Abstract
This review focuses on imaging of osteosarcoma and Ewing’s sarcoma of the long bones in children during preoperative neoadjuvant chemotherapy. Morphological criteria on plain films and conventional static MRI are insufficiently correlated with histological response. We review the contribution of dynamic MRI, diffusion-weighted MR and nuclear medicine (18FDG-PET) to monitor tumoural necrosis. MRI is currently the best method to evaluate local extension prior to tumour resection, especially to assess the feasibility of conservative surgery. Quantitative models in dynamic MRI and 18FDG-PET are currently being developed in order to find new early prognostic criteria, but for the time being, treatment protocols are still based on the gold standard of histological response.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma and Ewing’s sarcoma represent more than 90% of all primary malignant bone tumours in children. The current treatment for localized forms is based on neoadjuvant chemotherapy designed to treat micrometastatic disease and reduce primary tumour volume to facilitate the subsequent surgical procedure. Surgery must be as conservative as possible, but must also ensure complete resection [1–3]. After diagnosis, the role of imaging is to evaluate the degree of local extension precisely prior to surgery and to assess the response to neoadjuvant chemotherapy. The current challenge for imaging is to define new treatment response criteria and to identify new prognostic factors.
Current therapeutic protocols and prognostic factors
Treatment strategy
Treatment protocols for localised bone tumours are based on neoadjuvant chemotherapy. The reference drug for osteosarcomas is high-dose methotrexate; it is combined with other drugs such as doxorubicin or vepeside and ifosfamide over a period of about 11 weeks for osteosarcomas [4]. Six cycles of vincristine, ifosfamide, doxorubicin and etoposide are given over a period of 15 weeks for Ewing’s sarcoma (Euro-E.W.I.N.G. 99 protocol). This chemotherapy is followed by en bloc resection of the tumour, including the biopsy track, with variable reconstruction modalities (allografts, autografts, metallic prostheses, growth prostheses, rotation plasty) [5]. The amputation rate has been considerably decreased as a result of this approach. Local treatment of Ewing’s sarcoma may also be based on radiotherapy, notably in inoperable forms. Postoperative chemotherapy is adapted to the prognostic factors.
Prognostic factors
Apart from metastatic forms, the histological response to neoadjuvant chemotherapy remains the major prognostic criterion used for treatment of osteosarcoma [6–8] and Ewing’s sarcoma [9–11]. Good responders are defined by the percentage of residual viable cells below 5 or 10%, according to the protocol. The initial tumour volume is also considered to be a prognostic factor for some Ewing’s sarcomas, especially those treated by radiotherapy [9, 12, 13], and for osteosarcomas [14, 15]. New prognostic factors have recently been demonstrated, such as the presence of bone marrow micrometastases or circulating tumour cells detected by RT-PCR (reverse transcription-polymerase chain reaction) at the time of diagnosis for Ewing’s sarcomas [16].
Technical recommendations for MR examination
After conventional radiography, MRI is the second-line examination recommended by the ACR for invasive bone tumours of the extremities [17] (Table 1). A study by the Radiology Diagnostic Oncology Group in 1997 showed no statistically significant difference between MRI and CT for local staging assessment [18]. However, because of the quality of assessment of intramedullary and soft tissue extension, most authors consider MRI to be the imaging modality of choice for local staging assessment and evaluation of response to treatment [19–22].
The initial MRI should be performed prior to any biopsy procedure, which can induce intramedullary oedema that may interfere with the staging assessment. MRI also guides the surgeon’s choice of biopsy path [22, 23]. Efficient analgesia is mandatory before the examination at diagnosis in order to avoid motion artefacts. The field of view must be large enough to cover the entire bone segment. Depending on the available options, it is recommended that either phased-array surface multicoils allowing complete analysis be used or a two-stage examination be performed using the body coil for global analysis of the bone segment and a surface coil on the lesion. At least two perpendicular section planes are necessary, one parallel and the other perpendicular to the long axis of the bone. For lower limb tumours, comparative frontal study of the two bone segments facilitates analysis of the bone marrow signal (zones of haematopoiesis).
T1- and T2-weighted (T2-W) spin-echo or rapid spin-echo sequences (RARE, FSE, TSE) and STIR sequences are used [22]. STIR sequences reduce the fat signal and increase tumour signal by combining T1 and T2 effects [24–26]. They must be acquired before injection of contrast medium because the signal of vascularized zones may be suppressed [27]. Fat suppression options increase the contrast on T2-W [26] and contrast-enhanced T1-W sequences [28]. However, in the absence of fat suppression, injection of contrast agent limits evaluation of intramedullary, perineurovascular and synovial extension [29]. The value of conventional late gadolinium-enhanced sequences is a subject of debate, as enhancement is nonspecific and is observed in both the tumour and the reactive tissue around the tumour [20, 29, 30]. When contrast-enhanced sequences are obtained, 3D T1-W rapid gradient-echo with dynamic acquisition should be performed, allowing evaluation of early enhancement of the lesions, correlated with viable tumour zones. Vascular relations can be determined preoperatively by MR angiography with maximum intensity projection (MIP) reconstructions [31, 32].
Monitoring response to neoadjuvant chemotherapy
Response to chemotherapy is an essential prognostic criterion, but is based on the histological gold standard obtained late during management. Many studies have therefore tried to evaluate this response earlier in the course of treatment.
Plain films
Volume reduction, calcification of residual tumour in soft tissues and the medullary cavity and accentuation of the periosteal reaction have been described as predictive of good response [33, 34]. Conversely, an increase or stability of the soft-tissue mass, associated with accentuation of the invasive appearance, favours local progression [35]. However, these changes are very variable and insufficiently correlated with histological response [36].
MR signal intensity modifications
Various phenomena are observed during tumour regression: necrosis, haemorrhage (with haemosiderin deposition), development of granulation tissue, fibrosis and organization of a pseudocapsule around the extraosseous component [37].
T2 signal variations were initially described as being associated with a good histological response: decreased signal of the extraosseous tumour component [38], or, in the case of Ewing’s sarcoma, a pseudocystic increase of the intramedullary signal [39]. The presence of viable residual Ewing’s sarcoma was subsequently described in territories with both high T2 signal and low T2 signal [40]. In osteosarcomas, a ‘necrotic’ cystic appearance is also described in association with the presence of viable cells in the periphery of cysts [37]. Other studies have shown that the only significant finding is persistence or increase of peritumoural oedema on T2-W sequences, which, when associated with an increase in tumour volume, is predictive of poor response [41]. On gadolinium-enhanced sequences, late enhancement evaluated on static MRI is also an insufficient criterion, as it cannot distinguish residual viable tumour from granulation tissue secondary to tumour necrosis that is also highly vascular. Although static MRI clearly demonstrates signal changes associated with the effects of chemotherapy, it appears to be insufficient to quantify viable residual tumour.
Tumour volume
The length of intramedullary signal abnormalities do not vary in response to chemotherapy [42]. Only the transverse dimensions of the soft-tissue component usually reflect a reduction of tumour volume. As a result, the volume ‘response’ cannot be evaluated for strictly intraosseous lesions. Volume reduction is usually more pronounced in Ewing’s sarcomas than in osteosarcomas, in which regression of the osteoid matrix occurs more slowly [39, 43, 44].
Correlation between tumour volume and histological response
For osteosarcomas, an increase in volume is described as being well correlated with a poor histological response, while stability or regression is insufficiently predictive of a good response (PPV <60%) [35, 41]. Actually, progressive calcification of the soft tissue involvement related to persistent activity of the osteogenic matrix can be responsible for stable volume despite a good response [43]. In our experience, an increase in tumour volume can also be observed in histologically good-responder osteosarcomas, related to tumour necrosis phenomena (Fig. 1). The correlation between volume response and histological response is better for Ewing’s sarcomas, but difficult to quantify accurately [44, 45].
An 8-year-old girl with a tibial osteosarcoma in the right leg. a Plain radiograph and b frontal T1-W MRI at diagnosis. At the midpoint of preoperative chemotherapy (after four courses), while the child was painless, frontal T1-W (c) and axial fat-saturated T2-W MRI (d) show a global increase of tumour-containing multiple cystic areas with fluid-fluid levels. Despite this volume ‘progression’, pathological analysis after surgery demonstrated a very good histological response (less than 1% of viable cells)
Correlation between tumour volume and survival
There is no significant correlation between volume response and patient survival in osteosarcomas [35] and in the small paediatric series reported on Ewing’s sarcomas [12, 44]. Nevertheless, the initial tumour volume in Ewing’s sarcomas is of prognostic significance. The outcome of patients with tumoural volume under 200 ml is more favourable than patients with larger tumours [12].
For clinical practice, tumour measurements performed during chemotherapy have a limited prognostic value. Measured volumes must therefore be interpreted cautiously; apparent ‘stable disease’ can be related to a small extraosseous component or to the osteogenic matrix of an osteosarcoma. The diagnosis of tumour ‘progression’ must also be established cautiously, especially in osteosarcomas. MR findings must always be correlated with clinical criteria (especially the need to continue analgesic therapy), plain films, tumour signal changes and signs of metastatic spread.
Dynamic MRI
Principles
Dynamic MRI is based on the study of the initial distribution of low-molecular weight gadolinium chelates after bolus injection. It provides information about tissue perfusion, capillary permeability and interstitial volume [27]. The technique is usually performed at 1.5 T with rapid-3D-spoiled-gradient-echo sequences (Table 1). High temporal resolution (<15 s) is mandatory to differentiate viable malignant tumour zones, presenting early and intense enhancement (the steady-state may be reached in 25–30 s in osteosarcomas), from more slowly enhanced avascular necrotic territories and zones of fibrosis. Acquisitions are repeated for 5 min after rapid injection of the contrast agent (gadolinium, 0.1 mmol/kg patient weight; 3–5 ml/s with i.v. manual bolus injection, followed by 20 ml saline flush) [27, 46–48, 49]. This high temporal resolution constituted an intrinsic limit of the method, as it limited the number of sections and only allowed examination of part of the tumour, as in histology, but the more recent MR units are now able to analyse larger volumes.
Contribution of morphological dynamic MRI
A first, purely qualitative analysis of rapidly enhanced zones detects areas of viable tumour [46, 50, 51]. The sensitivity of this method is increased by subtraction techniques [27, 51]. A good correlation with histological response was initially reported for osteosarcomas, as good responders presented non-enhanced lesions, with or without fine linear or nodular enhancement <3 mm [30]. With high temporal resolution, enhancement is considered to be significant when it is observed within 6 s after arterial enhancement (i.e. 10–20 s after injection), with a limit of detection of 3–5 mm2 [51]. In children, interpretation of images before fusion of the epiphyses must take into account the physiological enhancement of vessels situated on both sides of the growth plate [51].
Contribution of quantitative dynamic MRI
Quantitative information can be extracted from dynamic acquisition by selecting a region of interest (ROI) on all or part of the tumour on the image and obtaining a time/intensity curve. Several indices can be calculated from this curve, based on the relative intensity of contrast enhancement and/or the enhancement slope [46, 47, 52, 53] (Fig. 2). Two-compartmental pharmacokinetic models have also been evaluated in osteosarcomas and Ewing’s sarcomas [53–55]. These models more precisely reflect tumour microvascularization by taking into account contrast agent uptake and elimination (wash out) and can theoretically predict the accessibility of the tumour to drugs before treatment, and viability of residual tumour after treatment [49, 55]. Limitations in the model approach are more complex analysis routines and the inability to determine whether changes in uptake in regions of necrosis are due to variance in flow or permeability [53].
A 14-year-old girl with a tibial osteosarcoma in the left leg. Initial conventional MR views: a coronal T1-W, b coronal fat-saturated T2-W, c coronal fat-saturated late contrast-enhanced T1-W. 3D T1-W dynamic acquisition repeated during 5 min: d enhancement at 60 s; e relative enhancement-weighted and f maximum initial slope-weighted parametric images show high enhancement rates and slopes within the lesion. g ROI may be defined around the tumour to study the enhancement curve (relative MR unit per s) (h). i Coronal fat-saturated late contrast-enhanced T1-W image after neoadjuvant chemotherapy displays no significant volume response (15% decrease); conversely, a maximum initial slope-weighted parametric image (j) shows only a few peripheral residual areas of rapid enhancement (arrows) and the enhancement curve (k) shows a decrease of relative enhancement and of initial slope. l Pathological analysis (courtesy of Dr. G. De Pinieux) confirms the overall good response (95% necrosis rate) despite residual foci of viable tumour within the peripheral soft tissue extension
By combining morphological data and quantitative measures, parametric imaging allows mapping based on various indices such as the enhancement slope (so-called ‘first-pass’ imaging) [47], or based on pharmacokinetic indices [54]. It allows rapid visual analysis of hypervascular territories of viable tumour. In the future, this method could constitute an index of residual tumour viability for inoperable sites.
Preoperative quantitative analysis, with the use of cut-off values, appears to be relatively well correlated with histological response of osteosarcomas, as good responders are detected with a sensitivity of 81% and a specificity of 85% [55]. Individual relative variations of quantitative indices before and after chemotherapy are also well correlated with histological response (accuracy 91%) [56]. However, this correlation is not observed for MRI performed at the midpoint of chemotherapy [56]. Quantitative dynamic MRI with pharmacokinetic model was recently compared to patient survival in two paediatric pilot studies. The results were not significant for Ewing’s sarcomas [12], but appeared to be significant in a series of large osteosarcomas, but only at the end of chemotherapy [55].
Standardization and routine use of dynamic MRI are currently limited by the sophisticated and rapidly evolving performances of post-processing using various mathematical models. For the time being, treatment protocols are therefore still based on the gold standard of histological response, the most robust prognostic criterion. Recent studies have been essentially designed to find a direct correlation between tumour perfusion parameters and patient survival, not only preoperatively, but especially from the time of diagnosis, in order to select future good or poor responders immediately [12, 55]. The follow-up is still insufficient to assess the reliability of these new indices.
Diffusion-weighted MRI
Diffusion-weighted MRI of bone marrow can distinguish highly cellular lesions from lesions with a predominant extracellular compartment and therefore contributes to the diagnosis of malignancy in musculoskeletal disease. This technique can be used to obtain qualitative morphological data [57], but with a loss of specificity related to the T2 effect. The specificity of the technique can be increased by quantitative measurement of the apparent diffusion coefficient [58, 59], which has essentially been used on the spine or on animal models of osteosarcoma [58], but its exact place in paediatric clinical practice has yet to be defined.
Nuclear medicine
Technetium-labelled diphosphonate bone scan (99mTc-MDP)
The bone scan is not sufficiently specific for assessment of response. Its low specificity is due to the fact that tissue-repair phenomena take up the radioactive tracer in the same way as residual tumour [19]. Multiphase dynamic scintigraphy shows a better correlation with histological response [20, 60, 61]. Its accuracy for evaluation of histological response at the end of treatment for osteosarcomas appears to be comparable to that of dynamic MRI [56].
18-fluorodeoxyglucose positron emission tomography
18-fluorodeoxyglucose (18FDG) is the radioisotope classically used for positron emission tomography (PET). This metabolite of glucose is phosphorylated in the body by a hexokinase, then bound by cells in the form of 18FDG-6-phosphate and then slowly dephosphorylated in the cell. At the time of acquisition of an 18FDG-PET examination, the radioactivity recorded therefore essentially reflects the tissue metabolism of 18FDG-6-phosphate.
In primary malignant bone tumours in children, this radioactive tracer can be more specific of tumour cell metabolism than technetium-labelled diphosphonates. Because of the intrinsic osteogenic activity of osteosarcomas, bone scintigraphy detects not only tumour activity, but also the reaction to any form of bone aggression, which does not necessarily reflect tumour proliferation.
Only limited data are currently available concerning 18FDG-PET for preoperative assessment of response to chemotherapy and are essentially derived from retrospective studies. In all reported cases, there is a correlation between uptake intensity after chemotherapy and the percentage of viable cells [62–65]. The long-term prognosis of patients considered to be “good responders” by 18FDG-PET is unknown at present and therefore cannot be compared to that of patients with a good histological response. Encouraging results were obtained in a recent study, in which semiquantitative determination of 18FDG uptake by osteosarcomas at the time of diagnosis was correlated with survival [66].
Doppler sonography
Variations of resistance indices in arteries supplying the tumour were evaluated during treatment follow-up. Good correlation was demonstrated between an increase of these indices after two cycles and a good histological response [67]. However, the poor reproducibility of these measurements limits the practical value of this method.
Preoperative assessment
Local staging must be primarily based on the initial MRI, but also on signal variations observed during treatment. Intramedullary extension is evaluated by unenhanced T1-W sequences, which are most closely correlated with tumour size estimated on pathology [42, 68]. STIR sequences overestimate extension compared to T1-W sequences [42]. The dimensions of intramedullary extension usually remain unchanged during preoperative chemotherapy and, except in the case of progression, must be measured on the initial MRI as the marrow signal can be modified during treatment [42].
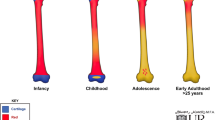
Haematopoietic growth factors used to reduce the duration of chemotherapy-induced neutropenia can be responsible for focal intramedullary signal abnormalities, which must not be confused with tumour progression. These territories of haematopoiesis are visualized as diffuse or focal, linear or nodular, symmetrical or asymmetrical zones of low intensity on T1 and high intensity on T2 and STIR [69–71]. Criteria in favour of this diagnosis are: involvement of other bone segments or bilateral zones, signal abnormalities less pronounced than tumour infiltration. Nuclear medicine may also be misleading in this situation as zones of haematopoiesis associated with increased uptake on bone scan [72] or 18FDG-PET [73] have also been reported.
The incidence of skip metastases is low, estimated to be 3% for osteosarcoma and 4% for Ewing’s sarcoma [74]. The presence of skip metastases reflects haematogenous spread limited to the affected bone and determines the level of surgical resection [22], hence the importance of examining the entire bone segment [75]. MRI appears to be the best technique to visualise skip metastases [22]. Longitudinal T1-W sequences are more sensitive than bone scan in osteosarcomas [19]. Normal MRI is usually sufficient to exclude skip metastasis with a high level of reliability (NPV 96%), but the PPV of MRI is low (14%) due to the rarity of these lesions [18]. These lesions must be distinguished from areas of physiological haematopoiesis in children [76].
Epiphyseal and joint involvement must be determined in order to allow conservative surgery: the growth plate does not constitute a barrier, and epiphyseal extension (mainly studied in metaphyseal osteosarcomas) is observed in 50–88% of cases [77–80]. The epiphysis may be invaded by effraction of the growth plate or by lateral extension. The tumour may extend as far as the joint cartilage or, exceptionally, may even extend beyond the cartilage [78]. Epiphyseal extension is difficult to evaluate with bone scan as a result of physiological uptake by the growth plate [81]. The sensitivity of MRI for the diagnosis of epiphyseal extension is almost 100% [79, 80, 82]. However, the specificity of MRI is lower, a maximum of 90% on T1-W sequences and 70% on STIR sequences [80]. Its overall precision has been estimated to be 90 vs 86% for CT [81].
Peritumoural changes (oedema, haematopoiesis, angiogenesis) can be responsible for false-positive results [80]. An intermediate signal, blurred margins and the absence of architectural abnormalities of the growth plate and epiphysis are suggestive of non-neoplastic signal abnormalities [80]. Conventional T1-W sequences appear to be sufficient for the diagnosis of epiphyseal extension and have a higher specificity than STIR sequences and even quantitative dynamic MRI [80, 82]. Nevertheless, in our experience, qualitative dynamic MRI may help to differentiate inflammatory changes from epiphyseal extension (Fig. 3). The frequency of joint involvement has been estimated to be approximately 20% for bone tumours situated close to joints [83]. This extension is detected by MRI with a very good sensitivity (100%), but with a low specificity (69%) [83]. Contrast-enhanced T1-W sequences are the most sensitive, showing a contrast-enhanced intra-articular mass with interruption of the synovial membrane or joint cartilage. Joint effusion is not a reliable criterion (PPV 27%), but absence of joint effusion is a good negative sign (NPV 92%). Involvement of the cruciate ligaments—extra-articular but intracapsular structures—is frequently observed in the knee. False-positive results of MRI are related to displacement of the capsule by the extraosseous component simulating capsular effraction and synovial contrast enhancement, which can be purely reactive [83].
A 12-year-old boy with a tibial osteosarcoma in the left leg. a Coronal T1-W MRI and b coronal fat-saturated late contrast-enhanced T1-W MRI display the metaphyseal tumour (long arrow) and a medial, small skip lesion (arrowheads). Epiphyseal signal abnormalities (small arrows) and late enhancement are also observed, but dynamic enhanced subtracted coronal view at 30 s (c) does not display any early enhancement within the epiphysis. d Pathological analysis (courtesy of Prof. M. Peuchmaur) confirms involvement of metaphysis and growth plate, and normality of the epiphysis
Soft tissue invasion is accurately evaluated by MRI [19]. Peritumoural oedema presents in the form of a high-intensity signal on T2-W or STIR sequences, which is more marked on more sensitive STIR sequences [25]. Peritumoural oedema and micro-invasion cannot be differentiated within the high-intensity signal [25]. However, a normal muscle volume and the presence of a clearly defined limit between the soft tissue tumour and the high-intensity muscle signal and complete normalization of the muscle signal during treatment are strong arguments against the neoplastic nature of the peritumoural high-intensity signal [84]. Dynamic MRI is able to distinguish between oedema and contiguous tumour invasion [50] (Fig. 4). Parametric information relating to tumour uptake may provide information to the surgeon indicating the extent of the disease [53].
An 8-year-old girl with a tibial osteosarcoma in the right leg. a Sagittal T1-W MRI, b sagittal fat-saturated late contrast-enhanced T1-W, and dynamic enhanced subtracted sagittal at 30 s (c) and 90 s (d). Late enhancement is observed along the posterior cruciate ligament (arrow) on conventional static MR. Dynamic acquisition shows no early enhancement in this area. e Pathological comparison. Absence of tumoural involvement was confirmed on pathological analysis (courtesy of Dr. P. Josset)
Extension to neurovascular bundles must be precisely evaluated on the initial imaging, as it is associated with a risk of incomplete resection [22]. The sensitivity and NPV of MRI for the diagnosis of neurovascular extension appear to be excellent, but the specificity is lower and the PPV has been estimated to be 38.5% for nerve invasion and 53% for vascular invasion [85]. Vascular encasement is rare, but vascular relations must be precisely analysed preoperatively on axial sections. When doubt persists on MRI, conservative surgery is not necessarily impossible, but its feasibility must be re-evaluated intraoperatively [85].
In conclusion, the initial pre-treatment imaging actually remains the most important assessment. The first MRI, performed before treatment and initial biopsy, constitutes the reference for follow-up during treatment and for local staging, which determines the subsequent surgical management. Various nonspecific morphological and signal changes are induced by preoperative chemotherapy, and assessment of response on the basis of these changes must be interpreted cautiously. Dynamic MRI can be used as a complementary technique for local staging and assessment of response for inoperable forms. Quantitative models in dynamic MRI and 18FDG-PET are currently being developed in order to demonstrate early prognostic criteria, which could be decisive in future protocols.
References
Jurgens H, Exner U, Gadner H, et al (1988) Multidisciplinary treatment of primary Ewing’s sarcoma of bone. A 6-year experience of a European cooperative trial. Cancer 61:23–32
Petrilli AS, Gentil FC, Epelman S, et al (1991) Increased survival, limb preservation, and prognostic factors for osteosarcoma. Cancer 68:733–737
Bacci G, Ferrari S, Longhi A, et al (2001) Pattern of relapse in patients with osteosarcoma of the extremities treated with neoadjuvant chemotherapy. Eur J Cancer 37:32–38
Gentet JC, Brunat-Mentigny M, Demaille MC, et al (1997) Ifosfamide and etoposide in childhood osteosarcoma. A phase II study of the French Society of Paediatric Oncology. Eur J Cancer 33:232–237
Dubousset J, Missenard G, Kalifa C (1991) Management of osteogenic sarcoma in children and adolescents. Clin Orthop 270:52–59
Huvos AG, Rosen G, Marcove RC (1977) Primary osteogenic sarcoma: pathologic aspects in 20 patients after treatment with chemotherapy en bloc resection, and prosthetic bone replacement. Arch Pathol Lab Med 101:14–18
Rosen G, Caparros B, Huvos AG, et al (1982) Preoperative chemotherapy for osteogenic sarcoma: selection of postoperative adjuvant chemotherapy based on the response of the primary tumor to preoperative chemotherapy. Cancer 49:1221–1230
Hudson M, Jaffe MR, Jaffe N, et al (1990) Pediatric osteosarcoma: therapeutic strategies, results, and prognostic factors derived from a 10-year experience. J Clin Oncol 8:1988–1997
Picci P, Bohling T, Bacci G, et al (1997) Chemotherapy-induced tumor necrosis as a prognostic factor in localized Ewing’s sarcoma of the extremities. J Clin Oncol 15:1553–1559
Picci P, Rougraff BT, Bacci G, et al (1993) Prognostic significance of histopathologic response to chemotherapy in nonmetastatic Ewing’s sarcoma of the extremities. J Clin Oncol 11:1763–1769
Le Deley MC, Ahrens S, Paulussen M, et al (2001) Histological response is the main prognostic factor of survival in localised Ewing tumour treated with chemotherapy alone before surgery (abstract). In: International Society of Paediatric Oncology XXXIII Meeting and International Society of Paediatric Surgical Oncology XXXIII Meeting. Brisbane, 10–13 October 2001. Med Pediatr Oncol 37:178
Miller SL, Hoffer FA, Reddick WE, et al (2001) Tumor volume or dynamic contrast-enhanced MRI for prediction of clinical outcome of Ewing sarcoma family of tumors. Pediatr Radiol 31:518–523
Oberlin O, Deley MC, Bui BN, et al (2001) Prognostic factors in localized Ewing’s tumours and peripheral neuroectodermal tumours: the third study of the French Society of Paediatric Oncology (EW88 study). Br J Cancer 85:1646–1654
Bieling P, Rehan N, Winkler P, et al (1996) Tumor size and prognosis in aggressively treated osteosarcoma. J Clin Oncol 14:848–858
Ferrari S, Bertoni F, Mercuri M, et al (2001) Predictive factors of disease-free survival for non-metastatic osteosarcoma of the extremity: an analysis of 300 patients treated at the Rizzoli Institute. Ann Oncol 12:1145–1150
Schleiermacher G, Peter M, Oberlin O, et al (2003) Increased risk of systemic relapses associated with bone marrow micrometastasis and circulating tumor cells in localized Ewing tumor. J Clin Oncol 21:85–91
Manaster BJ, Dalinka MK, Alazraki N, et al (2000) Follow-up examinations for bone tumors, soft tissue tumors, and suspected metastasis post therapy. American College of Radiology. ACR Appropriateness Criteria. Radiology 215[Suppl]:379–387
Panicek DM, Gatsonis C, Rosenthal DI, et al (1997) CT and MR imaging in the local staging of primary malignant musculoskeletal neoplasms: report of the Radiology Diagnostic Oncology Group. Radiology 202:237–246
Bloem JL, Taminiau AH, Eulderink F, et al (1988) Radiologic staging of primary bone sarcoma: MR imaging, scintigraphy, angiography, and CT correlated with pathologic examination. Radiology 169:805–810
Fletcher BD (1991) Response of osteosarcoma and Ewing sarcoma to chemotherapy: imaging evaluation. AJR 157:825–833
Fédération Nationale des Centres de Lutte contre le Cancer (FNCLCC) (1997) Standards Options et Recommandations pour le diagnostic, la surveillance et le traitement de l‘Ostéosarcome. John Libbey Eurotext, Montrouge
Leung JC, Dalinka MK (2000) Magnetic resonance imaging in primary bone tumors. Semin Roentgenol 35:297–305
Anderson MW, Temple HT, Dussault RG, et al (1999) Compartmental anatomy: relevance to staging and biopsy of musculoskeletal tumors. AJR 173:1663–1671
Dwyer AJ, Frank JA, Sank VJ, et al (1988) Short-TI inversion-recovery pulse sequence: analysis and initial experience in cancer imaging. Radiology 168:827–836
Shuman WP, Patten RM, Baron RL, et al (1991) Comparison of STIR and spin-echo MR imaging at 1.5 T in 45 suspected extremity tumors: lesion conspicuity and extent. Radiology 179:247–252
Mirowitz SA, Apicella P, Reinus WR, et al (1994) MR imaging of bone marrow lesions: relative conspicuousness on T1-weighted, fat-suppressed T2-weighted, and STIR images. AJR 162:215–221
Verstraete KL, Lang P (2000) Bone and soft tissue tumors: the role of contrast agents for MR imaging. Eur J Radiol 34:229–246
Gronemeyer SA, Kauffman WM, Rocha MS, et al (1997) Fat-saturated contrast-enhanced T1-weighted MRI in evaluation of osteosarcoma and Ewing sarcoma. J Magn Reson Imaging 7:585–589
Seeger LL, Widoff BE, Bassett LW, et al (1991) Preoperative evaluation of osteosarcoma: value of gadopentetate dimeglumine-enhanced MR imaging. AJR 157:347–351
de Baere T, Vanel D, Shapeero LG, et al (1992) Osteosarcoma after chemotherapy: evaluation with contrast material-enhanced subtraction MR imaging. Radiology 185:587–592
Swan JS, Grist TM, Sproat IA, et al (1995) Musculoskeletal neoplasms: preoperative evaluation with MR angiography. Radiology 194:519–524
Lang P, Grampp S, Vahlensieck M, et al (1995) Primary bone tumors: value of MR angiography for preoperative planning and monitoring response to chemotherapy. AJR 165:135–142
Smith J, Heelan RT, Huvos AG, et al (1982) Radiographic changes in primary osteogenic sarcoma following intensive chemotherapy. Radiological–pathological correlation in 63 patients. Radiology 143:355–360
Ehara S, Kattapuram SV, Egglin TK (1991) Ewing’s sarcoma. Radiographic pattern of healing and bony complications in patients with long-term survival. Cancer 68:1531–1535
Lawrence JA, Babyn PS, Chan HS, et al (1993) Extremity osteosarcoma in childhood: prognostic value of radiologic imaging. Radiology 189:43–47
Holscher HC, Hermans J, Nooy MA, et al (1996) Can conventional radiographs be used to monitor the effect of neoadjuvant chemotherapy in patients with osteogenic sarcoma? Skeletal Radiol 25:19–24
Pan G, Raymond AK, Carrasco CH, et al (1990) Osteosarcoma: MR imaging after preoperative chemotherapy. Radiology 174:517–526
Holscher HC, Bloem JL, Nooy MA, et al (1990) The value of MR imaging in monitoring the effect of chemotherapy on bone sarcomas. AJR 154:763–769
Lemmi MA, Fletcher BD, Marina NM, et al (1990) Use of MR imaging to assess results of chemotherapy for Ewing sarcoma. AJR 155:343–346
MacVicar AD, Olliff JF, Pringle J, et al (1992) Ewing sarcoma: MR imaging of chemotherapy-induced changes with histologic correlation. Radiology 184:859–864
Holscher HC, Bloem JL, Vanel D, et al (1992) Osteosarcoma: chemotherapy-induced changes at MR imaging. Radiology 182:839–844
Onikul E, Fletcher BD, Parham DM, et al (1996) Accuracy of MR imaging for estimating intraosseous extent of osteosarcoma. AJR 167:1211–1215
van der Woude HJ, Bloem JL, Hogendoorn PC (1998) Preoperative evaluation and monitoring chemotherapy in patients with high-grade osteogenic and Ewing’s sarcoma: review of current imaging modalities. Skeletal Radiol 27:57–71
Abudu A, Davies AM, Pynsent PB, et al (1999) Tumour volume as a predictor of necrosis after chemotherapy in Ewing’s sarcoma. J Bone Joint Surg Br 81:317–322
van der Woude HJ, Bloem JL, Holscher HC, et al (1994) Monitoring the effect of chemotherapy in Ewing’s sarcoma of bone with MR imaging. Skeletal Radiol 23:493–500
Reddick WE, Bhargava R, Taylor JS, et al (1995) Dynamic contrast-enhanced MR imaging evaluation of osteosarcoma response to neoadjuvant chemotherapy. J Magn Reson Imaging 5:689–694
Verstraete KL, Van der Woude HJ, Hogendoorn PC, et al (1996) Dynamic contrast-enhanced MR imaging of musculoskeletal tumors: basic principles and clinical applications. J Magn Reson Imaging 6:311–321
van der Woude HJ, Verstraete KL, Hogendoorn PC, et al (1998) Musculoskeletal tumors: does fast dynamic contrast-enhanced subtraction MR imaging contribute to the characterization? Radiology 208:821–828
Reddick WE, Taylor JS, Fletcher BD (1999) Dynamic MR imaging (DEMRI) of microcirculation in bone sarcoma. J Magn Reson Imaging 10:277–285
Lang P, Honda G, Roberts T, et al (1995) Musculoskeletal neoplasm: perineoplastic edema versus tumor on dynamic postcontrast MR images with spatial mapping of instantaneous enhancement rates. Radiology 197:831–839
van der Woude HJ, Bloem JL, Verstraete KL, et al (1995) Osteosarcoma and Ewing’s sarcoma after neoadjuvant chemotherapy: value of dynamic MR imaging in detecting viable tumor before surgery. AJR 165:593–598
Erlemann R, Reiser MF, Peters PE, et al (1989) Musculoskeletal neoplasms: static and dynamic Gd-DTPA-enhanced MR imaging. Radiology 171:767–773
Dyke JP, Panicek DM, Healey JH, et al (2003) Osteogenic and Ewing sarcomas: estimation of necrotic fraction during induction chemotherapy with dynamic contrast-enhanced MR imaging. Radiology 228:271–278
Egmont-Petersen M, Hogendoorn PC, van der Geest RJ, et al (2000) Detection of areas with viable remnant tumor in postchemotherapy patients with Ewing’s sarcoma by dynamic contrast-enhanced MRI using pharmacokinetic modelling. Magn Reson Imaging 18:525–535
Reddick WE, Wang S, Xiong X, et al (2001) Dynamic magnetic resonance imaging of regional contrast access as an additional prognostic factor in pediatric osteosarcoma. Cancer 91:2230–2237
Ongolo-Zogo P, Thiesse P, Sau J, et al (1999) Assessment of osteosarcoma response to neoadjuvant chemotherapy: comparative usefulness of dynamic gadolinium-enhanced spin-echo magnetic resonance imaging and technetium-99 m skeletal angioscintigraphy. Eur Radiol 9:907–914
Baur A, Stabler A, Bruning R, et al (1998) Diffusion-weighted MR imaging of bone marrow: differentiation of benign versus pathologic compression fractures. Radiology 207:349–356
Lang P, Wendland MF, Saeed M, et al (1998) Osteogenic sarcoma: noninvasive in vivo assessment of tumor necrosis with diffusion-weighted MR imaging. Radiology 206:227–235
Zhou XJ, Leeds NE, McKinnon GC, et al (2002) Characterization of benign and metastatic vertebral compression fractures with quantitative diffusion MR imaging. AJNR 23:165–170
Edeline V, Frouin F, Bazin JP, et al (1993) Factor analysis as a means of determining response to chemotherapy in patients with osteogenic sarcoma. Eur J Nucl Med 20:1175–1185
van der Woude HJ, Bloem JL, Schipper J, et al (1994) Changes in tumor perfusion induced by chemotherapy in bone sarcomas: color Doppler flow imaging compared with contrast-enhanced MR imaging and three-phase bone scintigraphy. Radiology 191:421–431
Provisor AJ, Ettinger LJ, Nachman JB, et al (1997) Treatment of nonmetastatic osteosarcoma of the extremity with preoperative and postoperative chemotherapy: a report from the Children’s Cancer Group. J Clin Oncol 15:76–84
Schulte M, Brecht-Krauss D, Werner M, et al (1999) Evaluation of neoadjuvant therapy response of osteogenic sarcoma using FDG PET. J Nucl Med 40:1637–1643
Franzius C, Sciuk J, Brinkschmidt C, et al (2000) Evaluation of chemotherapy response in primary bone tumors with F-18 FDG positron emission tomography compared with histologically assessed tumor necrosis. Clin Nucl Med 25:874–881
Hawkins DS, Rajendran JG, Conrad EU III, et al (2002) Evaluation of chemotherapy response in pediatric bone sarcomas by [F-18]-fluorodeoxy-D-glucose positron emission tomography. Cancer 94:3277–3284
Franzius C, Bielack S, Flege S, et al (2002) Prognostic significance of (18)F-FDG and (99m)Tc-methylene diphosphonate uptake in primary osteosarcoma. J Nucl Med 43:1012–1017
van der Woude HJ, Bloem JL, van Oostayen JA, et al (1995) Treatment of high-grade bone sarcomas with neoadjuvant chemotherapy: the utility of sequential color Doppler sonography in predicting histopathologic response. AJR 165:125–133
Gillespy T III, Manfrini M, Ruggieri P, et al (1988) Staging of intraosseous extent of osteosarcoma: correlation of preoperative CT and MR imaging with pathologic macroslides. Radiology 167:765–767
Fletcher BD, Wall JE, Hanna SL (1993) Effect of hematopoietic growth factors on MR images of bone marrow in children undergoing chemotherapy. Radiology 189:745–751
Ryan SP, Weinberger E, White KS, et al (1995) MR imaging of bone marrow in children with osteosarcoma: effect of granulocyte colony-stimulating factor. AJR 165:915–920
Fletcher BD (1997) Effects of pediatric cancer therapy on the musculoskeletal system. Pediatr Radiol 27:623–636
Itoh K, Kanegae K, Kato C (1995) Increased symmetric bone uptake during treatment with granulocyte colony stimulating factor and erythropoietin. Clin Nucl Med 20:932–933
Hollinger EF, Alibazoglu H, Ali A, et al (1998) Hematopoietic cytokine-mediated FDG uptake simulates the appearance of diffuse metastatic disease on whole-body PET imaging. Clin Nucl Med 23:93–98
Davies AM, Makwana NK, Grimer RJ, et al (1997) Skip metastases in Ewing’s sarcoma: a report of three cases. Skeletal Radiol 26:379–384
Saifuddin A, Twinn P, Emanuel R, et al (2000) An audit of MRI for bone and soft-tissue tumours performed at referral centres. Clin Radiol 55:537–541
Moore SG, Dawson KL (1990) Red and yellow marrow in the femur: age-related changes in appearance at MR imaging. Radiology 175:219–223
Enneking WF, Kagan A II (1978) Transepiphyseal extension of osteosarcoma: incidence, mechanism, and implications. Cancer 41:1526–1537
Simon MA, Bos GD (1980) Epiphyseal extension of metaphyseal osteosarcoma in skeletally immature individuals. J Bone Joint Surg Am 62:195–204
Norton KI, Hermann G, Abdelwahab IF, et al (1991) Epiphyseal involvement in osteosarcoma. Radiology 180:813–816
Hoffer FA, Nikanorov AY, Reddick WE, et al (2000) Accuracy of MR imaging for detecting epiphyseal extension of osteosarcoma. Pediatr Radiol 30:289–298
San-Julian M, Aquerreta JD, Benito A, et al (1999) Indications for epiphyseal preservation in metaphyseal malignant bone tumors of children: relationship between image methods and histological findings. J Pediatr Orthop 19:543–548
Panuel M, Gentet JC, Scheiner C, et al (1993) Physeal and epiphyseal extent of primary malignant bone tumors in childhood. Correlation of preoperative MRI and the pathologic examination. Pediatr Radiol 23:421–424
Schima W, Amann G, Stiglbauer R, et al (1994) Preoperative staging of osteosarcoma: efficacy of MR imaging in detecting joint involvement. AJR 163:1171–1175
Beltran J, Simon DC, Katz W, et al (1987) Increased MR signal intensity in skeletal muscle adjacent to malignant tumors: pathologic correlation and clinical relevance. Radiology 162:251–255
van Trommel MF, Kroon HM, Bloem JL, et al (1997) MR imaging based strategies in limb salvage surgery for osteosarcoma of the distal femur. Skeletal Radiol 26:636–641
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brisse, H., Ollivier, L., Edeline, V. et al. Imaging of malignant tumours of the long bones in children: monitoring response to neoadjuvant chemotherapy and preoperative assessment. Pediatr Radiol 34, 595–605 (2004). https://doi.org/10.1007/s00247-004-1192-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-004-1192-x