Abstract
Background
Diffuse marrow replacement in acute leukemia is well known, but there are few reports describing the MRI features of pediatric leukemic relapse.
Objective
Our purpose was to describe the MRI appearance of pediatric leukemic relapse.
Materials and methods
A total of 53 consecutive children with a history of ALL were referred for musculoskeletal MRI from 1 January 1998 to 28 February 2007 at one center, and from 1 January 2000 to 2 May 2007 at a second center. From this group, 14 children seen at initial diagnosis of leukemia and 2 children who underwent MRI after therapy for relapse were excluded. The remaining 37 children, 8 with relapse and 29 in remission, were studied. Images of patients with relapse and in remission were reviewed for type and configuration of marrow infiltration; coexisting marrow alterations including osteonecrosis or stress reaction were also reviewed.
Results
All eight children with relapse demonstrated nodular lesions with well-defined margins. Coexisting osteonecrosis was present in three children (38%) and pathologic fracture in one. Among the 29 children in remission, 9 showed stress reaction/fracture, 14 showed osteonecrosis and 9 showed ill-defined nodules, and in 5 the marrow was completely normal.
Conclusion
Well-defined nodules in all patients with leukemic relapse suggest that this appearance is characteristic and distinct from the published findings of diffuse marrow replacement in acute leukemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute leukemia is the most common malignancy in children. The prognosis of acute lymphoblastic leukemia (ALL) is excellent at initial presentation with complete remission rates with multidrug induction chemotherapy of up to 98% in children [1]. Leukemic relapse, however, carries a poor prognosis when the relapse occurs within 18 months, and there is a 30% event-free survival rate if relapse occurs more than 3 years after initial diagnosis [2]. The most common site of leukemic relapse is the marrow, with isolated marrow involvement seen in 48% of patients in one study [3]. Musculoskeletal MRI of children with a history of leukemia may demonstrate complications from therapy or from the disease process itself, which include osteonecrosis and stress injuries related to osteopenia [4]. Diagnostic dilemmas arise when determining whether signal alteration in the marrow represents residual red marrow, developing stress injury, osteonecrosis, or the initial manifestations of leukemic relapse. Although ultimately marrow biopsy will be required to confirm disease status and plan subsequent therapy, recognition of a characteristic lesion at MRI may identify the patients requiring biopsy and expedite appropriate management.
MRI features of leukemia at initial presentation have been well described, and comprise diffuse marrow cellularity or infiltration seen as elevated signal intensity (SI) on fluid-sensitive sequences and diffuse decrease in SI on T1-weighted (T1-W) sequences [5–7]. However, reports of musculoskeletal MRI features of leukemic relapse consist largely of case reports and there are a limited number of descriptions in pediatric patients [8–10]. Therefore, the purpose of this study was to describe our MRI observations in eight children with biopsy-proven leukemic relapse and compare these to other symptomatic leukemic survivors without relapse. To our knowledge, this is the largest consecutive MRI series in children with leukemic relapse.
Materials and methods
Patient selection
This was a retrospective study at two tertiary care children’s hospitals with Institutional Review Board approval. At one institution that serves only children, a text word search of pathology reports with the terms “lymphoblastic,” “leukemic” and “leukemia” generated a total of 545 patients between 1 January 1998 and 1 April 2005. From these patients, a total of 45 children had musculoskeletal MRI examinations. At the second institution, which serves children and adults, a leukemia pathology diagnostic code search generated 481 patients from 1 January 2000 to 2 May 2007. Of these patients, 13 children had musculoskeletal MRI examinations, for a total of 58 pediatric patients.
Among these 58 children, 14 were newly diagnosed, 10 showed relapse, and 34 were in remission. The 14 children seen at initial diagnosis were excluded. One patient with leukemic relapse was excluded because the MRI was performed 462 days after the diagnosis of relapse. A second patient with leukemic relapse was excluded because the MRI was performed 39 days after diagnosis of relapse and therapy had already begun. Of the 34 patients in remission, 5 with acute or chronic myelogenous leukemia were excluded. Therefore, the total numbers of patients with ALL from both institutions with relapse and in remission were 8 and 29, respectively, and these constituted our study and control populations.
Patients with relapse
The mean age of the patients with leukemic relapse was 12.6 years (range 4.6–19.7 years), and three of the eight were males. All MRI examinations were requested because of musculoskeletal pain. None of these patients was on therapy for relapsed disease at the time of imaging. No patients were on granulocyte colony-stimulating factor at the time of imaging. Diagnosis was proven by pathology. MRI was performed an average of 11.4 days (range 1–39 days) prior to pathological diagnosis of leukemic relapse. Among the eight patients, the MRI examinations included the pelvis in four patients, the ankle in one, the knee in one, the knee with ankle in one, and the pelvis with knee in one.
Patients in remission
The mean age of the patients in remission was 10.6 years (range 3.7–18.6 years) and 16 of the 29 were males. All MRI examinations were requested because of musculoskeletal pain. Initial diagnosis had been proved by pathology. Proof that the patient was in remission was either by negative subsequent pathology results and/or at least 1 year of clinical follow-up from the time of the MRI examination with no laboratory or clinical evidence of relapse. Among the 29 patients, the MRI included the ankle in eight patients, the pelvis in six, the knee in six, the femur in three, the shoulder in two, the humerus in one, the tibia in one, the femur with tibia in one, and the knee with ankle in one.
Imaging analysis
MRI was performed on a 1.5-T Philips Intera (Best, The Netherlands) or a 1.5-T GE Advantage (Milwaukee, Wis.) scanner. For all patients and controls, a bi- or triplane fluid-sensitive (T2-W sequence with fat saturation, a proton density sequence with fat saturation, or STIR sequence), a single-plane T1-W non-fat-saturated sequence, and a single-plane susceptibility (either 2-D or 3-D GRE with fat suppression) sequence were obtained. For all patients and controls, a single or biplane T1-W fat-saturated sequence after gadolinium administration was also obtained.
Images were evaluated by a board-certified pediatric radiologist with additional musculoskeletal radiology fellowship training and 2 years of experience in the evaluation of nodular or diffuse marrow infiltration, sharp or poorly defined margins, associated juxtacortical soft-tissue mass, and multiplicity of nodules; coexisting marrow alterations including osteonecrosis or stress injury were also reviewed and recorded. When nodules were present, the location of these nodules was recorded (pelvis, small bones of the feet, or specific location within the long tubular bones—epiphysis/metaphysis/diaphysis) for both control and study patients. MR images of eight relapse patients were additionally reviewed by consensus with a second board-certified pediatric radiologist with 14 years of experience using the same data points, who was blinded to the diagnosis and who reviewed the studies mixed with leukemic patients who had undergone musculoskeletal MRI at the time of initial presentation or who were in remission.
A chart review of the initial radiology reports for the study and control populations was performed to specifically determine whether the correct diagnosis of relapse/no relapse was made at the initial interpretation.
Results
Patients with relapse
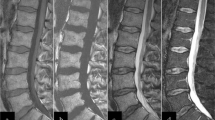
All eight children with biopsy-proven leukemic relapse had abnormal marrow changes. Multiple, well-defined nodules were present in seven children (Figs. 1 and 2) and a single heterogeneous nodule with a corrugated but still well-defined margin was present in one patient (Fig. 3). Using the criteria of nodular disease with well-defined margins, all eight children were correctly identified as having leukemic relapse by the second reader blinded to the final diagnosis. For all five children with MRI of the pelvis, the pelvis was replaced with multiple, well-defined nodules (Fig. 1). For both patients with MRI of the ankle, multiple, well-defined nodules involved multiple small bones of the foot. The appendicular long bones were partly or completely visualized in seven children. Well-defined nodular lesions were present in the metaphysis in seven, in the epiphysis in four, and in the diaphysis in four. Coexisting osteonecrosis was present in three of the eight patients (38%). A nondisplaced pathologic fracture was present in one of the eight patients (Fig. 2). No extramedullary soft-tissue masses were seen. Biopsy proof of relapse was made by directed bone biopsy of marrow signal alterations in two patients and by blind iliac marrow biopsy in six patients. The two patients who underwent directed bone biopsy had had blind iliac marrow biopsy performed initially, which was negative in both cases (Figs. 2 and 3).
A 19-year-old girl with ALL relapse. a Coronal proton density fat-saturated image (PD FS) of the right knee demonstrates evidence of epiphyseal osteonecrosis. In addition, there are multiple, well-defined nodular masses present (arrows). b Coronal PD FS of the pelvis demonstrates similar well-defined nodular masses in the pelvis bone marrow
A 9-year-old boy with ALL relapse. Coronal T1-W image demonstrates well-defined nodular masses in the right superior acetabulum (arrow) and left intertrochanteric femur (arrowhead). There is internal high-signal intensity in the left femoral lesion, and this was consistent with blood products related to pathological fracture (not shown). The right acetabular lesion was biopsied and the pathology was indicative of ALL relapse
Patients in remission
Of the 29 control patients in remission, 5 (17%) had a completely normal marrow pattern. In nine (31%) the marrow had a nodular appearance and the nodules were multiple with poorly defined margins (Fig. 4), unlike the well-defined appearance in the patients with relapse. Three of these nine children demonstrated ill-defined nodules in the small bones of the proximal foot. Among the nine patients with the long tubular bones partly or completely imaged, ill-defined nodular lesions were present in the metaphysis in three, in the epiphysis in six, and in the diaphysis in one. Among the six patients with pelvic imaging, no ill-defined nodules were seen in the pelvis. Coexisting stress reaction/fracture and osteonecrosis were present in 9 patients (31%) and 14 patients (48%), respectively.
An 18-year-old girl with ALL in clinical remission, initially thought to have relapse based on MRI. a, b Coronal T1-W (a) and coronal STIR (b) images demonstrate small, multiple, ill-defined nodular lesions in the metaphyses bilaterally involving the distal femurs and proximal tibias. This was thought to represent relapse based on the initial MRI report. There was no evidence of relapse clinically (1 year of follow-up) and this patient was being followed closely off therapy
On review of the radiology reports at initial interpretation, the correct diagnosis of leukemic relapse had been made prospectively in seven of eight children (88%). The patient with the false-negative finding had multiple, well-defined nodules coexisting with multiple foci of osteonecrosis (Fig. 5), perhaps explaining the false-negative initial interpretation. On review of the radiology reports, the correct diagnosis of no relapse was made prospectively in 26 of 29 patients (90%). Relapse was diagnosed in three patients who had a nodular pattern on MR images (Fig. 4). Although the initial diagnosis was false-positive, the nodular lesions in these three patients had indistinct margins, and they did not have relapse based on clinical and pathological follow-up.
A 7-year-old boy with ALL relapse, initially thought to have multiple foci of developing osteonecrosis. Sagittal STIR image shows multiple, well-defined masses in the distal tibia metaphysis and cuneiform (arrowheads). There is also a focus of epiphyseal osteonecrosis involving the distal tibia (arrow). At the time of the examination, this was felt to represent multiple areas of developing osteonecrosis. The patient was diagnosed with leukemic relapse shortly after this examination
Discussion
Leukemic relapse most commonly occurs in the marrow [3], and timely and accurate diagnosis is important both to reinstitute chemotherapy and to provide the family and child with accurate prognostic information. Unlike the published appearance at initial presentation, we found that marrow changes in all our patients with biopsy-proven relapse had a nodular pattern with well-defined margins.
Interpreting musculoskeletal MR images in leukemia patients in remission is challenging because the marrow pattern is usually not completely normal. The osseous structures in leukemic patients in remission are weakened and predisposed to osteonecrosis and stress injury from prior chemotherapy, radiation, and the disease process itself [4]. Sometimes, when the marrow alterations are small, it may be difficult to determine whether the area of signal alteration represents a developing stress injury, osteonecrosis, or leukemic relapse.
We found that the most important factor differentiating a malignant from a nonneoplastic cause of a nodular marrow pattern is the appearance of its margins. Well-defined margins indicated a neoplastic process. Ill-defined margins indicated a nonneoplastic process and did not herald a relapse event. One control patient had a disconcerting marrow pattern because of the focal distribution of nodules (Fig. 4), but the correct diagnosis could have been made by identifying the ill-defined margins of the individual nodules. Similarly, the correct diagnosis could have been made for the one prospectively false-negative diagnosis in our study group (Fig. 5) by identifying the well-defined margins of the nodular marrow replacement pattern, and distinguishing these from coexisting osteonecrosis affecting other bones of the foot.
A possible explanation of the nodular replacement pattern in leukemic relapse is that, because of stricter monitoring of symptoms, these patients might be undergoing MRI during the very early stages of hematogenous marrow seeding by tumor cells. There was a random distribution of nodules throughout flat, small, and tubular bones similar to the pattern that may be seen in diffuse metastatic disease. We speculate that eventually the marrow might become completely replaced by tumor and resemble the diffuse marrow replacement pattern typically seen in patients with leukemia at initial presentation.
Our MRI findings of well-defined nodular marrow replacement in leukemic relapse are similar to those described in adult case reports of leukemic relapse [8, 10]. Nodular marrow replacement in the pelvis seen in five of our patients with relapse has not been reported in the pediatric or adult literature to our knowledge. Our observations differ from those in the largest series that we are aware of in children. In the series of Benz-Bohm et al. [9], which included four patients with relapse, two different patterns of marrow replacement were seen: two children had a “diffuse inhomogeneous pattern” and two children had a “patchy pattern.” The single image in that report of a patient with relapse shows nodular lesions in the metaphyses and epiphyses about the knee with ill-defined margins. The differences in our observations and descriptions are most likely a result of improvements in MRI techniques since the study of Benz-Bohm et al. [9] in 1990.
Based on our small patient series, clinical, marrow biopsy, and laboratory work-up for relapse should be performed when well-defined nodular replacement is seen in patients with a history of ALL. Patients with an unrevealing blind iliac marrow biopsy or laboratory work-up should undergo directed lesional biopsy. However, patients with ill-defined nodules and no evidence of relapse on clinical and laboratory work-up should be clinically followed.
The limitations of this study include its retrospective nature, the relatively small sample size of eight patients, and the fact that the imaging features of patients in remission were evaluated by one reviewer, while the patients with leukemic relapse were evaluated by two reviewers. A double review was considered necessary since our major objective was to describe the imaging features of leukemic relapse. Although the appendicular regions imaged in the various patients were not identical, characterization of the margin of individual nodules in the marrow remains the most important factor in the differentiation of benign and malignant lesions.
Conclusion
All patients with ALL relapse demonstrated on MRI showed well-defined nodular lesions in the marrow that could be differentiated from marrow alterations in patients in remission. Other considerations to explain the patient’s symptoms, including coexisting osteonecrosis or stress injury, should be entered into the differential diagnosis when the margins of a nodular marrow replacement process are ill-defined.
References
Pui CH, Evans WE (2006) Treatment of acute lymphoblastic leukemia. N Engl J Med 354:166–178
Chan KW (2002) Acute lymphoblastic leukemia. Curr Probl Pediatr Adolesc Health Care 32:40–49
Gaynon PS, Qu RP, Chappell RJ et al (1998) Survival after relapse in childhood acute lymphoblastic leukemia: impact of site and time to first relapse – the Children's Cancer Group experience. Cancer 82:1387–1395
Strauss AJ, Su JT, Dalton VM et al (2001) Bony morbidity in children treated for acute lymphoblastic leukemia. J Clin Oncol 19:3066–3072
Ruzal-Shapiro C, Berdon WE, Cohen MD et al (1991) MR imaging of diffuse bone marrow replacement in pediatric patients with cancer. Radiology 181:587–589
Moore SG, Gooding CA, Brasch RC et al (1986) Bone marrow in children with acute lymphocytic leukemia: MR relaxation times. Radiology 160:237–240
Bohndorf K, Benz-Bohm G, Gross-Fengels W et al (1990) MRI of the knee region in leukemic children. Part I. Initial pattern in patients with untreated disease. Pediatr Radiol 20:179–183
Endo T, Sato N, Koizumi K et al (2004) Localized relapse in bone marrow of extremities after allogeneic stem cell transplantation for acute lymphoblastic leukemia. Am J Hematol 76:279–282
Benz-Bohm G, Gross-Fengels W, Bohndorf K et al (1990) MRI of the knee region in leukemic children. Part II. Follow up: responder, non-responder, relapse. Pediatr Radiol 20:272–276
Aydogdu I, Erkurt AM, Kaya E et al (2005) Bone relapse in a patient with acute lymphoblastic leukaemia. Br J Haematol 129:163
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kan, J.H., Hernanz-Schulman, M., Frangoul, H.A. et al. MRI diagnosis of bone marrow relapse in children with ALL. Pediatr Radiol 38, 76–81 (2008). https://doi.org/10.1007/s00247-007-0653-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-007-0653-4