Abstract
Background
Nontuberculous mycobacteria (NTM) are a common cause of chronic cervicofacial lymphadenitis in young children. The differential diagnosis includes other infections, lymphoepithelial cysts and malignancies.
Objective
To assess the sonographic findings of NTM cervicofacial lymphadenitis in children.
Materials and methods
We analysed the sonograms of cervicofacial lymph nodes of 145 children with microbiologically proven NTM lymphadenitis.
Results
The size of the involved lymph nodes ranged from 1.9 cm to 4.4 cm. Most of the NTM patients (85%) presented in a stage of lymph node fluctuation with violaceous skin discoloration. On sonography, marked decreased echogenicity was seen in all cases. In 133 of the patients (92%) liquefaction with intranodal cystic necrosis, nodal matting and adjacent soft-tissue oedema were present. 66 children received antibiotic treatment, and the other children underwent surgical excision of the involved lymph nodes. In 69% of the patients successfully treated with antibiotics, multiple intranodal calcifications were present on sonography after 1 year.
Conclusions
Sonographic findings can provide additional diagnostic clues for NTM lymphadenitis in childhood. A marked decrease of echogenicity in the early stages, with intranodal liquefaction in the advanced stages, are universal features, albeit not entirely specific. Multiple intranodal calcifications are rather characteristic of end-stage mycobacterial infection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Nontuberculous mycobacterial (NTM) lymphadenitis is a common cause of chronic cervicofacial lymphadenitis in immunocompetent children. The disease manifests itself in young children between the ages of 1 and 5 years, usually without generalized symptoms. Unilaterally enlarged solitary or clustered nodal masses occur in the submandibular or preauricular areas, and the nodes suppurate and form a chronic sinus tract [1] The differential diagnosis consists of other infections, e.g. Bartonella henselae lymphadenitis, lymphoepithelial cysts and malignancies. Following history and physical examination, sonographic evaluation of the head and the neck is one of the first investigations performed in such patients. In adult patients sonography may help to differentiate malignant from benign lymphadenopathy [2], and it provides information on the number, size, site, shape, borders, matting, adjacent soft-tissue oedema, and internal architecture of cervicofacial lymph nodes [3]. On grey-scale sonography, normal and reactive nodes tend to be hypoechoic and oval (short-axis to long-axis ratio, S/L, <0.5), except for submandibular and parotid nodes, which are usually round (S/L ≥0.5), and they have an echogenic hilus [3]. Malignant lymph nodes on grey-scale sonography and metastatic nodes are usually hypoechoic, round, and without an echogenic hilus. Coagulation necrosis, which appears as a demarcated echogenic focus, may be found in metastatic nodes while eccentric cortical hypertrophy is a useful sign to indicate focal tumour infiltration. Lymph nodes with cystic necrosis are suggestive of malignancy, and intranodal cystic necrosis is common in metastatic nodes from squamous cell carcinomas.
Ultrasonographic findings in a large series of children with NTM cervicofacial lymphadenitis have not previously been reported. During the course of the CHIMED (surgery versus medication) study, a randomized, prospective, multicentre trial on the optimal treatment of NTM cervicofacial lymphadenitis in children, we performed ultrasonography in 145 children. We here describe the findings in these patients with microbiologically proven NTM infection.
Materials and methods
Patients
Children with chronic cervicofacial lymphadenitis were included in the CHIMED trial, a nationwide study in the Netherlands on the optimal treatment of NTM cervicofacial lymphadenitis in children. Patients were referred by paediatricians, otolaryngologists, oral-maxillofacial surgeons and general practitioners from all over the country to the principal investigator (J.L.). The diagnosis of NTM lymphadenitis was confirmed in all patients by polymerase chain reaction (PCR) or culture, or both. The diagnostic procedures and patient characteristics have been described previously [4–6]. The Medical Ethics Committee of the Academic Medical Center of the University of Amsterdam approved the study.
Methods
Ultrasonographic examinations were performed with a Siemens Sonoline ultrasound scanner (Siemens Medical Solutions, Munich, Germany) and a 7.5–13-MHz linear-array transducer. All examinations were performed in the paediatric radiology department. Two paediatric radiologists (A.S. and R.R.) performed or supervised the ultrasound studies; only the regions of the head and neck were screened. Lymph nodes were classified according to their location in the head and neck regions. This method is similar to the one described by Hajek et al. [7], who subdivided the head and neck into eight regions. The lymph nodes shown by grey-scale sonography were analysed according to established sonographic criteria: distribution, size, shape, presence of an echogenic hilum, internal architecture, homogeneity, echogenicity, sharpness of borders, posterior sound enhancement, ancillary features such as intranodal cystic necrosis and presentation of surrounding soft tissues (e.g. thickening or oedema of the surrounding soft tissues). Lymph node shape was assessed by measuring the largest and smallest diameter on the same scan and by calculating the short-axis to long-axis (S/L) ratio. An S/L ratio of less than 0.5 indicates an elongated or elliptical node, whereas an S/L ratio of 0.5 or more indicates an oval or spherical node [8]. An abscess was suspected in the presence of ultrasonic posterior sound enhancement, cystic necrosis, poorly defined borders, and heterogeneous echo texture. Fine-needle aspiration was performed in all children to demonstrate the presence of pus and to obtain material for PCR and culture. All lymph nodes in the head and neck with a diameter more than 10 mm were regarded as infected nodes [3].
Statistical analysis
Descriptive statistics were used to characterize the patients and the sonographic data.
Results
Patients
A total of 145 patients had confirmed NTM cervicofacial lymphadenitis diagnosed either by positive culture only (n=32), PCR only (n=30) or both (n=83). Of the 145 infections, 101 (69.6%) were caused by Mycobacterium avium, 35 (24.1%) by M. haemophilum, 3 by M. malmoense, 2 by M. kansasii, 1 by M. chelonei, 1 by M. intracellulare and 1 by M. fortuitum. One NTM species was non-typable.
The age of the patients ranged from 9 months to 138 months, with a median age of 48 months. Of the 145 children, 73 were boys and 72 were girls. The mean duration of lymph node swelling until initial presentation at our clinic was 12.2±7.9 weeks. The children had no systemic symptoms and they were all in good health.
Treatment consisted of surgery or antibiotic treatment. Most children and their parents agreed to participate in a prospective randomized study comparing surgical excision of the affected lymph nodes with antibiotic treatment consisting of clarithromycin and rifabutin for a minimum of 3 months. Details of this study will be reported elsewhere. In total, 66 children received antibiotic treatment consisting of clarithromycin and rifabutin for a minimum period of 3 months, and the other children underwent surgical excision of the involved lymph nodes.
Ultrasound characteristics
In the 145 patients the diseased lymph nodes were detected in the submandibular region in 126 patients (87%), the preauricular/parotid region in 13 patients (9%) and the submental region in 4 patients. Abnormal lymph nodes were found in the supraclavicular region in only one patient and in the occipital region in another patient. Unilateral lymph node involvement was seen in 143 children and there were 2 children with bilateral submandibular involvement. More than one nodal region was involved in 22 patients (15%), which in 3 patients was caused by M. avium and in 19 patients by M. haemophilum infection The ultrasound-measured sizes of the diseased lymph nodes ranged from 1.9 cm to 4.4 cm. The mean diameter of the lymph nodes infected with M. avium was 3.2±0.9 cm and of those infected with M. haemophilum was 2.9±0.8 cm (Student’s t-test, P=0.18).
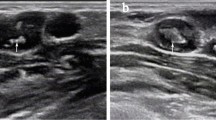
Most of the NTM cervicofacial lymphadenitis patients (85%) presented at the medical centre in a stage clinically characterized by lymph node fluctuation with violaceous skin discoloration (Fig. 1). A minority of the patients (15%) had clinical features of a cervicofacial swelling or nodal mass without abscess formation or skin colour changes. On sonography, all involved lymph nodes were hypoechoic. In 133 of the 145 patients (92%) liquefaction with intranodal cystic necrosis, nodal matting, and adjacent soft-tissue oedema were indications of central necrosis with the presence of pus, which could be confirmed by fine-needle aspiration in all patients. The S/L ratio was <2 in 6 patients (4%) and >2 in 139 patients (96%). Figure 2 shows central lymph node necrosis in a patient without skin discoloration or clinical evidence of abscess formation. Figure 3 shows the surgical specimen of the infected lymph node.
Of the 145 patients, 66 were treated with clarithromycin and rifabutin. A draining fistula was observed during follow-up sonography in 62 of these patients (93%). In 48 patients antibiotic treatment was successful. In 33 of these 48 patients multiple intranodal calcifications were present on the follow-up sonogram after 1 year (Fig. 4).
Discussion
To our knowledge this study is the first comprehensive description of grey-scale sonographic findings in a series of patients with microbiologically proven NTM cervicofacial lymphadenitis. Previous reports are limited to anecdotal cases. Singular or multiple enlarged lymph nodes with marked skin discoloration were seen in 85% of patients at initial presentation. The submandibular region was the most affected lymph node station, and almost all patients had unilateral node involvement. All lymph nodes were hypoechoic, and in the majority of the patients liquefaction with intranodal cystic necrosis, nodal matting, adjacent soft-tissue oedema and pus were present, as an indication of lymph node necrosis. The sonographic lymph node characteristics were not specific for the type of NTM species. Nevertheless, multiple involved lymph node stations were seen in 54% of patients infected with M. haemophilum and in only 3% of those with M. avium infection. Intranodal calcification was seen on the follow-up sonogram after 1 year in 68% of the patients successfully treated with antibiotics.
The clinical manifestations of the patients in our study were in accordance with previous reports from the literature [1], and a strong point of our study was that only patients with a culture- or PCR-proven NTM infection were analysed. The differential diagnosis of the clinical and imaging appearance of NTM cervicofacial lymphadenitis includes tuberculosis, cat-scratch disease and lymphomas. A limitation of our study was that no comparison was made with other infectious causes of chronically enlarged lymph nodes. The grey-scale sonographic features of cervical lymphadenopathy in cat-scratch disease have been described by Ridder et al. [8]. They found hypoechoic echogenicity and normal surrounding tissue in all patients.
A diagnostic delay during NTM infection is common as a result of lack of familiarity of clinicians with this condition [7]. Enlarged lymph nodes can be detected by various imaging modalities including ultrasonography, CT, and MRI [9].
B-mode sonography with ultrasonic frequencies of 5–7.5 MHz has been an integral diagnostic modality in patients with lymphadenopathy, while colour-flow Doppler can display the angioarchitecture of lymph nodes and is a useful addition to B-mode scanning for differentiating benign from malignant cervical lesions in various types of head and neck cancer [10]. The new generation of high-resolution ultrasound platforms with the power-mode feature enables the imaging of perinodular and intranodular small vessel blood flow. An aberrant course of intranodal vessels, focal absence of perfusion and subcapsular vessels are characteristics of malignant nodes, while straight hilar vessels with regular branches are associated with a reactive or inflammatory lymphadenopathy [11].
Several authors consider power Doppler to be superior to colour-coded Doppler sonography in visualizing intranodal flow patterns. The greater ability to visualize the tiny intranodal vessels as well as the better colour persistence and the angle independence are responsible for the diagnostic superiority of power Doppler over colour-coded Doppler sonography [11] Three-dimensional (3D) power Doppler sonography has also been used to classify vascular patterns of cervical lymphadenopathy; however, accurate assessment of vascular patterns might be difficult [12]. The use of ultrasound contrast agent during colour-coded duplex sonography and power Doppler appears to allow a better delineation of hilar and peripheral vascularization in enlarged lymph nodes, but it does not improve the diagnostic accuracy in the evaluation of lymph nodes suspected to be malignant [11]. On colour Doppler, power Doppler, and 3D sonography, normal cervical nodes show hilar vascularity or appear as avascular, and reactive nodes predominantly show hilar vascularity [3]. On spectral sonography normal and reactive nodes usually show low vascular resistance. Inflammation causes vasodilatation, which increases blood flow velocity in reactive lymph nodes.
The presence of an echo complex pattern of irregular hyperechoic small intranodular structures and the presence of an irregular diffuse intranodular blood flow are the best indicators of malignancy [10]. The more rounded lymph nodes with a Solbiati index (SI, ratio of largest to smallest diameter) of <2 corroborate the suspicion of malignancy, while a SI of >2 is highly indicative of benign changes [13]. However, the SI is not a tool allowing a reliable discrimination between malignancy and benignity if used as a single criterion [11]. In NTM infection a marked decrease in echogenicity in the early stages, and intranodal liquefaction, nodal matting and soft-tissue oedema in the progressed stages, are universal features, albeit not entirely specific. In the patient treated non-surgically, intranodal calcification is a common end-stage feature.
CT imaging of NTM lymphadenitis shows dominant peripheral enhancement with a central hypodense mass, associated with relatively little fat stranding, and often accompanied by skin thickening and smaller, anatomically separate, cavitating nodal masses [9, 14]. In MRI images, suppurative granulomatous material is represented by low-density ring-enhancing subcutaneous masses extending from the adenopathy to the skin, while minimal stranding of adjacent subcutaneous fat is seen [9].
Ultrasonography has the advantage that it is widely available and quick, and has a good patient tolerance. Using ultrasonography in NTM cervicofacial lymphadenitis can also play a role in treatment planning, and during therapeutic follow-up. A preferred treatment of NTM cervicofacial lymphadenitis is surgical excision [15–18], which should be performed with the least possible complications. In patients with lymph node necrosis and violaceous skin discoloration many surgeons remove the affected skin. Skin involvement could be detected with sonographic examination in the early stages of the disease. In addition, sonographic assessment of NTM lymphadenitis might provide the physician with information on the number of affected lymph nodes, the contiguity of major vessels, and the status of the affected lymph nodes prior to surgery.
Conclusion
We conclude that detection of central liquefaction or presumed suppuration by early sonographic assessment, and the other characteristics as assessed in this study, could play an important role in early recognition of necrotizing NTM lymphadenitis. Furthermore, it provides supplemental information that may be helpful for initiating early and correct treatment.
References
Wolinsky E (1995) Mycobacterial lymphadenitis in children: a prospective study of 105 nontuberculous cases with long-term follow-up. Clin Infect Dis 20:954–963
Ahuja A, Ying M, Yuen YH, et al (2001) Power Doppler sonography to differentiate tuberculous cervical lymphadenopathy from nasopharyngeal carcinoma. AJNR 22:735–740
Ahuja AT, Ying M (2005) Sonographic evaluation of cervical lymph nodes. AJR 184:1691–1699
Bruijnesteijn van Coppenraet ES, Lindeboom JA, Prins JM, et al (2004) Real-time PCR assay using fine-needle aspirates and tissue biopsy specimens for rapid diagnosis of mycobacterial lymphadenitis in children. J Clin Microbiol 42:2644–2650
Bruijnesteijn van Coppenraet ES, Kuijper EJ, Lindeboom JA, et al (2005) Mycobacterium haemophilum and lymphadenitis in children. Emerg Infect Dis 11:62–68
Lindeboom JA, Prins JM, Bruijnesteijn van Coppenraet ES, et al (2005) Cervicofacial lymphadenitis in children caused by Mycobacterium haemophilum. Clin Infect Dis 41:1569–1575
Hajek PC, Salomonowitz E, Turk R, et al (1986) Lymph nodes of the neck: evaluation with US. Radiology 158:739–742
Ridder GJ, Richter B, Disko U, et al (2001) Gray-scale sonographic evaluation of cervical lymphadenopathy in cat-scratch disease. J Clin Ultrasound 29:140–145
Robson CD, Hazra R, Barnes PD, et al (1999) Nontuberculous mycobacterial infection of the head and neck in immunocompetent children: CT and MR findings. AJNR 20:1829–1835
Görges R, Eising EG, Fotescu D, et al (2003) Diagnostic value of high resolution B-mode and power mode sonography in the follow up of thyroid cancer. Eur J Ultrasound 16:191–206
Schulte-Altedorneburg G, Demharter J, Linne R, et al (2003) Does ultrasound contrast agent improve the diagnostic value of colour and power Doppler sonography in superficial lymph node enlargement? Eur J Radiol 48:252–257
Ahuja AT, Ying M (2004) Evaluation of cervical lymph node vascularity: a comparison of colour Doppler, power Doppler and 3-D power Doppler sonography. Ultrasound Med Biol 12:1557–1564
Solbiati L, Osti V, Cova L, et al (2001) Ultrasound of thyroid, parathyroid gland and neck nodes. Eur Radiol 11:2411–2424
Bagla S, Tunkel D, Kraut MA (2003) Nontuberculous mycobacterial lymphadenitis of the head and neck: radiologic observations and clinical context. Pediatr Radiol 33:402–406
Danielides V, Patrikakos G, Moerman M, et al (2003) Diagnosis, management and surgical treatment of non-tuberculous mycobacterial head and neck infection in children. ORL J Otorhinolaryngol Relat Spec 64:284–289
Schaad UB, Votteler TP, McCracken GH Jr, et al (1979) Management of atypical mycobacterial lymphadenitis in childhood: a review based on 380 cases. J Pediatr 95:356–360
Margileth AM, Chandra R, Altman RP (1984) Chronic lymphadenopathy due to mycobacterial infection. Am J Dis Child 138:917–922
Rahal A, Abela A, Arcand PH, et al (2001) Nontuberculous mycobacterial adenitis of the head and neck in children: experience from a tertiary care pediatric center. Laryngoscope 111:1791–1796
Acknowledgements
The study was supported by grants from the Netherlands Organization for Scientific Research (ZonMw), grant no. 945-02-019, and from the Leiden Foundation Microbiology. We thank all the children who took part in the study, and their parents.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindeboom, J.A., Smets, A.M.J.B., Kuijper, E.J. et al. The sonographic characteristics of nontuberculous mycobacterial cervicofacial lymphadenitis in children. Pediatr Radiol 36, 1063–1067 (2006). https://doi.org/10.1007/s00247-006-0271-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-006-0271-6