Abstract
Sickle cell disease is associated with a high risk of stroke in the early years of childhood. The risk of a secondary stroke can be significantly reduced through chronic blood transfusions. Prevention of the first stroke (primary prevention) was made possible through the use of transcranial Doppler (TCD) US and demonstrated in a randomized clinical trial called the stroke prevention trial in sickle cell anemia (STOP). TCD results were classified as normal, conditional, abnormal or inadequate based on velocity readings in specific arterial segments. The MCA and ICA were carefully searched to find the highest velocity, and this was used to stratify patients as to stroke risk. Those with abnormal or high-risk TCD received either monthly blood transfusions or no transfusions, and those randomized to transfusion had a much better outcome in terms of stroke (one stroke, versus ten in the control group) and also fewer other medical problems while transfused. TCD screening is recommended for SCD patients to begin at 24 months of age and should be repeated every 6–12 months during early childhood. Transcranial Doppler imaging (TCDI) can be easier to use and learn and with a few adjustments can provide equivalent predictive power. Currently, TCD is the only recommended method for treatment selection for primary-stroke prevention. MRI and MRA can provide important information on the status of the brain and the blood vessels and, when abnormal, indicate greater risk. Although TCD cannot predict all strokes, TCD and TCDI offer an opportunity to apply an effective therapy for patients in this risk group and reduce many first-time strokes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stroke is one of the most serious complications of sickle cell disease (SCD) [1]. It occurs in 11% of patients with homozygous sickle cell disease by the age of 20 years, and the rates in children are particularly high [2]. Cerebral infarction, the most common stroke type in children with SCD, results from occlusion/stenosis of large arteries supplying the brain. The distal intracranial portions of the internal carotid artery (ICA) and the proximal middle cerebral artery (MCA) are particularly prone to stenosis, which can be detected by transcranial Doppler (TCD) US [3]. Most strokes—(>75%) in SCD children—are infarctions. There are fewer hemorrhages in children, and it is less clear how well TCD predicts hemorrhage.
Secondary-stroke prevention with periodic red cell transfusion
Recurrent stroke without transfusion is high (46–90%) [4]. Chronic transfusion apparently (there were no randomized trials) brings about a dramatic reduction in recurrent stroke to less than 10% and has now become routine practice. Maintenance of the sickle hemoglobin (Hb S) to below 30% is customary, although there is debate about whether reduction to this level is necessary, given its attendant iron overload problems.
Predicting stroke in SCD: the MCG TCD stroke model
Although children with SCD are at much higher risk than children with normal hemoglobin, their overall unselected incidence is still only 0.5–1% per year. Without a better way to select patients for treatment, this would mean that one would have to transfuse more than 100 children for a year to prevent one stroke. TCD is now well-established as a predictor of future cerebrovascular symptoms in long-term prospective studies [5, 6]. Silent lesions on MRI have been reported, and recently the CSSCD group reported that silent infarcts predict future CNS problems, which are mostly more silent lesions, but also clinical stroke. Silent brain infarction has been detected in 10–20% of SCD patients studied with MRI, but the MRI’s predictive power is less robust than TCD [7]. From this paper, the risk of stroke in those with so-called silent lesions was 1.45%, compared to 0.11% for those without such lesions. Although the relative risk was 14-fold, the absolute yearly risk is only about three times the unselected stroke rate from the CSSCD; MRI from these data is not as robust a predictor, but it is widely available and could be used if TCD were not available. Currently, silent MRI lesions are not an indication for chronic transfusion, although a trial (SITT) is underway to test transfusion in this setting. In this trial, children are screened prior to entry for a TCD indication for transfusion, and if an indication does not exist and they have a silent infarction, they will be randomized to chronic transfusion or observation. There are data suggesting that MRA predicts stroke in patients with abnormal TCD [8], but more data are needed to relate specific MRA findings with yearly risk.
Primary prevention: the STOP study design and results
Primary prevention, that is, prevention of the first rather than a recurrent stroke, was made possible by the predictive power of TCD, which allowed a randomized, controlled clinical trial (STOP) of chronic blood transfusion [9]. Children with SCD aged 2–16 years with no history of stroke were screened with TCD for an elevated time-averaged mean of the maximum velocity (TAMMX). [Note: Acuson (Siemans Medical Solutions, Mountain View, Calif., USA) labels this velocity time average of the maximum (TAMX), and Advanced Technology Laboratories (Philips Medical Systems, Bothell, Wash., USA) labels this velocity time-average peak (TAP)]). An elevated TAMMX in either the ICA or the MCA of ≥200 cm/s was required for randomization to either transfusion (regular red cell infusions sufficient to lower and maintain Hb S to <30% of total Hb) or standard care (no transfusions). Primary endpoints of cerebral infarction or intracerebral hemorrhage were determined by a blinded panel, and the incidence of stroke in the two groups was compared using survival analysis. From 1,934 children screened at 14 sites, 130 children with a mean age of 8.3±3.3 years were randomized to transfusion (n=63) or standard care (n=67). The two groups were balanced with respect to important baseline variables, except that the transfusion group had a slightly lower baseline Hb (7.2 vs 7.6 gm/dl, P=0.001). Transfusion was associated with a 92% reduction in stroke by intention-to-treat analysis (P=0.0009) and a 91% reduction (P=0.0017) if one patient, who was discovered on day 2 to have a subacute intracerebral hematoma, is excluded. Regular erythrocyte transfusions were associated with a marked reduction in first stroke in children with SCD who were shown by TCD to be at high risk (Fig. 1) [10].
A 2.5-year-old child with SCD was noted to have bilateral MCA velocities between 180 cm/s and 200 cm/s during initial screening exam. The patient was lost to follow-up and returned 2 years later with clinical symptoms of a stroke. a Coronally reconstructed anterior circulation 3-D time-of-flight MRA demonstrates marked narrowing and tortuosity of the right supraclinoid ICA and narrowing of the left anterior communicating artery. Multiple collaterals extend from the left MCA. b Axial FSE T2-weighted imaging of the brain demonstrates extensive infarction of the left MCA territory of varying stages, as well as old right frontal cortical infarction
Discussion
When can transfusion be safely stopped?
This is the subject of STOP II, but it was halted in late 2004 because of the higher incidence of stroke in those taken off transfusions. There is yet no agreement on when transfusion can be safely stopped when it is used either after a stroke or for prevention of a first stroke. (See the final article in this mini-symposium.)
How patient results were classified as to stroke risk
Transcranial Doppler was read by selection of representative velocities (peak systolic, TAMMX, diastolic) for each of these 15 arterial segments: right and left distal to proximal middle cerebral artery (MCA), bifurcation (BIF), distal internal cerebral artery (dICA), anterior cerebral artery (ACA), posterior cerebral artery (PCA), and the basilar (BA). Velocities were used to classify the study into one of four exclusive categories:(1) normal; (2) conditional A, B, or C; (3) abnormal; or (4) inadequate.
Adequate: the MCA and bifurcation areas had to be represented with the MCA tracked in 2 mm increments out to at least 42 mm or less.
Normal: no velocity over 170 cm/s in any artery.
Abnormal: ≥200 cm/s time-averaged maximum mean (TAMMX) had to be reached in one or more of the following arterial segments: MCA, BIF, dICA. If this happened, the study was classified as abnormal regardless of the results or the readability of the opposite side of the TCD study.
Inadequate: as above (unless one side qualified as abnormal).
Conditional: the remaining adequate studies were classified as follows: TAMMX velocity of between 170 and 199 cm/s in one or more of the segments M1, MCA, BIF, or dICA led to classification as a “conditional 2A”; any velocity in the PCA, TOB or BAS ≥170 cm/s was classified as “conditional 2B”; an ACA ≥170 cm/s was classified as “conditional 2C.” In STOP, screening began in January 1995 and closed November 1996 after 3,929 TCDs had been performed on 1,934 children (range, 68–294 cm/s across the 14 sites). The rates among initial examinations: abnormal −9.4%; conditional −17.3%; normal −67.9%; inadequate −5.4%. The abnormal TAMMX in the initial examinations ranged from 200 cm/s to 334 cm/s. The rate of abnormals varied with age: 2–8 years −10.9%; 9–12 years −9.7%; 13–16 years −6.5% (P=0.027).
How did the STOP examination protocol differ from most clinical protocols?
The primary differences were: (1) The flow rates even without stenosis are by other standards pathologically high, and there might be turbulence even without lesions. (2) The examination provides essentially three levels of information: (a) a detailed listing of systolic, time-averaged maximum mean and diastolic velocities of not only the key arterial segments, the MCA and ICA, but also other arteries including the ACA, PCA and the basilar; (b) from these data is derived a single number, comparable in a sense to a cholesterol level or a CD 4 count, on which the patient’s risk is based; (c) based on this velocity number, the patient’s risk is categorized into one of the four risk groups described above. The cut points used in STOP were arbitrary, and although there is still much to be learned about the risk associated with different TCD results. These categories worked well, and the cutoff of 200 cm/s, confirmed with a second examination and supported by the MCG cohort, was corroborated in the STOP study. The most crucial difference between the STOP examination and most clinical examinations is that in STOP, a concerted effort is made to search carefully along the MCA/ICA to find the highest velocity. If one gets this number right, then the prospective data of almost 5,000 TCD examinations in more than 2,000 children can be drawn upon. If one does not get this number right, either by underestimating velocity by not optimizing the examination, or by not carefully searching the artery, or by overestimating by allowing the child to go to sleep during the examination, that examination cannot be accurately related to the data in the MCG cohort [5, 6] and STOP [10]. It can be argued that basing the entire interpretation on one number is simplistic, and in fact, further criteria might emerge with more data. The reason to keep it simple has more to do with statistical concerns than anything else. When using TCD to select for a potentially toxic therapy such as transfusion, a high degree of specificity is desirable. More criteria might improve sensitivity, but would almost surely degrade specificity.
Where is the highest velocity—the one used for risk stratification—typically found?
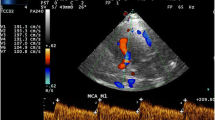
Among the more than 4,000 TCD studies in STOP, more than 250 were abnormal. The qualifying, or highest, velocity was found in the MCA, usually at 46–50 mm depth, in about 85% of cases; it was found in the dICA in about 12% of cases, and in the rest it was found either in the bifurcation area or the more distal segments of the MCA (Fig. 2).
A 9-year-old child with SCD. a TCD demonstrates abnormal right MCA time-average maximum mean velocities measuring over 240 cm/s and a peak systolic velocity of 300 cm/s. b Coronally reconstructed anterior circulation from 3-D time-of-flight MRA demonstrates marked narrowing of the right MCA as well as some narrowing of the right proximal ACA
Do velocities from other arteries figure into risk stratification?
There are two reasons for doing a complete TCD: (1) we might someday figure out how to employ the other arterial velocities (such as data from the ACA) into an advanced predictive score. In fact, a recent analysis of STOP data suggested that velocity elevation in the ACA did contribute to data from MCA/ICA arterial segments for risk prediction [11]; (2) also, although we did not use the ACA or other arteries in the STOP protocol risk reading, it is reasonable to comment on major abnormalities seen in these vessels in interpretations made in the clinical setting.
What is learned from the waveform, and what do low velocities mean?
From a STOP perspective, no waveform information is used to indicate risk. However, this too, is under study, and waveforms that show an extremely dampened appearance (low resistive index) are consistent with severe stenosis, especially when seen with low velocities. Although only high velocities were used in STOP to indicate elevated stroke risk, it is known that TCD velocities might not remain high after vessel stenosis advances to a critical flow-limiting point. By the time many patients become symptomatic, they no longer have high-velocity Doppler signals for several reasons, including: (a) occlusion of a previously stenotic artery; (b) development of collaterals with resultant decrease in flow through the artery in question; and (c) decrease in blood flow demand caused by infarction, which will be reflected in arterial decrease in velocity. In a study that directly compared TCD to cerebral angiography of 31 symptomatic patients, 18 had high velocity (>190 cm/s) TCD in areas of stenosis, but 11 had abnormally low velocities, and these generally correlated with internal carotid artery occlusion on catheter angiography [12]. The criterion found useful in this study was 70 cm/s (which is about 2SD below normal for a young child with SCD), or less than 50% of the contralateral artery’s velocity.
Why have a “confirmation” TCD?
A confirmatory TCD was added because intracranial velocities can show as much as a 10–15% variation over minutes to hours due to normal physiological and pathological factors that alter cerebral blood flow. About 15% of those restudied did not confirm. Almost all of these were children with TAMMX near the 200 cm/s cut point on the first examination. In STOP, it was learned that if a child had a TAMMX of 220 cm/s or more, they had >95% chance of having a second abnormal TCD on repeat testing, and for this reason a single high abnormal TCD (>220 cm/s) is now considered sufficient to establish high risk.
When should TCD screening start?
Current recommendations are for screening to start at age 2 years [13, 14]. Because children up to age 10 have high stroke rates, the younger years are crucial for prevention of stroke. TCD can be performed in most children younger than 2 years, but it is not clear how the results should be interpreted or used clinically. In the ongoing study of hydroxyurea in infants with SCD (BABYHUG) children 6–24 months are being studied. TCD is an exclusion criterion, meaning that if the TCD is abnormal, the child would be considered for transfusion rather than enrolled in the study [15].
How often should TCD be repeated?
It has been recommended that TCD be performed every 6–12 months during early childhood, when the risk for stroke is highest [13, 15]. However, less often might be sufficient, depending on whether the last TCD was normal or showed some other result. In STOP, some patients with normal or conditional study results were rescreened later and some of these had a different result. Patients with TCD in the conditional range, especially if the velocities are close to 200 cm/s, probably ought to be rescreened relatively soon. New information from STOP on the risk implications of normal, conditional, and inadequate TCD after follow-up on the entire screened population of 2,020 children might help answer the question of how often to perform TCD [16]. The main finding from this analysis is that the younger the patient is and the higher the TAMMX on the last TCD (the closer to 200 cm/s), the more likely the child is to convert to high-risk TCD with a later examination. Such children should receive preferential rescreening. Specific recommendations based on age and velocity are being developed based on this long-term follow-up data.
Does the TCD imaging (TCDI) technique obtain velocities similar to the non-imaging technique used in STOP?
The short answer is that with a few adjustments in technique and cut-point velocities, TCDI provides comparable velocity information and might be easier to learn and use. There have been three studies correlating same-day TCD STOP protocol (Nicolet EME TC2000 Madison, Wis., USA) with velocity data from various TCDI systems (Acuson/Siemans Medical Solutions, ATL/Philips Medical Systems, General Electric) using the STOP protocol. It appears that TCD imaging velocities are approximately 10% lower than TCD velocities [17–19].
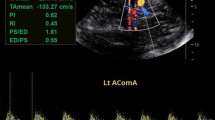
If using TCDI, what velocity criteria should be used?
Correlation studies between TCDI systems and TCD have shown a systematic offset of about 10%, with TCDI measurements of systolic or time-average of the mean of the maximum (TAMMX) measured lower than TCD for the same patient. Accordingly, to be comparable to a 200 cm/s TAMMX using TCDI, the velocity cutoff of 185 cm/s has been recommended [20].
Can peak systolic be used instead of TAMM?
This question was recently examined using data from the STOP study by comparing stroke prediction between systolic and TAMMX velocities from the same examination [21]. This was possible because in STOP the reader read both the peak systolic velocity (PSV), the diastolic (DV) and the TAMMX in a blinded fashion, although only TAMMX was considered in the STOP trial itself. In this report, TAMMX and PSV were superior to DV, and PSV appeared to predict stroke as well as TAMMX. The authors recommended these cut points for PSV when using TCDI compared to TAMMX from TCD.
System used | Velocity | High risk (cm/s) | Conditional (cm/s) |
|---|---|---|---|
TCD | TAMMX | 200 | 170 |
TCDI | PSV | 250 | 200 |
Can other tests substitute for TCD?
Currently, only TCD is recommended for primary-stroke prevention treatment selection. Other tests providing information on the condition of the brain and the arteries such as MRI of the brain and magnetic resonance angiography (MRA) might be found with further research to provide additional or complementary information on stroke risk. The risk associated with abnormal MRI (showing a silent infarct) is estimated from CSSCD data as cited above. One series has reported MRA to be predictive of future stroke, but prospective data have not been sufficient to generate quantitative risk stratification based on particular MRA findings [8]. Many would believe that an MRA with significant signal dropout or flow loss suggests a higher risk for stroke, but precisely which finding implies a fivefold, tenfold or 20-fold risk beyond the baseline of 0.5–1% per year for stroke is not clear.
Limitations of TCD
Not all strokes were predicted by TCD. The reasons for stroke with normal TCD are not known, but might be the timing or quality of the examinations in some cases. Some of these strokes might be caused by small-vessel disease where large arteries are not involved. In addition, whether TCD predicts subarachnoid hemorrhage, an uncommon but important type of stroke in these children, is not clear [16].
In summary, TCD and TCDI offer an opportunity to selectively and rationally apply a very effective preventive therapy, chronic transfusion, and might also be important surrogate markers for risk in future studies involving other agents. Early and repeated screening, with appropriate follow-up and action, should reduce first stroke substantially, and there is evidence from a study performed in California that the rate of first stroke in SCD is dropping in the post-STOP era [21, 22]. Widespread screening can make an impact, and pediatric radiologists play a crucial role in the provision of this service.
References
Adams RJ (1994) Neurological complications. In: Embury SH, Hebbel RP, Narla M, et al (eds) Sickle cell disease:scientific principles and clinical practice, vol 40. Raven Press, New York, pp 599–621
Ohene-Frempong K, Wiener SJ, Sleeper LA, et al, and the Cooperative Study of Sickle Cell Disease (1998) Cerebrovascular accidents in sickle cell disease:rates and risk factors. Blood 91:288–294
Adams RJ, Litaker M, Nichols FT (1993). Anemia and sickle cell disease. In: Babikian V, Wechsler L (eds) Transcranial Doppler ultrasonography. Decker-Mosby, Philadelphia, pp 160–171
Pegelow CH, Adams RJ, McKie V, et al (1995) Risk of recurrent stroke in patients with sickle cell disease treated with erythrocyte transfusions. J Pediatr 126:896–899
Adams RJ, McKie V, Nichols FT, et al (1992) The use of transcranial ultrasonography to predict stroke in sickle cell disease. N Engl J Med 326:605–610
Adams RJ, McKie VC, Carl EM, et al (1997) Long-term stroke risk in children with sickle cell disease screened with transcranial Doppler. Ann Neurol 42:699–704
Miller ST, Macklin EA, Pegelow CH, et al (2001) The Cooperative Study of Sickle Cell Disease. Silent infarction as a risk factor for overt stroke in children with sickle cell anemia:a report from the Cooperative Study of Sickle Cell Disease. J Pediatr 139:385–390
Seibert J, Glasier C, Kirby R, et al (1998) Transcranial Doppler (TCD), MRA and MRI as a screening examination for cerebrovascular disease in patients with sickle cell anemia—an eight-year study. Pediatr Radiol 28:138–142
Adams RJ, McKie VC, Brambilla DJ, et al (1997) Stroke Prevention Trial in Sickle Cell Anemia (“STOP”): study design. Contr Clin Trials 19:110–129
Adams RJ, McKie VC, Hsu L, et al (1998) Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. N Engl J Med 339:5–11
Kwiatkowski JL, Granger S, Brambilla D, et al for the STOP study investigators (2003) Elevated blood flow velocity in the anterior cerebral artery and stroke risk in sickle cell disease. Blood 102:120
Adams RJ, Nichols FT, Figueroa R, et al (1992) Transcranial Doppler correlation with cerebral angiography in sickle cell disease. Stroke 23:1073–1077
Clinical alert. National Heart Lung and Blood Institute, September 19, 1997
Goldstein LB, Adams RJ, Becker K, et al (2001) AHA scientific statement. Primary prevention of ischemic stroke: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke 32:280–299
Adams RJ, Brambilla DJ, Granger S, for the STOP study investigative team (2004) Stroke and conversion to high risk in children screened with transcranial Doppler ultrasound during the STOP Study. Blood 103:3689–3694
Bulas DI, Jones A, Siebert JJ, et al (2000) Transcranial Doppler (TCD) screening for stroke prevention in sickle cell anemia: pitfalls in technique variation. Pediatr Radiol 30:733–738
Jones AM, Seibert JJ, Nichols FT, et al (2001) Comparison of transcranial color Doppler imaging (TCDI) and transcranial Doppler (TCD) in children with sickle cell anemia. Pediatr Radiol 31:461–469
Neish A, Blews DE, Sims CA, et al (2002) Screening for stroke in sickle cells anemia: comparison of transcranial Doppler imaging and non-imaging US techniques. Radiology 222:709–714
Jones A, Granger S, Brambilla D, et al (2004) Peak systolic and diastolic transcranial Doppler velocities for prediction of stroke in sickle cell anemia. Pediatr Radiol (in press)
Adams RJ, Pavlakis S, Roach ES (2003) Sickle cell disease and stroke:primary prevention and transcranial Doppler. Ann Neurol 54:559–563
Fullerton H, Johnston SC, Zhao S, et al (2004) Declining rates in Californian children with sickle cell disease. Blood 104:336–339
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adams, R.J. TCD in sickle cell disease: an important and useful test. Pediatr Radiol 35, 229–234 (2005). https://doi.org/10.1007/s00247-005-1409-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-005-1409-7