Abstract
Fetus in fetu is an extremely rare entity and refers to the growth of a “parasitic” twin within a more mature fetus due to its inclusion within cells of the blastocyst. The presence of a vertebral column is considered essential for the diagnosis of a fetus in fetu. The retroperitoneum is the most common location for a fetus in fetu and its location in the mouth is rare. We report a case of oropharyngeal mass detected on antenatal sonography with imaging features consistent with a fetus in fetu. Complete surgical removal of the mass was aided by imaging. Follow-up of these patients is recommended to detect the rare incidence of malignant degeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fetus in fetu is a rare entity occurring in approximately 1 per 500,000 births [1] and was described by Meckel at the turn of the nineteenth century [2]. Since then there has been controversy regarding the definition and embryogenesis of fetus in fetu [3, 4]. Most investigators believe it to be a monozygotic parasitic twin growing inside its otherwise normal fellow twin [1]. Some investigators believe it to be a highly organized and well-differentiated teratoma and term it a fetiform teratoma [3]. While a retroperitoneal location is common for fetus in fetu, an oropharyngeal fetus in fetu is extremely rare [5]. We report a case of a huge organoid oropharyngeal mass protruding from the mouth of a premature neonate detected on antenatal sonography and MR imaging. Because of the danger of respiratory embarrassment, the fetus was delivered following intrapartum tracheostomy while the patient was receiving placental blood flow. Postnatal imaging features of the mass were consistent with fetus in fetu; however, on subsequent resection and histological examination it was difficult to definitively distinguish it from a well-differentiated teratoma.
Case report
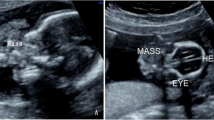
A premature male fetus was delivered at 29.5 weeks’ gestation because of extreme maternal polyhydramnios. The cause of increased amniotic fluid was the fetus’s inability to swallow due to obstruction of the oropharyngeal airway by a large mass that was detected on antenatal ultrasonography and confirmed by MR imaging. An urgent EXIT (ex-utero intrapartum technique) procedure was performed that involved fetal tracheostomy during delivery while the fetus was receiving placental blood. Once adequate airway was secured the fetus was delivered. The baby weighed approximately 1,500 g at birth. An extremely large exophytic mass, larger than the baby’s head, was exiting the oropharynx though a wide-open mouth with two large polyps protruding through the nares (Fig. 1). The mass was lobulated, with external hair and multiple soft tissue polyp-like protuberances reminiscent of digits. The baby was transferred to the neonatal intensive care unit where an intracranial ultrasonography showed grade III germinal matrix hemorrhage.
A 29.5-week premature neonate, on day 3 after urgent EXIT delivery due to giant oropharyngeal fetus in fetu. a Large lobulated mass, larger than the neonate’s head, protrudes from the oral cavity through a stretched open mouth (long thin arrow). Note tracheostomy tube (short thick arrow) placed during delivery. Arrowheads mark polypoidal components of the mass arising from the nares (hidden by the mass on this image). b View of inferior surface of mass and oral cavity shows mass to be arising from the roof of the oral cavity with an intact tongue and floor of mouth. Large, discolored and ulcerated component of mass (arrows) is visible along its inferior surface
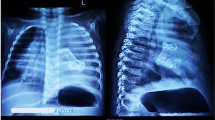
The following day a CT scan of the head and face was performed to assess the extent of the oropharyngeal mass. CT confirmed the clinical findings of a large, heterogeneously enhancing mass arising from the hard palate extending into the oropharyngeal and nasal cavities with no evidence of intracranial extension. Ossified bone was visible on CT resembling vertebrae, ribs and limbs (Fig. 2) consistent with the diagnosis of fetus in fetu. Due to the complex clinical management that included significant fluid losses, ulceration of the mass and progressive platelet consumption, the baby was operated on day 3 following birth. A debulking procedure was performed—the exophytic component of the mass was transected at its junction with the hard palate. The nasal polypoid segments of the mass were also resected and the patient returned to the neonatal intensive care unit.
Contrast-enhanced CT scan of the oropharyngeal mass. a Coronal CT of oropharyngeal mass shows a large heterogeneously enhancing mass (thick arrows) centered on the hard palate extending superiorly and inferiorly into nasal and oral cavities, respectively; note intracranial hemorrhage (thin arrow). Bony components are marked with an arrowhead. b Axial section through the mass demonstrated bony components resembling cervical vertebrae (long arrow), ribs (arrowhead) and limbs (not shown). Presence of vertebrae supports diagnosis of fetus in fetu
The resected lobulated mass weighed 371 g and measured 16.0×12.5×6.0 cm. The mass appeared to be covered entirely by skin except at the resected margins. The lobules in the mass measured 6.0 cm in the greatest dimension with gross areas of adipose tissue, cystic spaces containing clear yellow fluid, bony and cartilaginous tissue. The polyps in the nasal cavities that were a part of the mass measured 2.4×1.6×0.7 cm and 3.0×1.6×0.6 cm. Microscopically, the entire mass had a portion of skin along with predominantly neuroepithelial elements and focal areas showing mature brain tissue. Also identified were hepatoid elements, respiratory-type and intestinal-type epithelium, islands of pancreatic tissue, immature and mature cartilage, bony tissue including bone marrow elements in bony trabeculae, tooth, salivary gland structures and squamous epithelium containing hair shafts. The mass also contained elements suggestive of yolk-sac carcinoma.
Because there was concern of yolk-sac carcinoma, the residual mass (Fig. 3) along the hard palate was completely excised at a second stage resection at approximately 2 weeks of age. Microscopic examination showed the skin with adenexa, adipose tissue, serous glands, cartilage, bone, tooth, glial tissue and pigmented retinal epithelial. No immature or yolk-sac elements were present. The alpha-fetoprotein level 1 week after the second surgery was 19,814 ng/ml (normal <170,000 ng/ml). The microscopic examination of the mass demonstrating differentiation into fetal elements, together with the CT demonstration of portions of ossified skeleton, especially the spine, is consistent with fetus in fetu.
Discussion
Fetus in fetu is an extremely rare entity having an incidence of 1 per 500,000 births [1]. It refers to the development of a parasitic twin in the body of its partner due to early inclusion of totipotent cells of the blastocyst in the more mature growing embryo [1, 3]. Most authors consider fetus in fetu to be a form of a monozygotic, monochorionic and diamniotic pregnancy [1], although some authors support the theory that it represents a highly organized and well-differentiated teratoma and term it “fetiform teratoma” [3]. The former hypothesis that fetus in fetu is distinct from a teratoma is supported by the fact that as compared to a teratoma, malignant degeneration of fetus in fetu is extremely rare [6] and fetus in fetu most commonly occurs in the upper retroperitoneum whereas teratoma most frequently occurs in the pelvis. Rarely, teratoma and fetus in fetu may coexist in the same patient [7].
There is also confusion regarding the diagnostic criteria for fetus in fetu—while most investigators emphasize the presence of a clearly identifiable vertebral column (reflecting that during embryological development such a twin must pass through the primitive streak stage) necessary for the diagnosis of fetus in fetu [4], others believe that the presence of a vertebral column is not essential for the diagnosis of fetus in fetu [8]. Hoeffel et al. [1] reviewed the literature and found that in 9% of cases of fetus in fetu there was no vertebral column even on pathologic examination. In our case, although no vertebral column was found at pathology, resemblance of the bony components of the mass to the vertebral column on imaging (Fig. 2), with attempt at formation of a cervical spine, is highly suggestive of fetus in fetu. Potter [9] described fetus in fetu as representing a part of a continuum of the twinning process with normal twins at one end of the spectrum and immature teratomas with malignant potential at the other end, with conjoined twins, fetus in fetu and fetal inclusions somewhere in between.
While most living cases of fetus in fetu are children presenting before the age of 2 years [1] this entity has also been reported in adults [10]. These masses are frequently discovered antenatally on routine obstetric ultrasound, especially if they arise outside the abdomen as in our case. However, the specific diagnosis of fetus in fetu antenatally is difficult to make and it may be impossible to distinguish them from teratomas, since both appear as soft-tissue masses with calcifications [2]. Neither is any laboratory test available to distinguish between these two entities—alpha-fetoprotein levels are normal in fetus in fetu, elevated in only 50% of immature teratomas and 6% of mature teratomas [11]. Computed tomography or even MR imaging may be necessary to diagnose this entity postnatally [8]. The most frequent location of fetus in fetu is the retroperitoneum (80%), followed in frequency by intracranial or sacral locations, with the scrotum and mouth (epignathus is a term used to define teratomas arising from the oropharynx) being the least common [1]. The clinical presentation depends on the site of the tumor and therefore 70% these cases present with abdominal masses [1]. Our patient had compromise of the airway due to the large size of the tumor and underwent tracheostomy during the delivery prior to transection of the umbilical cord. The number of parasitic fetuses is usually single (88%) with a range of 2–5 [1]. The fetus is always anencephalic, with the vertebral column and limbs present in 91% and 82.5% of cases respectively; central nervous system, gastrointestinal, vascular and genitourinary tract components are found less commonly and the heart is rarely present [1]. A retroperitoneal fetus in fetu may derive blood supply from a major abdominal artery with an identifiable umbilical vessel [2]. No such vascular supply to the fetus in fetu was seen in our case.
The treatment of fetus in fetu is complete surgical removal of the mass as soon as possible. Various complications have been reported such as growth of the mass [2], hemorrhage, intestinal obstruction [2], raised intracranial pressure [12] and malignant degeneration or recurrence [6]. Because of the risk of malignant degeneration it is recommended that alpha-fetoprotein levels be monitored in all cases especially if immature tissue is found on pathologic examination or if resection of the mass is incomplete [2].
In conclusion, fetus in fetu is a rare entity. An abdominal mass in a child less than 2 years of age is the most common presentation due to the retroperitoneal location of this entity. The origin of a fetus in fetu from the mouth is rare and imaging may aid in the differentiation of these masses from an epignathus (oropharyngeal teratoma) by demonstration of spinal components. However, clinically, differentiation between fetus in fetu and epignathus is of limited value since management of both entities is complete surgical removal with follow-up by monitoring of alpha-fetoprotein levels to detect malignant degeneration.
References
Hoeffel CC, Nguyen KQ, Phan HT, et al (2000) Fetus-in-fetu: a case report and literature review. Pediatrics 105:1335–1344
Nastanski F, Downey EC (2001) Fetus in fetu: a rare cause of a neonatal mass. Ultrasound Obstet Gynecol 18:72–75
Heifetz SA, Alrabeeah A, Brown BS, et al (1998) Fetus in fetu: a fetiform teratoma. Pediatr Pathol 8:215–226
Willis RA (1935) The structure of a teratoma. J Pathol Bacteriol 40:1–36
Senyuz OF, Rizalar R, Celayir S, et al (1992) Fetus in fetu or giant epignathus protruding from the mouth. J Pediatr Surg 27:1493–1495
Hopkins KL, Dickson PK, Ball TI, et al (1997) Fetus in fetu with malignant recurrence. J Pediatr Surg 32:1476–1479
Du Plessis JPG, Winship WS, Kirstein JDL (1974) Fetus in fetu and teratoma: a case report and review. S Afr Med J 48:2119–2122
Fink AM, Cuckow PM, Scott R (1995) Case report: fetus-in-fetu—imaging, surgical and pathological findings. Clin Radiol 50:274–275
Potter EL (1962) Pathology of the fetus and the new born, 2nd edn. Year Book Publishers, Chicago, pp 183–187
Dagradi AD, Mangiante GL, Serio GE, et al (1992) Fetus in fetu removal in a 47-year-old man. Surgery 112:598–602
Tsuchida Y, Hasegawa H (1983) The diagnostic value of alpha-fetoprotein in infants and children with teratomas: a questionnaire survey in Japan. J Pediatr Surg 18:152–155
Yang ST, Leow SW (1992) Intracranial fetus in fetu: CT diagnosis. AJNR 13:1326–1329
Acknowledgement
We would like to thank the parents of the patient for kindly allowing us to publish this educational manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kapoor, V., Flom, L. & Fitz, C.R. Oropharyngeal fetus in fetu. Pediatr Radiol 34, 488–491 (2004). https://doi.org/10.1007/s00247-003-1103-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-003-1103-6