Abstract
Background
Multidetector CT (MDCT) seems to be a promising tool for detection of neonatal coronary arteries, but whether the ECG-gated or non-ECG-gated technique should be used has not been established.
Objective
To compare the detection rate and image quality of neonatal coronary arteries on MDCT using ECG-gated and non-ECG-gated techniques.
Materials and methods
Twelve neonates with complex congenital heart disease were included. The CT scan was acquired using an ECG-gated technique, and the most quiescent phase of the RR interval was selected to represent the ECG-gated images. The raw data were then reconstructed without the ECG signal to obtain non-ECG-gated images. The detection rate and image quality of nine coronary artery segments in the two sets of images were then compared. A two-tailed paired t test was used with P values <0.05 considered as statistically significant.
Results
In all coronary segments the ECG-gated technique had a better detection rate and produced images of better quality. The difference between the two techniques ranged from 25% in the left main coronary artery to 100% in the distal right coronary artery.
Conclusion
For neonates referred for MDCT, if evaluation of coronary artery anatomy is important for the clinical management or surgical planning, the ECG-gated technique should be used because it can reliably detect the coronary arteries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In neonates with complex congenital heart disease, such as tetralogy of Fallot or D-loop transposition of the great arteries, evaluation of coronary artery anatomy is very important [1–3] because coronary anomalies make early total corrective surgery very difficult [4–9], if not impossible. Furthermore, coronary artery anomalies have proved to be an important negative postoperative prognostic factor [9]. Not knowing the presence of a coronary anomaly and incautiously injuring the neonatal coronary arteries could lead to perioperative mortality because vessels of diameter <1 mm are extremely difficult or impossible to repair. Thus, in some institutions that are unfamiliar with coronary reimplantation techniques, a coronary anomaly is considered a contraindication to early corrective surgery. Traditionally, evaluation of neonatal complex congenital heart disease has included echocardiography (ECHO) and cardiac catheterization. However, detection of coronary arteries by ECHO is limited by the acoustic window and spatial resolution [1, 3, 10], and cardiac catheterization is an invasive procedure with a potential procedure-related death rate of around 0.1–1% [11, 12]. Thus, a reliable noninvasive examination for neonatal coronary artery visualization is needed.
Recently, multidetector row CT (MDCT) has been used more frequently in congenital heart disease [13–23]. Although there are many reports of coronary anomaly detection [19–22], most focus on older children or adults. Only the study by Goo et al. [19] included neonates. They used non-ECG-gated CT to visualize the coronary arteries in children aged from 1 day to 15 years. They reported a detection rate of the proximal coronary arteries of 81.7%, but the detection rate was correlated with the patient’s age. In neonates the detection rate usually varies widely.
In our clinical experience, we have not found non-ECG-gated MDCT to be reliable in terms of either diagnostic confidence or image quality for coronary artery detection. Although we expected it to be reliable as a preoperative planning reference, results were disappointing in our early cases. Thus, we decided to use ECG-gated MDCT for simultaneous coronary artery detection in the evaluation of the anatomy of neonatal complex congenital heart disease. Because there are no reports of studies that have compared ECG-gated and non-ECG-gated MDCT for detection of the coronary arteries in neonates, we decided to conduct this study. We investigated (1) the ability of ECG-gated MDCT to detect the coronary arteries in neonates and the quality of the images produced, and (2) whether ECG-gated MDCT has a better detection rate and produces images of better quality than non-ECG-gated MDCT.
Materials and methods
Patients
From February to November 2006, all neonates (<30 days old) with complex congenital heart disease (defined as more than one cardiovascular anomaly) referred for MDCT in a 1,500-bed tertiary referral centre were included in this study. The indication for referral was the agreement of two independent paediatric cardiologists (each with more than 8 years’ experience) that ECHO could not completely evaluate the neonate’s cardiovascular anatomy because of, for example, the extent of coarctation of the aorta, coronary artery anatomy, the condition of the pulmonary vein, a limited acoustic window, and the extent of peripheral pulmonary stenosis [2, 24]. The exclusion criteria were: heart rate >140 bpm (exceeding the scanner limit for ECG gating), impaired renal function (serum creatinine level >1.4 mg/dl) and parental refusal to allow the neonate to undergo MDCT. The demographics of the neonates, including gender, age, and body weight, were recorded.
Because the study involved image analysis, all procedures were performed within the confines of clinical practice. The potential risk of radiation exposure and contrast medium injection were explained to all parents by a cardiac radiologist. Written informed consent had to be signed before the CT scan was acquired. The clinical management and decisions and the patient’s privacy and rights were not compromised. Thus, this study was conducted under the waiver of authorization of the institutional review board of our hospital.
Cardiac MDCT protocol
Feeding was prohibited for 1 h before scanning. A 24-gauge intravenous catheter was placed in the dorsal aspect of the right hand. The CT room lights were dimmed. Radiolucent monitoring electrodes (Red Dot 2570; 3M Health Care, Ontario, Canada) and socket lead wires (radiolucent ECG lead sets M1649A; Philips Medical Systems, Andover, Mass.) were used for acquiring ECG signals. These electrodes and wires are made of carbon to ensure good conductivity and minimize beam-hardening artefacts. For the three patients with an endotracheal tube, ventilator support using intermittent mandatory mode and 100% oxygen were used during scanning. Ventilator settings included a respiratory rate of 30 per minute and an inspiratory time of 0.5 s. For the other patients without an endotracheal tube, an oxygen cannula was used. Intravenous injection of 0.15 ml/kg midazolam (Dormicum; Roche, Vienna, Austria) was used for sedation after the pulse oximeter showed oxygen saturation >80%. No additional respiratory control, or oral or intravenous beta-blocker was administered.
The scan was undertaken using a 40-detector-row CT scanner (Brilliance 40; Philips, Best, the Netherlands). Protocol details were: 40×0.625-mm collimation, 80 kVp tube voltage, 150 mA tube current, rotation time 0.42 s and pitch 0.2 with retrospective ECG gating. For heart rates >95 bpm a four-segment reconstruction strategy was used to improve temporal resolution. The contrast material (Omnipaque 350; Amersham, Cork, Republic of Ireland) was diluted to a contrast medium/saline ratio of 2:1. The diluted contrast medium was injected at a volume of 3 ml per kg body weight. The saline chaser volume was 0.3 times the diluted contrast volume + 5 ml. Saline (5 ml) was added to compensate for the volume of the connection tube. Flow rate was determined by the ‘contrast-covering time’ concept (http://tinyurl.com/rymuw) [23] and was calculated using the following formula:
The scan was from the upper margin of the shoulder to the lower end of the liver. Bolus tracking was used for synchronization between contrast medium injection and scanning, with the region of interest in the descending aorta at the level of the carina, a point that is always easily identified on the nonenhanced locator image. After the enhancement reached 150 HU, a 5-s postthreshold delay was applied before the scan. A paediatrician continuously monitored the oxygen saturation and blood pressure during the scan to ensure patient safety.
Ten equally spaced phases of images were reconstructed from 0% to 90% RR interval with a slice thickness/index of 0.67/0.33 mm. Furthermore, for nongated images the ECG signals were removed from the raw data and a new set of images was reconstructed on the CT console (offline reconstruction, Brilliance 40; Philips, Best, The Netherlands). This set of images represented the nongated spiral CT images. The image thickness/index was also set at 0.66/0.33 mm.
A senior CT technologist with more than 10 years’ experience performed all the scans. The diluted contrast medium volume, saline chaser volume, flow rate, time to threshold from injection, dose–length product, scan time, mean heart rate during scan, and average standard deviation of heart rate during scan of each patient were also recorded.
Image evaluation
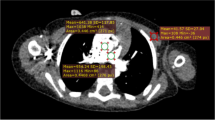
Two cardiac radiologists who had reviewed more than 1,400 adult and paediatric cardiac MDCT scans and were blinded to the image techniques performed, collected the following measurements in consensus. All the reconstructed images were loaded into the CT work station (Cardiac Review, Extended Brilliance Workspace; Philips, Best, The Netherlands). The most quiescent phase was then chosen and loaded into the viewer (Cardiac Viewer, Extended Brilliance Workspace) for interpretation. Techniques such as multiplanar reformation and maximum-intensity projection were freely used to visualize the nine coronary artery segments—left main coronary artery, proximal, middle and distal left anterior descending coronary arteries, proximal and distal circumflex arteries, and proximal, middle and distal right coronary arteries [19]. Because the side branches such as diagonal and marginal branches are usually not identified in neonates, the definition of proximal, middle and distal coronary arteries was made by the interpreting cardiac radiologist according to length and location. In the nine segments, four segments, including the left main, proximal left anterior descending, proximal circumflex and proximal right coronary arteries, were defined as proximal coronary segments. The other five were considered as distal coronary segments. A five-grade scoring system was used in the image quality evaluation:
-
Grade 5:
clear visualization without any motion artefact
-
Grade 4:
mild motion artefact, but still with high diagnostic confidence
-
Grade 3:
obvious blurring, moderate diagnostic confidence
-
Grade 2:
identified but equivocal, may simulate other structures
-
Grade 1:
severe motion artefact, no coronary segment can be visualized
Grades 1 and 2 were considered as “not detected”. Grades 3, 4 and 5 were considered as “detected”. The same procedures as above were used in the evaluation of nongated images.
Evaluation of detection rate and image quality
The detection rates of all, proximal, distal and individual coronary segments were calculated for both gated and nongated images. The quality scores of individual coronary segments and average quality of all, proximal and distal coronary artery segments were also calculated to represent the image quality.
Statistical analysis
A two-tailed paired t test was used to compare the image quality between the gated and non-gated images. P values <0.05 were considered statistically significant.
Results
This study initially included 15 neonates, but 3 had a heart rate >140 bpm, even after sedation, and were, therefore, excluded. No parents refused MDCT and no neonates had renal impairment. After the exclusions, 12 neonates remained in the study. Four had aortic coarctation, two had tetralogy of Fallot, two had a double-outlet right ventricle, one had an interrupted aortic arch, one had D-loop transposition of the great arteries, one had hypoplastic left heart syndrome and one had pulmonary atresia with the main pulmonary artery arising from the conus branch of the right coronary artery (Figs. 1, 2, 3 and 4; Electronic supplementary material, animation 1). The demographic data are shown in Table 1.
Demonstration of the 5-grade image quality scoring system. a Grade 5: clear delineation of the coronary segment without any visualized motion artefact or discontinuity (arrow). This grade provides excellent diagnostic confidence. b Grade 4: clear delineation of the coronary segment with minimal motion artefact (arrowhead) and attenuation inhomogeneity (arrow). This grade provides high diagnostic confidence. In this case, the central pulmonary artery is arising from the conus branch (dashed arrow) of the right coronary artery. c Grade 3: visualization of the coronary segment with marginal blurring motion artefact, but the coronary segment can still be confidently identified (arrow). Grades 5–3 are considered diagnostic. d Grade 2: marked blurring of the coronary segment, which makes identification difficult (arrow). With this grade, the interobserver agreement is considered to be low and interpretation becomes more subjective. The diagnostic confidence is also low. Thus, this kind of image is considered to be nondiagnostic. e Grade 1: severe motion artefact, which makes identification of the coronary segment impossible (arrow). Grade 1 images are not diagnostic. (Ao aorta)
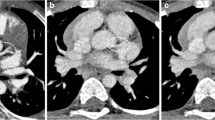
ECG-gated image quality. a Multiplanar reformatted image shows the left main coronary artery (arrow, grade 5) and proximal left anterior descending artery (arrowheads, grade 4). Both segments are diagnostic. b Multiplanar reformatted image shows the proximal (arrow, grade 4) and distal circumflex artery (arrowhead, grade 4). Both segments are diagnostic. c Multiplanar reformatted image shows the proximal right coronary artery (arrow, grade 4). The segment is also diagnostic. Also note the large conus branch (dashed arrow) anastomosing with the central pulmonary artery (CPA). (Ao aorta)
Non-ECG-gated image quality. The same patient as in Fig. 2. The images were reformatted in the same plane. a The same plane as in Fig. 2a shows no left main coronary artery and the proximal left anterior descending artery can be identified (grade 1). Distally, a faint density is noted (dashed arrow), probably the middle left anterior descending artery (grade 2). The plane is exactly the same as in Fig. 2a, but due to the vigorous motion, the pulmonary artery is visualized in this level. Scrolling up or down, the left main and proximal left anterior descending arteries are not found. b The same plane as in Fig. 2b shows no proximal or distal circumflex arteries due to motion artefact. c The same plane as in Fig. 2c shows that the proximal right coronary artery cannot be identified. Even with retrospective examination, only a faint density is noted in the location (arrow). In this patient, the anatomy of the right coronary artery is important since the final diagnosis was pulmonary artery arising from the conus branch of the right coronary artery (dashed arrow). If not recognized, the insertion would be considered in the ascending aorta. The surgeon may have begun corrective surgery but found the case inoperable due to possible disruption of the right coronary artery during manipulation. (Ao aorta, CPA central pulmonary artery, RPA right pulmonary artery)
Annotation image for the animation of cardiac motion. The animation is provided online. The heart size is only about 5 cm in the long axis. The circumflex artery (arrowhead), right coronary artery (arrow) and atrial septal defect (dashed arrow) are all clearly visualized and annotated. (RA right atrium, RV right ventricle, LA left atrium, LV left ventricle)
Nine coronary segments could potentially be identified in every patient, making a total of 108 segments, of which 48 were proximal and 60 were distal coronary segments. The detection rates are shown in Table 2 and the image qualities are shown in Table 3. In all coronary segments, ECG-gated images had better detection rate and quality. The smallest difference between the techniques was in the detection of the left main and middle left anterior descending coronary arteries: 25% more arteries were detected in the ECG-gated images than in the nongated images. The largest difference between the techniques was in the detection of the distal right coronary artery: 100% more arteries were detected in the ECG-gated images than in the nongated images.
Discussion
In the imaging of the coronary arteries in neonates, ECG-gated MDCT detected 100% of the proximal coronary artery segments and 73.3% of the distal coronary artery segments. ECG-gated MDCT detected almost 60% more proximal and distal coronary segments than non-ECG-gated MDCT. Furthermore, ECG-gated MDCT had a better detection rate and the images were of better quality in all coronary artery segments. We therefore consider that in a neonate referred for cardiac CT of the coronary anatomy either to assist in diagnosis (for example, of an anomalous left coronary artery from the pulmonary artery or complex pulmonary atresia with a pulmonary artery from the coronary artery) or for surgical planning (for example, D-loop transposition of the great arteries in an arterial switch operation or total correction of tetralogy of Fallot) the ECG-gated technique should be used. The nongated technique can provide valuable information about chamber anatomy, but it is not reliable for coronary artery detection.
Goo et al. [19] have reported that detection of proximal segments of the coronary artery in patients with congenital heart disease can reach 81.7% using the non-ECG-gated technique. However, the age range of their study population was wide, from 1 day to 15 years, and further analysis also demonstrated that detection of the coronary arteries was better in older children. Moreover, the detection rate of the coronary arteries in neonates varied widely and thus was not reliable. In our study we focused exclusively on neonates to obtain more specific results. Furthermore, we used stricter criteria in defining the term “detected” because we did not believe that images with obvious blurring, such as grade 2 (of 5) in our study and visual grade 2 (of 3) in the study by Goo et al. [19] could provide enough diagnostic confidence for surgical planning. In their study, visual grade 2 (of 3) was considered “detected”, which is different from our definition of grade 2. This is one reason why the non-ECG-gated technique had a lower detection rate in our study than it did in theirs.
In our institution, diagnostic neonatal cardiac catheterization is rarely performed preoperatively due to high diagnostic confidence in MDCT for demonstrating both chamber and coronary artery anatomy. The ECG-gated technique has about twice the radiation dose of the non-gated technique (91.2 mGy*cm in this study vs. 47.1 mGy*cm for the nongated technique in the study by Lee et al. [23]). Although the gated pitch is one-third of the nongated pitch, the radiation dose from the gated technique is far less than three times that from the nongated technique. This is because the spiral scan has an inherent baseline dose caused by the exposure at the start and end of the scan. Considering the risk of diagnostic cardiac catheterization, the ECG-gated technique is still preferred.
Some radiologists might straightforwardly think that since breath-holding is mandatory in performing CT coronary angiography in adults, gated cardiac CT in free-breathing neonates would probably not generate good quality images. However, from our 400-case experience of paediatric cardiac CT, the gated technique does provide a great opportunity to demonstrate the whole coronary artery tree in free-breathing patients below 2 years of age. The reason for this is not known and there is so far no literature exploring this topic. The assumed reason is that the respiratory motion of neonates is relatively small compared to that in older children, and is also compensated by a faster respiratory rate. This smaller motion might sometimes truncate the coronary arteries on CT, but most segments can still be clearly seen. Furthermore, in neonates, we need coronary artery ‘detection’; but in adults, we need to be able to determine the extent of coronary artery stenosis. Thus, in neonates we can tolerate more respiratory motion in gated CT, but in children beyond 2 years of age, gated cardiac CT mostly fails to show the location of the coronary arteries. We now use the non-gated technique in older children with congenital heart disease if coronary detection is not the main issue.
Since MDCT has the inherent limitation of radiation dose, MRI might be considered an alternative cross-sectional imaging modality to visualize neonatal coronary arteries. Though some leading institutions have had some encouraging early experience, there are still no studies published concerning MRI in neonatal coronary artery detection. Su et al. [25] evaluated the origins of the coronary arteries in a paediatric population using real-time navigator MRI and achieved a 95% detection rate. However, their patients’ ages ranged from 11 days to 21 years (mean 12.6±5.4 years, median 14.3 years), and no images of neonatal coronary arteries are shown in the publication. It is unknown whether MRI could still produce good results when only neonates are evaluated.
There were three limitations to this study. Firstly, we did not scan the same patients with the ECG-gated and non-ECG-gated techniques. Instead, we reconstructed the raw data without the ECG signal to represent the non-ECG-gated technique. The image is actually a nongated spiral scan with a pitch of 0.2, which is different from the pitch usually used of 0.6–1 [19, 23]. Although the spatial resolution and functional width might be pitch-independent with modern technology, the temporal resolution actually differs since the scan time is prolonged and the images are reconstructed using data from multiple rotations. Considering that neonates are very radiation sensitive, scanning a neonate twice for study purposes is considered unethical and unnecessary. The second limitation was the small sample size because of the strict indications for neonatal cardiac CT. Only neonates with complex congenital heart disease who could not be completely evaluated by ECHO were included in the study. In comparing the gated and nongated images of the same patient a two-tailed paired t test has great statistical power, which could partly compensate for the small sample. The significant difference in the comparison result was also enough to differentiate the two techniques. Finally, we did not use the ECG-pulsing technique because the radiation dose saved by this technique is inversely correlated with the patient’s heart rate. For the high heart rates seen in neonates, ECG pulsing cannot save much radiation dose, but could have a potentially negative effect on image quality.
Conclusion
Our study shows that ECG-gated MDCT is very accurate for the detection of the coronary arteries in neonates and is significantly better than the nongated technique. For neonates referred for MDCT, if evaluation of coronary artery anatomy is important to clinical management or surgical planning, the ECG-gated technique should be used because it can reliably detect the coronary arteries.
References
Tworetzky W, McElhinney DB, Brook MM et al (1999) Echocardiographic diagnosis alone for the complete repair of major congenital heart defects. J Am Coll Cardiol 33:228–233
Soongswang J, Nana A, Laohaprasitiporn D et al (2000) Limitation of transthoracic echocardiography in the diagnosis of congenital heart diseases. J Med Assoc Thai 83(Suppl 2):S111–S117
Marek J, Skovranek J, Hucin B et al (1995) Seven-year experience of noninvasive preoperative diagnostics in children with congenital heart defects: comprehensive analysis of 2,788 consecutive patients. Cardiology 86:488–495
Ruzmetov M, Jimenez MA, Pruitt A et al (2005) Repair of tetralogy of Fallot with anomalous coronary arteries coursing across the obstructed right ventricular outflow tract. Pediatr Cardiol 26:537–542
Chang YH, Sung SC, Lee HD et al (2005) Coronary reimplantation after neoaortic reconstruction can yield better result in arterial switch operation: comparison with open trap door technique. Ann Thorac Surg 80:1634–1640
Sung SC, Chang YH, Lee HD et al (2005) Arterial switch operation for transposition of the great arteries with coronary arteries from a single aortic sinus. Ann Thorac Surg 80:636–641
Schreiber C, Horer J, Lange R (2005) Modification of the arterial switch procedure in the presence of a rare coronary arterial pattern. Cardiol Young 15:82–84
Cetin G, Tireli E, Ozkara A (2004) Arterial switch operations for single coronary artery ostium or intramural coronary artery. Circ J 68:1179–1183
Kolcz J, Januszewska K, Mroczek T et al (2004) Anatomical correction of complex forms of transposition of the great arteries in neonates. Scand Cardiovasc J 38:164–171
Gremmels DB, Tacy TA, Brook MM et al (2004) Accuracy of coronary artery anatomy using two-dimensional echocardiography in d-transposition of great arteries using a two-reviewer method. J Am Soc Echocardiogr 17:454–460
Simpson JM, Moore P, Teitel DF (2001) Cardiac catheterization of low birth weight infants. Am J Cardiol 87:1372–1377
Vitiello R, McCrindle BW, Nykanen D et al (1998) Complications associated with pediatric cardiac catheterization. J Am Coll Cardiol 32:1433–1440
Cinar A, Haliloglu M, Karagoz T et al (2004) Interrupted aortic arch in a neonate: multidetector CT diagnosis. Pediatr Radiol 34:901–903
Frush DP, Herlong JR (2005) Pediatric thoracic CT angiography. Pediatr Radiol 35:11–25
Bean MJ, Pannu H, Fishman EK (2005) Three-dimensional computed tomographic imaging of complex congenital cardiovascular abnormalities. J Comput Assist Tomogr 29:721–724
Goo HW, Park IS, Ko JK et al (2003) CT of congenital heart disease: normal anatomy and typical pathologic conditions. Radiographics 23 (Spec No):S147–S165
Gilkeson RC, Ciancibello L, Zahka K (2003) Multidetector CT evaluation of congenital heart disease in pediatric and adult patients. AJR 180:973–980
Goo HW, Park IS, Ko JK et al (2005) Computed tomography for the diagnosis of congenital heart disease in pediatric and adult patients. Int J Cardiovasc Imaging 21:347–365
Goo HW, Park IS, Ko JK et al (2005) Visibility of the origin and proximal course of coronary arteries on non-ECG-gated heart CT in patients with congenital heart disease. Pediatr Radiol 35:792–798
Schmitt R, Froehner S, Brunn J et al (2005) Congenital anomalies of the coronary arteries: imaging with contrast-enhanced, multidetector computed tomography. Eur Radiol 15:1110–1121
Dogan OF, Guvener M, Demircin M et al (2006) Diagnosis of a coronary artery anomaly by 16-channel computed tomography coronary angiography in an infant. Pediatr Cardiol 27:658–659
Coche E, Muller P, Gerber B (2006) Anomalous origin of the left main coronary artery from the main pulmonary artery (ALCAPA) illustrated before and after surgical correction on ECG-gated 40-slice computed tomography. Heart 92:1193
Lee T, Tsai IC, Fu YC et al (2006) Using multidetector-row CT in neonates with complex congenital heart disease to replace diagnostic cardiac catheterization for anatomical investigation: initial experiences in technical and clinical feasibility. Pediatr Radiol 36:1273–1282
Gutgesell HP, Huhta JC, Latson LA et al (1985) Accuracy of two-dimensional echocardiography in the diagnosis of congenital heart disease. Am J Cardiol 55:514–518
Su JT, Chung T, Muthupillai R et al (2005) Usefulness of real-time navigator magnetic resonance imaging for evaluating coronary artery origins in pediatric patients. Am J Cardiol 95:679–682
Acknowledgements
We would like to express our appreciation to Mr. Larry Chia-Hon Chen (Philips Medical Systems, Taiwan) and Mr. Leon Wei-Chun Lee (Unison Tek Co. Ltd., Taiwan) for their assistance in improving the quality of neonatal cardiac CT.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tsai, IC., Lee, T., Chen, MC. et al. Visualization of neonatal coronary arteries on multidetector row CT: ECG-gated versus non-ECG-gated technique. Pediatr Radiol 37, 818–825 (2007). https://doi.org/10.1007/s00247-007-0512-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-007-0512-3