Abstract
Background
Pulmonary venous (PV) obstruction may complicate surgical repair of PV abnormalities. By combining phase-contrast cine (PC) imaging and contrast-enhanced angiography, magnetic resonance (MR) imaging can provide physiological information complementing anatomical diagnosis.
Objectives
To compare the PV flow pattern observed after surgical repair of PV abnormalities with normal PV flow pattern and to investigate the changes occurring in the presence of PV stenosis by using PC MR in children.
Materials and methods
By using PC MR, PV flow was evaluated in 14 patients (3 months-14 years) who underwent surgical repair for PV abnormalities. Eleven children (8–18 years) were studied as normal controls. Peak flow velocities and patterns were compared among three groups: normal veins (n=23), surgically repaired veins without (n=44) and with stenosis (n=10).
Results
Normal and unobstructed pulmonary veins after surgery showed a biphasic or triphasic flow pattern with one or two systolic peaks and a diastolic peak. Unobstructed surgically repaired veins showed decreased peak systolic velocity (P =0.001) and an increased peak diastolic velocity (P=0.005) when compared to normal values. Obstructed veins showed decreased systolic and diastolic velocities when measured upstream from the stenosis.
Conclusion
PC MR shows different flow patterns among normal, surgically repaired pulmonary veins with and without stenosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stenosis of the individual pulmonary veins is rarely a primary condition [1, 2], but it occurs more often after surgical repair of anomalous pulmonary venous (PV) connections [2, 3, 4]. It is important to recognize this condition as early as possible because severe stenosis can be lethal. Echocardiography with color and spectral Doppler interrogation has been used as the primary diagnostic method in the preoperative and postoperative evaluation of PV abnormalities with or without obstruction [5, 6, 7, 8]. However, echocardiography is limited in its visualization of the pulmonary veins within the aerated lungs and in Doppler quantification of the severity of stenosis [5, 6]. In contrast, magnetic resonance (MR) is able to visualize the pulmonary veins along their entire course through the lungs as well as in the mediastinum [9, 10, 11]. Contrast-enhanced MR angiography in particular has been recognized as the fastest and most accurate diagnostic tool for anatomical evaluation of the pulmonary veins [12, 13]. With its excellent anatomical imaging capability, MR could be used as the primary diagnostic tool for the evaluation of PV abnormalities if additional haemodynamic information could also be provided.
Phase-contrast cine (PC) MR is an established technique for the evaluation of velocity, volume and pattern of blood flow [14, 15, 16, 17, 18, 19, 20, 21, 22, 23]. PC MR is advantageous over Doppler ultrasound techniques in at least two respects. Firstly, PC MR provides the flow information from the entire cross-sectional area of the target vessel, enabling calculation of the average flow velocity and therefore the flow volume. Secondly, as PC MR imaging is not compromised by the presence of air, bone or surgical scar, any vessel in any anatomical location and orientation can be imaged in a desired plane, which for accurate measurement of velocity should be parallel or perpendicular to the vessel. The latter advantage of PC MR is particularly important in the evaluation of the pulmonary arteries and veins within the lungs. Despite these clear advantages, however, PC MR remains underutilized for the evaluation of PV pathology with only a few reports having described its application in adults [16, 24] and children [25].
The aim of our study was to compare the PV flow pattern observed after surgical repair of PV abnormalities with normal PV flow pattern and to investigate the changes occurring in presence of PV stenosis by using PC MR in children.
Materials and methods
Patient population
Patients undergoing cardiac MR for anatomical evaluation of the pulmonary veins after surgical repair of PV abnormalities were prospectively enrolled in this study. Patients with additional lesions that might influence PV blood flow pattern, such as more than trivial regurgitation of the atrioventricular valve, systolic or diastolic ventricular dysfunction and branch pulmonary artery stenosis detected by echocardiography, were excluded. Thus 14 patients, 3 months to 14 years of age, with a median of 30 months and weighing 3.3–62 kg with a median of 13 kg, underwent cardiac MR for evaluation of the results of surgical repair of PV abnormalities. Surgery was performed for repair of total anomalous PV connection in 12, of partial anomalous PV connection in 1, and of native pulmonary vein stenosis in 1 patient. The time interval between surgery and the MR study ranged from 10 days to 14 years with a median interval of 30 months. Associated cardiac anomalies were present in three patients: a ventricular septal defect in one and right isomerism in two. In one patient the ventricular septal defect was closed at the time of surgical PV repair. The two patients with right atrial isomerism underwent palliation with a Blalock-Taussig shunt and a bidirectional cavopulmonary connection, respectively, simultaneously with the PV repair.
During the same period, 11 patients without cardiac abnormality were recruited as normal control subjects. The primary indications for cardiac MR in these patients included suspected arrhythmogenic right ventricular dysplasia in eight, suspected partial anomalous pulmonary venous connection in one, suspected residual atrial septal defect in one and a mild form of Marfan syndrome in one patient. The patients were 8 −18 years of age with a median of 16 years and weighed 26–82 kg with a median of 56 kg. None of these children had a previous surgical atriotomy, evidence of systolic or diastolic ventricular dysfunction, valvular disease, left ventricular outflow tract obstruction, abnormal pulmonary blood flow distribution or an intracardiac shunt.
The study was approved by the Research Ethics Board of our institution. Written informed consent was obtained from the parents. Written assent was obtained from the patient when possible.
MR technique
MR imaging was performed with a 1.5-T System (Signa CVMR; General Electric Medical Systems, Milwaukee, Wisc.). The patients were scanned in a phased-array cardiac or head coil, depending on their body size. The MR imaging protocol included: contrast-enhanced angiography as described elsewhere [13], cine MR using a fast gradient-echo sequence to assess ventricular function, and PC MR to measure blood flow velocity and profile in the pulmonary veins and arteries.
The parameters of the PC MR were: minimum TE and TR, flip angle 20°, matrix 256×128, views per segment 1, number of excitations 2, number of phases in a cardiac cycle 20, slice thickness 4 mm. Retrospective electrocardiographic gating was used. Starting with a minimal velocity of 100 cm/s, the upper-velocity range was set at least 25% higher than the expected peak velocity, suggested by echocardiography, in order to optimize measurement accuracy while avoiding aliasing. The imaging plane perpendicular to the axis of the pulmonary vein was chosen from the cine gradient-echo or from the contrast-enhanced angiographic images. When a stenotic lesion was identified, imaging was tailored to target the pulmonary vein upstream from the stenosis. Where possible, PC MR was also performed at the narrowest point.
The study was performed with sedation in six cases and general anaesthesia in six. Two patients required neither sedation nor general anaesthesia. None of the normal control studies was performed under sedation or general anaesthesia.
Data analysis
Based on the findings at contrast-enhanced MR angiography, the PV anatomy was classified into three groups: normal veins (control group), surgically repaired veins without stenosis and surgically repaired veins with stenosis. We defined a vein as stenotic if its diameter was narrowed by more than 25% of the adjacent unobstructed segment of the same vein in form of either discrete or segmental narrowing. A severe stenosis was defined as more than 50% narrowing.
The analysis of the PC data was performed on a separate commercially available workstation (Advantage Windows 3.0; General Electric Medical Systems, Milwaukee, Wisc.) using built-in flow analysis software, by manually tracing the contour of the vessel in each of the acquired 20 phases. We evaluated the PV flow pattern as shown in the velocity-time curves (Fig. 1). According to the number of definable positive peaks in the curve, the flow pattern was described as biphasic, triphasic or continuous. The maximum peak velocities were measured and the ratio between the systolic and diastolic velocities (S/D) was calculated. The presence and timing of the nadir, i.e. the point of lowest flow velocity, were also recorded. The data thus produced were compared for the three groups. We also compared the changes in pulmonary venous flow pattern between the two different surgical procedures used for pulmonary vein repair. The sutureless neoatrium technique reconstructs the pulmonary veins and their connection to the left atrium by using in situ pericardium, while the conventional technique does not use either pericardium or foreign material for repair or augmentation of the pulmonary veins [26]. The choice of the technique was determined by the surgeon's preference and not by the anatomical findings or severity of the lesion.
Phase-contrast MR of normal pulmonary vein. Magnitude (a) and phase-contrast (b) images are obtained in a plane perpendicular to the right lower pulmonary vein (RLPV). The right pulmonary artery (RPA) and its upper branch (RUPA) are included in the imaging plane. c The velocity-time curves for blood flow in the right lower pulmonary vein and right pulmonary artery. The pulmonary venous flow curve consists of two systolic (es and ls) peaks and a diastolic (d) peak with a nadir in the late diastole when the atrium contracts. The diastolic flow peak is slightly higher than the systolic flow peaks. The systolic and diastolic phases are clearly defined in the arterial curve
The PC data from the normal control group were analysed separately by two independent investigators (S.J.Y., E.R.V.), to test the interobserver variability of measurement.
Statistical analysis
Descriptive data are reported as means ± standard deviations or medians and ranges, as appropriate. For comparison between two groups, an unpaired Student's t-test was performed. Welch correction was applied to the t-test when two groups of data showed different standard deviations, even after logarithmic transformation. A P value of less than 0.05 was considered to be statistically significant. Linear regression analysis was performed to determine the dependence of the measurement data on the heart rate and age. Interobserver variability was analysed by calculating the mean difference (bias) and the standard deviation of the difference between the measurements of the two investigators in the normal control group.
Results
PC MR was performed for 23 normal pulmonary veins in the control group and for 50 surgically repaired pulmonary veins. In the study group 44 pulmonary veins did not show any anatomical obstruction, and 10 pulmonary veins were stenotic. PC MR could not be performed in 4 stenotic pulmonary veins.
Normal pulmonary venous flow patterns
The flow pattern was biphasic (n=14) or triphasic (n=9) in all 23 normal control pulmonary veins. The biphasic flow pattern consisted of one peak in the systolic phase and a second peak in the diastolic phase. Triphasic flow consisted of two peaks in the systolic phase and one peak in the diastolic phase (Fig. 1). The nadir of the flow curve was observed in the late diastolic phase corresponding to the atrial contraction in all cases. In 21 of 23 (91%), the nadir was associated with a small amount of reversed flow.
In normal subjects the average peak systolic velocity (S) was slightly higher than the peak diastolic velocity (D), resulting in an S/D ratio of 1.1±0.3 (Table 1). Within the observed heart rate range of 54–90 beats per minute, no correlation was observed between heart rate and any of the following; peak systolic velocity (r=−0.13, P=0.56), peak diastolic velocity (r=−0.32, P=0.13) and S/D ratio (r=0.1, P=0.6). Similarly, no correlation was demonstrated between peak velocities and age.
Excellent agreement in measurement of the peak systolic and diastolic velocities and the velocity at the nadir was found between the two observers (n=23, mean difference =0.08 cm/s, 95% limits of agreement ±5.8 cm/s).
Flow patterns in unobstructed pulmonary veins after surgery
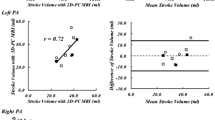
All 44 surgically repaired pulmonary veins without obstruction showed a biphasic or triphasic flow pattern (Fig. 2). However, the mean peak systolic velocity was lower (P=0.001) and the mean peak diastolic velocity was higher (P=0.005) and as a result, the S/D ratio was lower (0.67±0.2, P<0.001) than the velocities in the normal control group (Fig. 2, Table 1).
A 3-month-old girl who underwent surgical repair for native pulmonary vein stenosis. a After surgery, contrast-enhanced MR angiogram shows a patent left upper pulmonary vein (LUPV) but severe segmental hypoplasia of the left middle (LMPV) and the left lower (LLPV) pulmonary veins. b Phase-contrast MR was performed perpendicularly to the LUPV and LMPV. The curve from the unobstructed LUPV shows biphasic flow pattern with decreased systolic peak (s) velocity and increased diastolic peak (d) velocity. Notice that the nadir is in the early systolic phase. The curve from the LMPV upstream from the stenosis shows continuous flow with decreased velocity (LA left atrium)
The nadir of the flow curve was observed in the late diastolic phase in 14 veins (four patients). In 30 veins (ten patients), the nadir was in the early systolic phase (Fig. 2). The nadir was associated with reversed flow in 32 of 44 veins. The peak velocity of the reversed flow was 12.4±6.5 cm/s.
Within the observed heart rate range of 66–157 beats per minute, there was weak inverse correlation between the heart rate and the peak diastolic velocity (r=−0.29, P=0.03). However, there was no correlation between the heart rate and either the peak systolic velocity (r=−0.15, P=0.27) or the S/D ratio (r=0.18, P =0.18). A positive correlation was found between the age and peak systolic velocity (r=0.36, P=0.006). However, there was no correlation between the age and either the peak diastolic velocity (r=0.18, P=0.18) or the S/D ratio (r=0.21, P=0.11).
The peak systolic velocity was significantly lower in the veins that had been reconstructed with the sutureless neoatrium technique (n=21) than in the veins that had been repaired with a conventional technique (n=23) (P=0.002). There was no significant difference in the peak diastolic velocity and the peak velocity of the reversed flow between the two groups.
Flow patterns in obstructed pulmonary veins
PC flow analysis was possible in six of the ten stenotic pulmonary veins. In these six pulmonary veins, stenosis was mild to moderate in four, severe in one and diffuse hypoplasia was present in another one. PC flow analysis could not be performed in four stenotic pulmonary veins; two of them were so severely hypoplastic that they were functional atretic, one vein showed a diameter of only 2.5 mm and in the fourth case the anatomy was so complex that a correct tailoring for the PC images was impossible from the reference angiographic images.
In all four veins with mild-to-moderate stenosis, flow was measured upstream from the stenosis and showed a biphasic pattern with a reduced peak velocity (<45 cm/s). Flow was also measured at the level of stenosis in one of these veins with mild narrowing and in the pulmonary vein with severe stenosis; in both cases we observed still biphasic pattern, but indeed higher peak velocities (>100 cm/s).
The vein with diffuse hypoplasia showed a continuous flow curve with very low velocity, reflecting the small amount of blood flowing through it (Fig. 2).
Discussion
This study compared the blood flow pattern of surgically repaired pulmonary veins with the normal PV flow pattern in children by using PC MR. Our results demonstrate that PC MR enables differentiation of abnormal from normal PV flow pattern and provides preliminary information about the changes in the flow pattern, and therefore about the functional significance of stenotic lesions depicted by contrast-enhanced MR angiography.
Normal pulmonary venous flow pattern
The flow pattern and peak velocities we observed in normal pulmonary veins are similar to those of previous studies that utilized either spectral Doppler echocardiography or PC MR (Table 2). In both techniques, normal PV flow curve consists of one or two systolic peaks and a diastolic peak with the lowest flow velocity (nadir) seen at the end of the ventricular diastole when the atrium contracts [16, 27, 28]. Doppler echocardiographic data from a paediatric population demonstrated an increased peak diastolic velocity with increasing age and a decreased peak diastolic velocity with increasing heart rate [29]. However, the range of the peak velocities observed in normal pulmonary veins was wide, not only among different studies in adults and children, but also among the subjects within each individual study [29, 30]. This heterogeneity may create some difficulties in distinguishing abnormal from normal flow patterns [30]. Unlike other authors [29, 30], we did not find any correlation between peak velocities and either heart rate or age. This may be due to the small study population and the limited ranges of age and heart rate of our normal control group.
Flow patterns in unobstructed pulmonary veins after surgery
The flow pattern we found in surgically repaired pulmonary veins without any anatomical stenosis corresponds to those reported in previous Doppler echocardiographic studies that described a shift of dominant forward flow from systole to diastole in the surgically repaired patients [30, 31]. This shift is considered to reflect the impaired compliance of the left atrium owing to scar formation in the incision site or introduction of new materials in the left atrial wall [26, 32, 33, 34, 35]. In our study, patients who had been operated on with the sutureless neoatrium technique showed lower systolic velocities than those who had undergone a conventional repair. We suppose that with the use of "in situ" pericardium, the sutureless technique may compromise more severely the compliance of the functional neoatrium [3, 26].
In more than half of the surgically repaired pulmonary veins we studied, the nadir of the flow curve was observed in the early systolic phase instead of in the late diastole, indicating that the nadir was not associated with normal atrial contraction. The possibility of error in the timing of the nadir within the cardiac cycle could be excluded by referencing the flow curve of the pulmonary arterial branches or aorta shown in the same PC MR images (Fig. 2). This shift of the nadir into the early systolic phase may be due to impaired left atrial compliance after surgery. At the beginning of ventricular systole, the mitral valve bulges into the left atrium and the left atrial pressure increases. Normally, this pressure change is absorbed by the compliant left atrium and does not propagate into the pulmonary veins. However, if the left atrial compliance is impaired, this pressure might be propagated into the pulmonary veins and cause a decrease in the PV flow or even a short reversal flow in early systole. Alternatively, the nadir can be due to real atrial contraction if an abnormal postoperative cardiac rhythm, i.e. junctional rhythm, is present. We consider the former mechanism as more plausible than the latter since only three of ten patients with a nadir in early systole had a junctional rhythm on electrocardiography. Furthermore, it is unlikely for an abnormal atrial contraction to occur consistently in early systole.
Flow patterns in obstructed veins. Postsurgical PV stenosis usually involves the proximal segment of the vein at its entrance into the left atrium [1, 2]. In real-time echocardiography, the Doppler sampling volume is usually positioned within the left atrium in the post-stenotic jet. As PC MR is not a real-time imaging method, however, it is difficult to target the post-stenotic jet that streams in any direction within the left atrial cavity. Therefore, we routinely examined the pre-stenotic segment, expecting that an abnormal flow pattern would also be seen upstream from the stenosis. Our hypothesis was confirmed and we obtained flow data consistent with those reported in a spectral Doppler echocardiographic study, where Smallhorn et al. described decreased flow velocity if the flow was measured upstream from the stenosis [7].
We were not able to perform PC MR measurements in four of ten stenotic pulmonary veins, either because the vessel size was too small or because the complex tortuous anatomy prevented us from achieving proper targeting. The size of stenotic or hypoplastic pulmonary veins in children may represent a limitation for the clinical applicability of this technique. Indeed, our data, which are based on six pulmonary veins showing different degrees of narrowing, are not enough for defining the typical obstructive flow pattern. Nevertheless, the good correlation between the flow pattern observed by PC MR and the pattern observed by spectral Doppler for the unobstructed veins suggests that the flow pattern measured by PC MR may also be reliable in the presence of stenosis. Further studies in a larger group of patients may validate the reproducibility of our findings. Furthermore, evaluation of the changes in pulmonary arterial blood flow in the central and peripheral branches can provide important additional physiological information, considering that pulmonary arterial blood flow may be redistributed in the presence of PV obstruction. The clinical significance of these blood-flow changes in association with PV obstructions also deserves further investigation. However, in severe stenosis, contrast-enhanced angiography clearly shows on the anatomical images the severe nature of the lesion, even if the flow pattern cannot be analysed.
PC MR
In PC MR, data can be acquired in the direction of blood flow (in-plane measurement) or in a plane perpendicular to the blood-flow direction (through-plane measurement). Kilner et al. [33] demonstrated that velocities up to 6 m/s can accurately be measured by using in-plane PC MR . Videlefsky et al. [25] applied the same method for evaluation of the severity of the pulmonary venous obstruction. In-plane imaging often yields a greater number of voxels for analysis of peak velocity [21]. However, during in-plane imaging, the region of interest can easily move out of plane because of cardiac and respiratory motion, and partial volume effects are larger. This is especially true for small pulmonary veins in children. Moreover, the post-stenotic jet is extremely difficult to target because it streams in any direction within the left atrial cavity. In our experience, through-plane imaging is easier than in-plane imaging for evaluation of the pulmonary veins than for evaluation of larger vessels. Thus, as our results indicate that PV flow upstream from a stenosis might be recognized and distinguished from a normal PV flow, we recommend assessment of PV flow upstream from the narrowest point.
As the PC MR averages the data from many heart beats and respiration cycles, a certain range of difference in measured velocities between PC MR and real-time Doppler ultrasound is inevitable. Thus, we consider the flow pattern more important than the peak velocities when the results of the two diagnostic methods are compared.
In conclusion, PC MR is useful in assessing PV flow pattern in paediatric patients. We demonstrated a difference between the flow pattern in surgically repaired veins and the flow pattern in normal pulmonary veins. In the presence of obstruction, changes in the PV flow pattern could be easily detected when the measurements were performed upstream from the stenosis. Cardiac MR with contrast-enhanced angiography and PC flow mapping enables not only anatomical but also physiological evaluation of the pulmonary veins.
References
Freedom RM, Mawson MB, Yoo SJ, et al (1997) Abnormalities of pulmonary venous connections including subdivided left atrium. In: Congenital heart disease. Textbook of angiocardiography. Futura, Armonk, pp 665–705
Krabill KA, Lucas RV (1990) Congenital cardiac anomalies producing pulmonary venous obstruction (1990). In: Moller JH, Neal WA (eds) Fetal, neonatal, and infant cardiac disease. Appleton & Lange, Norwalk, pp 709–722
Caldarone CA, Najm HK, Smallhorn JF, et al (1998) Relentless pulmonary vein stenosis after repair of total anomalous pulmonary venous drainage. Ann Thorac Surg 66:1514–1520
Hyde JA, Stumper O, Barth MJ, et al (1999) Total anomalous pulmonary venous connection: outcome of surgical correction and management of recurrent venous obstruction. Eur J Cardiothorac Surg 15:735–740
Smallhorn JF, Freedom RM (1986) Pulsed Doppler echocardiography in the preoperative evaluation of total anomalous pulmonary venous connection. J Am Coll Cardiol 8:1413–1420
Smallhorn JF, Burrows P, Wilson G, et al (1987). Two-dimensional and pulsed Doppler echocardiography in the postoperative evaluation of total anomalous pulmonary venous connection. Circulation 76:298–305
Smallhorn JF, Pauperio H, Benson L, et al (1985) Pulsed Doppler assessment of pulmonary vein obstruction. Am Heart J 110:483–486
Obeid AI, Carlson RJ (1995) Evaluation of pulmonary vein stenosis by transoesophageal echocardiography. J Am Soc Echocardiogr 8:888–896
White CS (2000) MR Imaging of thoracic veins. MRI Clin North Am 8:17–32
Ferrari VA, Scott CH, Holland GA, et al (2001) Ultrafast three-dimensional contrast-enhanced magnetic resonance angiography and imaging in the diagnosis of partial anomalous pulmonary venous drainage. J Am Coll Cardiol 37:1120–1128
Choe YH, Lee HJ, Kim HS, et al (1994) MRI of total anomalous pulmonary venous connection. J Comput Assist Tomogr 18:243–249
Greil G, Powell AJ, Gildein HP, et al (2002) Gadolinium-enhanced three-dimensional MR angiography of pulmonary and systemic venous anomalies. J Am Coll Cardiol 39:335–341
Valsangiacomo ER, Levasseur S, McCrindle BW, et al (2003) Contrast-enhanced MR angiography of pulmonary venous abnormalities in children. Pediatr Radiol 33:92–98
Meier D, Maier S, Boesiger P (1988) Quantitative flow measurements on phantoms and on blood vessels with MR. Magn Reson Med 8:25–34
Van Rossum AC, Sprenger M, Visser FC, et al (1991) An in vivo validation of quantitative blood flow imaging in arteries and veins using magnetic resonance phase-shift techniques. Eur Heart J 12:117–126
Mohiaddin RH, Amanuma M, Kilner PJ, et al (1991) MR phase-shift velocity mapping of mitral and pulmonary venous flow. J Comput Assist Tomogr 15:237–243
Mostbeck GH, Caputo GR, Higgins CB (1992) MR measurement of blood flow in the cardiovascular system. AJR 159:453–461
Rebergen SA, van der Wall EE, Doornbos J, et al (1993) Magnetic resonance measurement of velocity and flow: technique, validation and cardiovascular applications. Am Heart J 126:1439–1456
Lee VS, Spritzer CE, Carroll BA, et al (1997) Flow quantification using fast cine phase-contrast MR imaging, conventional cine phase-contrast MR imaging, and Doppler sonography: in vitro and in vivo validation. AJR 169:1125–1131
Mohiaddin RH, Pennell DJ (1998) MR blood flow measurement. Cardiol Clin 16:161 –178
Powell AJ, Maier SE, Chung T, et al (2000) Phase-velocity cine magnetic resonance imaging measurement of pulsatile blood flow velocity in children and young adults: in vitro and in vivo validation. Pediatr Cardiol 21:104–110
Papaharilaou Y, Doorly DJ, Sherwin SJ (2001) Assessing the accuracy of two-dimensional phase contrast MRI measurements of complex unsteady flows. J Magn Reson Imaging 14:714–723
Greil G, Geva T, Maier SE, et al (2002). Effect of acquisition parameters on the accuracy of velocity encoded cine magnetic resonance imaging blood flow measurements. J Magn Reson Imaging 15:47–54
Galjee MA, Van Rossum AC, van Eenige MJ, et al (1995) Magnetic resonance imaging of the pulmonary venous flow pattern in mitral regurgitation. Indipendence of the investigated vein. Eur Heart J 16:1675–1685
Videlefsky N, Parks WJ, Oshinski J, et al (2001) Magnetic resonance phase-shift velocity mapping in pediatric patients with pulmonary venous obstruction. J Am Coll Cardiol 38:262–267
Najm HK, Caldarone CA, Smallhorn JF, et al (1998) A sutureless technique for the relief of pulmonary vein stenosis with the use of in situ pericardium. J Thorac Cardiovasc Surg 115:468–470
Keren G, Sherez J, Megidish R, et al (1985) Pulmonary venous flow pattern—its relationship to cardiac dynamics. A pulsed Doppler echocardiographic study. Circulation 71:1105–1112
Smallhorn JF, Freedom RM, Olley PM (1987) Pulsed Doppler echocardiographic assessment of extraparenchymal pulmonary vein flow. J Am Coll Cardiol 9:573–579
Abdurrahman L, Hoit BD, Banerjee A, et al (1998) Pulmonary venous flow Doppler velocities in children. J Am Soc Echocardiogr 11:132–137
DeMarchi SF, Bodenmueller M, Lai DL, Seiler C (2001) Pulmonary venous flow velocity pattern in 404 individuals without cardiovascular disease. Heart 85:23–29
Minich LA, Tani LY, Hawkins JA, et al (1995) Abnormal Doppler pulmonary venous flow patterns in children after repaired total anomalous pulmonary venous connection. Am J Cardiol 75:606–610
Smallhorn JF, Gow R, Freedom RM, et al (1986) Pulsed Doppler echocardiographic assessment of the pulmonary venous pathway after the Mustard or Senning procedure for transposition of the great arteries. Circulation 73:765–774
Kilner PJ, Firmin DN, Rees RS, et al (1991) Valve and great vessel stenosis: assessment with MR jet velocity mapping. Radiology 178:229–235
Masuyama T, Lee JM, Tamai M, et al (1991) Pulmonary venous flow velocity pattern as assessed with transthoracic pulsed Doppler echocardiography in subjects without cardiac disease. Am J Cardiol 67:1396–1404
Klein AL, Burstow DJ, Tajik AJ, et al (1994) Effects of age on left ventricular dimensions and filling dynamics in 117 normal persons. Mayo Clin Proc 69:212–224
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Valsangiacomo, E.R., Barrea, C., Macgowan, C.K. et al. Phase-contrast MR assessment of pulmonary venous blood flow in children with surgically repaired pulmonary veins. Pediatr Radiol 33, 607–613 (2003). https://doi.org/10.1007/s00247-003-0983-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-003-0983-9