the underlying mediastinal aortic vascular anomaly is the currently accepted standard treatment, which improves the morbidity and mortality in most patients [1–5]. However, surgical correction of mediastinal aortic vascular anomalies alone might not adequately treat airway symptoms if extrinsic compression is accompanied by intrinsic tracheomalacia (TM), a condition characterized by weakness of the airway walls and associated excessive expiratory collapsibility [6–12]. This condition escapes detection on routine end-inspiratory imaging, and a delay in diagnosis can result in the need for a second surgical procedure.
In the past, the diagnosis of TM in infants often required bronchoscopy, but bronchoscopy has inherent disadvantages, particularly in infants who are already in respiratory distress, because of its invasiveness and inability to completely evaluate adjacent extraluminal mediastinal structures including anomalous or abnormally positioned aortic vessels. Recently, however, Chan et al. [13] reported the successful detection of TM with paired inspiratory-expiratory MDCT in a 2-month-old infant presenting with respiratory distress caused by TM associated with a double aortic arch. These authors emphasized that the preoperative diagnosis of TM associated with mediastinal aortic vascular anomalies can prevent the need for a second surgical procedure.
A larger case series is needed to establish whether paired inspiratory–expiratory MDCT can be routinely applied for evaluating TM in symptomatic infants with mediastinal aortic vascular anomalies. Thus, the goal of this study was to assess the technical feasibility of evaluating TM with paired inspiratory–expiratory MDCT in symptomatic infants with mediastinal aortic vascular anomalies.
Materials and methods
Patients
Our hospital’s Institutional Review Board (IRB) approved the review of radiologic and clinical data for this study. Informed consent was waived by the IRB for this retrospective analysis, but patient confidentiality was protected. Included in the study were all consecutive infants referred for respiratory symptoms who underwent paired inspiratory–expiratory MDCT between 1 October 2004 and 1 August 2006, and who had a subsequent final diagnosis of mediastinal aortic vascular anomaly. Our hospital digital archiving system identified a total of five patients (four boys and one girl), with a mean age of 4.1 months (range 2 weeks to 6 months). They comprised the patient population in our study.
CT protocol
All patients underwent CT studies using our department’s standard paired inspiratory–expiratory MDCT airway protocol with either a 16-row detector scanner (n = 4) (LightSpeed 16, General Electric Medical Systems, Milwaukee, WI) or a 64-row detector scanner (n = 1) (Sensation 64, Siemens Medical Solutions, Erlangen, Germany). The protocol includes imaging during two different phases of respiration: end-inspiration and end-expiration.
CT parameters included 0.75-mm collimation (for 16 MDCT) and 0.6-mm collimation (for 64 MDCT), with weight-based low-dose tube current and kilovoltage, high speed mode, and a pitch equivalent of 1.0 to 1.5 [14]. Scanning was performed for both end-inspiratory and end-expiratory imaging with the patients in the supine position. Prior to CT scanning, initial scout topographic images were obtained to determine the area of coverage, which extended from the most superior portion of the trachea to the level of the diaphragm.
All five infants in our study required general anesthesia and intubation. End-inspiratory and end-expiratory phases of the CT scanning were obtained by alternatively applying and withholding positive pressure ventilation during inspiration and expiration, respectively. After consultation with a pulmonologist for consistency of results, end-inspiratory pressure was always held to 15–20 cm H2O. By keeping these pressures consistent, we avoided having airway diameters artificially larger than physiologically normal simply as a result of excessive airway pressure.
The end-inspiration phase of the CT scanning was performed using contrast-enhanced CT angiography in all patients after intravenous injection of 2 ml/kg (not exceeding 125 ml) of nonionic contrast medium (320 mg I/ml). In patients with antecubital catheters (n = 3), contrast medium was injected with a power injector at a rate of 1.0 ml/s for a 24-gauge catheter. Manual injection was used when intravenous access was secured via a catheter placed in the dorsum of the hand in two patients. Scanning initiation was started by the radiologist and CT technologist when optimal contrast enhancement was observed in the proximal descending aorta or left ventricle on the monitoring scan.
CT image review and evaluation
All CT images were reviewed in a randomized, blinded fashion by an experienced pediatric radiologist and second-year pediatric radiology fellow in consensus on a PACS workstation (Fujifilm Medical Systems, Stamford, CT) using standard soft-tissue (e.g., level 40–50 HU, width 400–450 HU) and lung (e.g., level −450–550 HU, width 1,600–1,800 HU) window settings. To minimize potential bias, the end-inspiratory and end-expiratory CT images for each patient were reviewed out of sequence so that the radiologist was unaware of a subject’s end-inspiratory scan findings when reviewing the end-expiratory scan, and vice versa.
The CT images were reviewed for the type of mediastinal aortic vascular anomaly and the degree of airway narrowing at the level of the anomaly. The tracheal lumen was measured using a computerized tracing tool that is part of our hospital’s PACS system. For each scan, the region of maximal tracheal narrowing at the level of mediastinal aortic vascular anomaly was identified and, using an electronic tool, the inner wall of the airway was hand-traced at the desired level and the cross-sectional area of the airway in square millimeters was calculated. End-inspiratory and end-expiratory scans were carefully compared to ensure that airway lumen measurements were obtained at the same level. For each patient, the percentage expiratory tracheal collapse was calculated by comparing the reduction in cross-sectional area between images from each end-expiratory sequence and the end-inspiratory sequences obtained at the same level. The standard CT criterion of ≥50% reduction in cross-sectional luminal area was applied for establishing the diagnosis of TM [7–9, 11]. By applying this criterion at the level of a mediastinal aortic vascular anomaly, the diagnosis of TM was determined [7–9, 11]. The trachea was also routinely assessed above and below the level of the vascular anomaly in order to determine whether diffuse TM was present. The equation for calculating percentage luminal collapse between inspiration and expiration was as follows: luminal collapse (%) = [1 − (luminal area of airway at end-expiration)/(luminal area of airway at end-inspiration)] ×100.
Bronchoscopic evaluation
Four out of five patients (80%) underwent bronchoscopy, either before or after CT examination. The presence or absence of TM was recorded.
Results
Study cohort
The patient characteristics are summarized in Table 1.
Patient characteristics
There were four boys and one girl with ages ranging from 2 weeks to 6 months and a mean age of 4.1 months. Each of the five patients presented with respiratory symptoms including stridor (n = 3) and apnea (n = 2). Other relevant symptoms included recurrent infection (n = 2) and failure to extubate (n = 1).
Diagnosis of mediastinal aortic vascular anomalies
There were three types of mediastinal aortic vascular anomalies in our study: a right aortic arch with an aberrant left subclavian artery (n = 2), innominate artery compression (n = 2), and a left aortic arch with an aberrant right subclavian artery (n = 1).
A right aortic arch with aberrant left subclavian artery was diagnosed when an aberrant left subclavian artery arising from the right aortic arch coursed behind the esophagus to the left hemithorax. Innominate artery compression was diagnosed when the innominate artery arising from the left aortic arch resulted in anterior tracheal compression while crossing to the right of the trachea. A left aortic arch with aberrant right subclavian artery was diagnosed when an aberrant right subclavian artery arising from the left aortic arch coursed behind the esophagus to the right hemithorax [15].
CT imaging findings
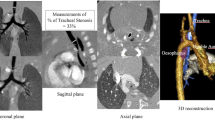
The CT imaging findings are shown in Table 1. Three (60%) of the five patients demonstrated TM. The TM in all three patients was focal in distribution, and located only at the level of the mediastinal aortic vascular anomaly. Both patients with the innominate artery narrowing the airway showed TM. One of the two patients with a right aortic arch with an aberrant left subclavian artery showed TM (Fig. 1). TM was not detected in the patient with a left aortic arch with an aberrant right subclavian artery (Fig. 2).
Axial CT images using the soft-tissue window in patient 1, a 5-month-old boy who presented with apnea: a at end-inspiration, b at end-expiration. On bronchoscopy, TM was seen at the aortic arch level. At end-inspiration (a) a right aortic arch (RA) and patent trachea (arrow) are seen. At end-expiration (b) almost complete expiratory collapse of the trachea (arrow) in seen, meeting CT criteria for TM (RA right aortic arch)
Axial CT images using the soft-tissue window in patient 5, a 2-week-old boy who presented with recurrent stridor: a at end-inspiration, b at end-expiration. At end-inspiration (a) a left aortic arch (LA) with an aberrant right subclavian artery (arrow) are seen. The trachea is patent. Note the nasogastric tube (arrowhead). At end-expiration (b) again a left aortic arch (LA) with an aberrant right subclavian artery (arrow) are seen. There is only a mild expiratory decrease (<50%) in the caliber of the trachea, which does not meet CT criteria for TM. Again, note the nasogastric tube (arrowhead)
Table 2 shows the cross-sectional area of the trachea during inspiration and expiration, and the percentage tracheal airway collapse at the level of the mediastinal vascular anomaly for each patient. The range of cross-sectional areas at the tracheal narrowing at inspiration was 5.57 mm2 to 26.46 mm2, with an average of 16.72 mm2. The range of cross-sectional areas at the tracheal narrowing at expiration was 0 mm2 to 26.35 mm2, with an average of 9.22 mm2. The range of percentage of airway collapse in the patients without TM was 0.3% to 27.4%, with an average of 13.9%. The range of percentage of airway collapse in the patients with TM was 95.6% to 100%, with an average of 98.5%.
Bronchoscopic findings
The bronchoscopic results are shown in Table 1. Four out of five patients (80%) underwent bronchoscopy either before or after CT study. In all four patients who underwent bronchoscopy, there was concordance between the bronchoscopy findings and the CT findings as to the presence (three patients) or absence (one patient) of TM.
Discussion
TM is defined as a weakness of the tracheobronchial wall and supporting cartilage that results in increased compliance and excessive expiratory collapsibility [6–11]. This disorder can arise congenitally from impaired cartilage maturation or might be secondarily acquired from prior intubation, infection, or longstanding extrinsic airway compression caused by adjacent mediastinal structures such as anomalous or abnormally positioned vessels [6, 13].
It is well-known that infants with mediastinal aortic vascular anomalies resulting in extrinsic central airway narrowing and/or associated TM can present with nonspecific respiratory symptoms such as cough, stridor, wheezing, and apnea [1, 7, 13]. For these symptomatic infants, early diagnosis and subsequent surgical decompression or resection of the underlying mediastinal aortic vascular anomalies are currently considered standard management, which improves the morbidity and mortality [1–5]. However, surgical correction of mediastinal aortic vascular anomalies alone might not adequately treat airway symptoms if extrinsic compression is accompanied by intrinsic TM. Although the course of TM associated with mediastinal aortic vascular anomalies in infants can be self-limited in some cases, persistent TM resulting in respiratory symptoms in infants should be detected early and correctly so that proper patient management can be achieved.
In this study, we showed that paired inspiratory–expiratory MDCT is technically feasible for evaluation of TM in a case series of five symptomatic infants with mediastinal aortic vascular anomalies. We found a high prevalence (60%) of TM among symptomatic infants with mediastinal aortic vascular anomalies. Notably, this important finding would have gone undetected in three out of three patients (100%) if only traditional end-inspiratory imaging had been performed. Thus, our results emphasize the need to perform dedicated expiratory imaging in order to detect this important condition.
The protocol that we employed was recently described by Chan et al. [13], who reported the successful use of applying and withholding positive ventilatory pressures alternately to simulate inspiratory and expiratory phases for MDCT imaging of TM in a 2-month-old infant with a double aortic arch and TM. All five infants in our study were intubated in preparation for the paired inspiratory–expiratory MDCT. We would emphasize that the presence of the endotracheal tube and airway pressure affect the compliance of the trachea and its ability to collapse. It is important that the end-inspiratory pressure is always held to 15–20 cm H2O to achieve consistent results. By keeping these pressures constant, obtaining airway diameters artificially larger than physiologically normal simply as a result of excessive airway pressure can be avoided.
This MDCT protocol was applied successfully in all five infants in our case series and the MDCT findings were concordant with the bronchoscopy findings in all four patients who underwent this procedure. Although bronchoscopy has been considered the gold standard for the diagnosis and assessment of airway abnormalities including TM [16], it is an invasive procedure with inherent risks, particularly in infants who are already in respiratory distress. In addition, bronchoscopy is limited in evaluating extraluminal mediastinal vascular anomalies associated with TM in these infants. Based upon our results, we believe that the paired inspiratory–expiratory MDCT technique can obviate the need for more invasive techniques such as bronchoscopy for evaluating TM, and should be routinely applied in the preoperative assessment of TM in symptomatic infants with mediastinal aortic vascular anomalies.
With the advent of CT, particularly now MDCT, it has become possible to obtain a complete objective and reproducible evaluation of the central airways, adjacent mediastinal structures, and lung parenchyma [8, 11, 13, 17–21]. In the past, evaluation of tracheal dynamics in infants was a complex process, often requiring multiple imaging modalities as well as invasive procedures such as bronchoscopy. Currently available imaging modalities including fluoroscopy-guided airway study and MRI are potentially useful in evaluating tracheal dynamics in infants. Although fluoroscopy can demonstrate central airway compression and/or narrowing, it is a very operator-dependent procedure and its findings are often nonspecific. Moreover, the evaluation of mediastinal vessels is markedly limited with a fluoroscopy-guided airway study. For imaging evaluation of infants with mediastinal vascular anomalies, MRI has proved to be useful and does not expose the patient to ionizing radiation [22, 23]. However, MDCT has potential advantages over MRI in evaluating infants with symptomatic tracheal narrowing from mediastinal aortic vascular anomalies. First, because of its fast scanning times, MDCT is less likely to require sedation and is therefore associated with fewer sedation-related complications in children [24, 25]. Second, unlike MRI, which has a limited role in evaluating central airway and lung parenchyma, MDCT can provide high-resolution images of central airway and lung parenchyma. Although MDCT involves ionizing radiation, the use of age- and weight-appropriate parameters ensures that the lowest level of exposure necessary for diagnosis is used.
Following the results of our study, we believe that a complete evaluation of both TM and mediastinal aortic vascular anomalies can be expeditiously accomplished by combining a paired inspiratory–expiratory MDCT study with CT angiography. This is particularly important in infants with vascular rings or innominate artery compression of the central airway in whom surgical treatment requires precise knowledge of the mediastinal vascular anatomy. Similar to prior reports, we found that an MDCT angiography protocol is beneficial for evaluation of mediastinal aortic vascular anomalies and associated airway disorder in infants [13, 18, 21].
We acknowledge that our study was limited by the small number of patients. We plan a larger multicenter study seeking to confirm these preliminary results in a larger cohort. Such a study will also provide the statistical power to determine the prevalence of TM among patients with various mediastinal aortic vascular anomalies. Second, although we were aware that recently published studies in adult patients have shown that active dynamic expiratory and coughing-maneuver CT studies are more sensitive than end-expiratory CT studies for evaluation of TM [8, 26], these techniques require the patient to follow directions, and our patients were infants.
Radiation exposure is a factor that also needs to be seriously considered when CT is performed, especially in infants. Radiation exposure is directly proportional to tube current. Although the CT studies performed in this study were done with the same radiation dose during the end-inspiration and end-expiration phases, we anticipate that further dose reductions will be possible and are exploring this issue in an on-going dose-reduction protocol [27].
Conclusion
Paired inspiratory–expiratory MDCT is technically feasible and should be considered for the assessment of TM in symptomatic infants with mediastinal aortic vascular anomalies. Prompt and accurate diagnosis of TM associated with mediastinal aortic vascular anomalies using paired inspiratory–expiratory MDCT has the potential to improve the surgical management of infants with this underdiagnosed but important disorder.
References
Erwin EA, Gerber ME, Cotton RT (1997) Vascular compression of the airway: indications for and results of surgical management. Int J Pediatr Otorhinolaryngol 40:155–162
Anand R, Dooley KJ, Williams WH et al (1994) Follow-up of surgical correction of vascular anomalies causing tracheobronchial compression. Pediatr Cardiol 15:58–61
Han MT, Hall DG, Manche A et al (1993) Double aortic arch causing tracheoesophageal compression. Am J Surg 165:628–631
Sebening C, Jakob H, Tochtermann U et al (2000) Vascular tracheobronchial compression syndromes – experience in surgical treatment and literature review. Thorac Cardiovasc Surg 48:164–174
Horvath P, Hucin B, Hruda J et al (1992) Intermediate to late results of surgical relief of vascular tracheobronchial compression. Eur J Cardiothorac Surg 6:366–371
Paston F, Bye M (1996) Tracheomalacia. Pediatr Rev 17:328
Carden KA, Boiselle PM, Waltz DA et al (2005) Tracheomalacia and tracheobronchomalacia in children and adults: an in-depth review. Chest 127:984–1005
Baroni RH, Feller-Kopman DF, Nishino M et al (2005) Tracheobronchomalacia: comparison between end-expiratory and dynamic expiratory CT for evaluation of central airway collapse. Radiology 235:635–641
Gilkeson RC, Ciancibello LM, Hejal RB et al (2001) Tracheobronchomalacia: dynamic airway evaluation with multidetector CT. AJR 176:205–210
Hein E, Rogalla P, Hentschel C et al (2000) Dynamic and quantitative assessment of tracheomalacia by electron beam tomography: correlation with clinical symptoms and bronchoscopy. J Comput Assist Tomogr 24:247–252
Zhang J, Hasegawa I, Hatabu H et al (2004) Frequency and severity of air trapping at dynamic expiratory CT in patients with tracheobronchomalacia. AJR 182:81–85
Fleck RJ, Pacharn P, Fricke B et al (2002) Imaging findings in pediatric patients with persistent airway symptoms after surgery for double aortic arch. AJR 178:1275–1279
Chan MS, Chu WC, Cheung KL et al (2005) Angiography and dynamic airway evaluation with MDCT in the diagnosis of double aortic arch associated with tracheomalacia. AJR 185:1248–1251
Bhalla S, Siegel MJ (2002) Multislice computed tomography in pediatrics. In: Silverman PM (eds) Multislice computed tomography: a practical approach to clinical protocols. Lippincott Williams & Wilkins, Philadelphia, pp 231–282
Higgins CB, Roos AD (2006) MRI and CT of the cardiovascular system. Lippincott Williams & Wilkins, Philadelphia, pp 441–468
Naidich DP, Harkin TJ (1995) Airways and lungs: correlation of CT with fiberoptic bronchoscopy. Radiology 197:1–12
Boiselle PM, Ernst A (2002) Multiplanar and three-dimensional imaging of the central airways with multidetector CT. AJR 179:301–308
Lee EY, Siegel MJ, Hildebolt CF et al (2004) MDCT evaluation of thoracic aortic anomalies in pediatric patients and young adults: comparison of axial, multiplanar, and 3D images. AJR 182:777–784
Siegel MJ (2003) Multiplanar and three-dimensional multi-detector row CT of thoracic vessels and airways in the pediatric patients. Radiology 229:641–650
Boiselle PM, Lee KS, Ernst A (2005) Multidetector CT of the central airways. J Thorac Imaging 20:186–195
Lee EY, Siegel MJ (2007) MDCT of tracheobronchial narrowing in pediatric patients. J Thorac Imaging 22:300–309
Russo V, Renzulli M, Palombra CL et al (2006) Congenital diseases of the thoracic aorta: role of MRI and MRA. Eur Radiol 16:676–684
Hernandez RJ (2002) Magnetic resonance imaging of mediastinal vessels. Magn Reson Imaging Clin N Am 10:237–251
Papas JN, Donnelly LF, Frush DP (2000) Reduced frequency of sedation of young children with multisection helical CT. AJR 182:777–784
Lemos AA, Siegel MJ, Rossi G et al (2006) Single- versus multidetector-row CT: comparison of sedation rates, conventional angiograms and motion artifacts in young children following liver transplantation. Radiol Med 111:911–920
Boiselle PM, Lee KS, Lin S et al (2006) Cine CT during coughing for assessment of tracheomalacia: preliminary experience with 64-MDCT. AJR 204:565–573
Zhang J, Hasegawa I, Feller-Kopman D et al (2003) 2003 AUR Memorial Award. Dynamic expiratory volumetric CT imaging of the central airways: comparison of standard-dose and low-dose techniques. Acad Radiol 10:719–724
Acknowledgements
This work was supported in part by a GE-AUR Research Award, a Society of Thoracic Radiology Research Grant, and a Society for Pediatric Radiology Research Fellow Grant (E.Y.L.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, E.Y., Mason, K.P., Zurakowski, D. et al. MDCT assessment of tracheomalacia in symptomatic infants with mediastinal aortic vascular anomalies: preliminary technical experience. Pediatr Radiol 38, 82–88 (2008). https://doi.org/10.1007/s00247-007-0672-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-007-0672-1