Abstract
Critical hypoxemia soon after birth is the most critical preoperative determinant of neurological outcomes and survival in newborns with Dextro Transposition of the Great Arteries and Intact Ventricular Septum (D-TGAIVS). Our study aimed to define fetal echocardiographic aspects that can better predict neonates with D-TGAIVS at risk for restricted interatrial communication after birth. 31 fetuses with a prenatal diagnosis of D-TGAIVS were included in our study. We divided patients with D-TGAIVS according to the timing of balloon atrial septostomy: Urgent, Not-Urgent and no BAS. We identified five fetal echocardiographic aspects of the interatrial septum (redundant, aneurysmal, flat, fixed, hypermobile). No significant differences in these fetal echocardiographic features were found between the three different groups of D-TGAIVS according to the timing of balloon atrial septostmy. However, only two patients showed flat appearance of interatrial communication: both needed Urgent balloon atrial septostomy. The prevalence of hypermobile septum primum was significantly lower in the control group compared to patients with D-TGAIVS. Fetal echocardiographic aspects cannot predict patients with D-TGAIVS who will not need Urgent balloon atrial septostomy. Therefore, we recommended a delivery in a tertiary center, equipped for Urgent balloon atrial septostomy, for all patients with D-TGAIVS regardless of fetal echocardiographic features.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prenatal diagnosis of Dextro-Transposition of the Great Arteries (D-TGA) allows delivery planning, so that a balloon atrial septostomy (BAS) could be performed if needed without delay soon after birth. Predicting patients who will need an urgent BAS may allow better resource utilization in D-TGAIVS. The arterial switch and the improvement in postoperative management dramatically increased the survival rate of patients with D-TGA. Nevertheless, the first hours after delivery remain crucial, because severe cyanosis and hypoxemia can impact the neurological outcomes of these neonates [1,2,3,4,5].
Immediately after birth, a restricted interatrial septum communication with or without a small patent ductus arteriosus is the most critical determinant of neurological outcome and survival in newborns with D-TGA with Intact Ventricular Septum (D-TGAIVS) [6,7,8].
There is limited data on fetal predictors for inadequate circulatory mixing in newborns with D-TGAIVS resulting in critical hypoxia. Nevertheless, it still remains challenging to assess which fetal echocardiographic features can help the identification of those patients who will need a BAS immediately after birth [6, 7, 9,10,11,12].
Therefore, our study aimed to discriminate which fetal echocardiographic aspects can better predict, alone or in combination, those neonates with D-TGAIVS at risk for critical hypoxemia soon after birth that will require an urgent BAS.
Material and Methods
Study Design
Since October 2017, The Bambino Gesù Children's Hospital (BGCH) of Rome, Italy, has started a collaboration (“Progetto Nascita OPBG”) with the Obstetrics Department of San Pietro-Hospital of Rome, for the delivery in the operating room of BGCH of those patients at risk of death or major neurological complications immediately after birth. Patients with fetal diagnosis of D-TGAIVS constitute the most represented cohort in this group. The study was approved by the institutional review board and the need for consent was waived due to the retrospective nature of the study.
Patients and Delivery Procedure
From October 2017 to September 2020, 35 consecutive fetuses with a prenatal diagnosis of D-TGAIVS were identified. From Xcelera viewing platform (Philips Medical Systems, Andover, MA) and clinical database (Intranet Obg Clinico), we reviewed clinical reports, fetal and neonatal echocardiographic images and videos of all patients affected by D-TGAIVS. Inclusion criteria were: confirmed diagnosis of D-TGAIVS, absence of associated major cardiac anomalies, rather than atrial septal defects and small restrictive ventricular septal defects, and delivery in our institution. Thirty-one patients met inclusion criteria and were included in our study. Two patients were excluded due to the presence of major associated cardiac anomalies (aortic coartation). In addition, one patient was excluded because the delivery took place in an emergency situation at another hospital. Furthermore, we did not have sufficient echocardiographic data for another patient due to the unsuitable acoustic window during the examinations.
The control group consisted of 21 normal fetuses at different gestational ages (mean 28.5 ± 4.3) who were free from frequent atrial ectopic beats at the time of the exam.
The obstetricians performed a cesarian section in our cardiac operating room, then, the newborn was immediately transferred to the cardiac catheterization laboratory (Cath Lab), where a team composed of a neonatologist, a perinatal cardiologist and a pediatric anesthesiologist, was in charge of immediate evaluation and management. Echocardiography, catheterization equipment and prostaglandin E1 were available in the Cath Lab. Prostaglandin E1 infusion was started in all patients immediately after umbilical venous catheter placement in the Cath Lab.
Balloon Atrial Septostomy (BAS)
After clinical and echocardiographic evaluation, BAS was performed in those newborns with severe hypoxemia. After evaluation and/or BAS the neonates were moved to the Cardiac Intensive Care Unit (CICU). After delivery, the mother returned to the referral center.
The decision to perform an urgent BAS (UBAS) within the first 60 min after delivery was based on the patient clinical conditions and the postnatal assessment of the foramen ovale. After patient stabilization, an oxygen saturation < 70% and/or a restricted foramen ovale (diameter < 3 mm and color flow aliasing) were considered indications for UBAS. If the baby does not require UBAS they were transferred to the CICU and monitored. If desaturation develops they underwent a non-urgent BAS. Otherwise, they underwent an elective arterial switch operation.
Fetal Echocardiographic Features
Fetal echocardiography was performed by a transabdominal approach using a pulsed and color Doppler ultrasound (Philips EPIQ CVx, with various probes: Philips C9-2 broadband curved array transducer with PureWave crystal technology, and Philips X5-1 matrix array phased array ultrasound probe transducer), and measurements were performed offline on an Xcelera viewing platform (Philips Medical Systems, Andover, MA). Gestational age was determined by the last menstruation date.
The fetal measurements were performed by an operator (MM) without knowledge of the postnatal outcome, and repeatability was assessed apart by another operator (AT) but at the same clip.
The foramen ovale (FO) length and total septal length (TSL) were measured retrospectively in a 4-chamber view of the heart. The TSL was measured from the atrial septal infold at the most posterior wall of the atrium at the level of the mitral valve, and the FO length was measured in the same frame from effective interatrial communication measuring the color Doppler jet width passing through the redundant septum primum (functional measurement) rather than at the level of the fossa ovale (anatomical measurement). Additionally, we calculated the ratio of Foramen Ovale/TSL (PFO/TSL).
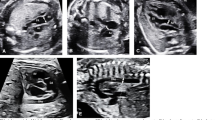
We also identified the foramen ovale characteristics (Fig. 1):
-
Redundant septum primum defined as septum primum herniating more than 50% beyond the plane of the septum secundum across the length of the left atrium [13]—Video 1;
-
Fixed atrial septum defined as an angle between the septum primum and secundum of less than 30° [13]—Video 2;
-
Flat atrial septum: lack of mobility of the atrial septum [13]—Video 3;
-
Hypermobile atrial septum primum: septum primum oscillating between the left and the right atrium [13]—Video 1;
-
Aneurysmal septum primum: defined as the flap valve having a sail in the wind, with a dome shape appearance and is deviated into the left atrium [13]—Fig. 1D.
A Redundant Septum Primum, septum primum herniating more than 50% beyond the plane of the septum secundum across the length of the left atrium as shown by blue dashed line devide left atrium in 4 quadrants. B Fixed Septum Primum: an angle between the septum primum and secundum of less than 30°; blue lines form less than 30°. C Flat Septum Primum: lack of mobility of the atrial septum. D Aneurysmal Septum Primum: defined as the flap valve having a sail in the wind, with a dome shape appearance and is deviated into the left atrium
We analyzed the septum primum characteristics and dimensions at three occasions. At first examination between the 19th and the 32nd weeks of gestational age. We repeated the evaluation between 32nd and the 37th weeks of gestational age.
Finally, all patients with D-TGAIVS had an echocardiogram just before the delivery.
Where possible, we evaluated pulmonary veins mean and maximum velocities in patients with D-TGAIVS and we stratified those values for different BAS groups and for gestational age.
Statistical Analysis
We carried out uni- and multivariable logistic regression analyses to explore the relationship between potential prenatal predictors and the need for an UBAS.
In the univariable analysis categorical variables are expressed in frequency and percentage while the continuous variables are described as mean with standard deviation (SD) and median with range. To identify the differences in the three groups based on the need for BAS, we used chi-squared test for categorical variables and the non-parametric Kruskal–Wallis test for continuous variables.
To compare fetal echocardiographic parameters in the first and second exam and with the first and second operator (paired data) we performed non-parametric Wilcoxon’s rank-sum test for continuous variables and McNemar’s test for categorical variables.
Bland–Altman analysis was used to assess the reliability of paired echocardiographic measurements obtained from the first and the second operator.
Finally, in the multivariable analysis, we used a logistic regression (outcome: BAS vs no BAS) to obtain adjusted Odds Ratio (OR) and 95% confidence intervals (CIs). Results were considered statistically significant at two-tailed p < 0.05.
Data analysis was carried out with STATA 14.0 SE (Stata Corporation, College Station, Texas).
Results
The mean gestational age at the time of the first fetal echocardiogram was 25.5 weeks (range 20.9–30.1) in the D-TGAIVS group (Table 1) and 28.5 weeks (mean 28.2—range 21.6–35.3) in the control group. Fifteen neonates (48.4%) with D-TGAIVS underwent an UBAS. Additionally, a non-urgent BAS was performed in 12 (38.7%), and in the remaining 4 cases (12.1%) BAS was not performed. The UBAS was performed at a mean time after delivery of 43.9 ± 11.4 min. The non-urgent BAS was performed at a mean time after delivery of 15.7 ± 28 h. After initial stabilization, the mean transcutaneous preductal oxygen saturations in patients with D-TGAIVS was 67%. In the UBAS group mean saturation was 57.0% (SD 13.25—range 43.75–70.25) compared to 81% (SD 6.83—range 74.2–87.83) in the rest of the group.
UBAS and Fetal Echocardiography Features
Fixed septum primum was found in 5 patients, 3 of whom in the group of UBAS; other 2 in non-urgent BAS group. None of the patients who didn’t require BAS showed fixed septum primum. No statistically significant difference was found between these groups (p = 0.62) in fixed septum primum.
There was no difference in the prevalence of redundant (p = 0.700) atrial septum primum in fetuses requiring UBAS at birth compared to the others. Interestingly, flat septum primum (restrictive appearance of the FO, with a limited motion of the atrial septum) was identified in 2 fetuses (6.7% of patients with D-TGAIVS—Table 2) and both of them required an UBAS. Interestingly, no fetus in the control group had a flat atrial septum (p = 0.053).
The hypermobile septum primum (oscillating between the left and right atrium during the cardiac cycle in fetal life) was found in 23/31 cases (88.5%—Table 2) during the first fetal examination and there was no significant difference between the three groups based on BAS (p = 0.234). Also, in latter evaluation, there wasn’t a statistical difference between UBAS [11 (78.6%)], Non-urgent BAS [8 (100%)] and No BAS groups [4 (100%)] (p = 0.158) (Table 3). This finding changed during pregnancy; 17/31 (55%) continue to present a hypermobile septum primum at the second examination (Table 2) without significant difference between the BAS groups. Hypermobile septum primum was less common in controls and was found only in 3 cases (14.3%, p < 0.001) (Table 4).
Finally, aneurysmal septum primum (defined as a dome-type) was identified in 24/31 (77.4%) cases and was seen in all 3 groups without statistical difference (p 0.365). This characteristic of the septum primum was noted even in the control group fetuses, without reaching significant difference compared to the TGAIVS group (p = 0.918) (Tables 2, 3 and 4).
The mean fetal FO length at the first examination was 0.46 ± 0.15 cm for the first operator and 0.47 ± 0.14 cm for the second operator, without significant differences between the two examinators and with a good reproducibility. Besides, this parameter was evaluated in different groups of BAS without a difference between the groups (Table 3).
The mean fetal FO length measured during the second examination was, for the first operator, 0.55 ± 0.16 cm in the UBAS group, 0.56 ± 0.17 cm in non-urgent BAS group, and 0.69 ± 0.15 cm in no BAS group. The fetal FO length was not significantly different between the three groups (p 0.400). Same results were found by the second operator (Table 2).
PFO/TSL ratio didn’t reach a statistically significant difference between the three groups at the first and second examination and also between the two operators (Table 2, Fig. 2). On the contrary, we found that PFO/TSL ratio reached a significant difference between patients with D-TGAIVS and controls patients at the second echocardiogram (mean 0.33 ± 0.11) and control cases (mean 0.47 ± 0.07) (p < 0.001) (Table 4).
There was a good interoperator reproducibility for all our measurements and ratios in both exams analyzed, as shown by Spearman’s rho correlation and Bland–Altman analysis (Fig. 2).
Moreover, we have found that the size of interatrial communication just before delivery and immediately after didn’t correlate. In other terms when we judge a widely open interatrial communication before birth that could be restrictive immediately after delivery or vice versa (Table 5).
We analyzed the pulmonary veins velocity just in 15/31 pts which had the appropriate images acquired. The mean gestational age of analysis was 30 weeks. No significant differences were found in pulmonary veins maximum and mean velocities stratified for different BAS groups (UBAS, Non-UBAS, No BAS). Based on gestational age, we found that there is a significantly higher peak pulmonary veins velocity after the 30th weeks compared to below 30 weeks (p = 0.05). This is likely due to the drop in pulmonary vascular resistance at the end of pregnancy (Table 6).
Discussion
The arterial switch operation has resulted in excellent survival in patients born with DTGAIVS. Nevertheless, a crucial point, that remains partially unsolved, is that some patients present severe hypoxemia immediately after delivery with non-negligible preoperative mortality and/or neurological damage [14,15,16,17,18]. Besides, during fetal life, in patients with D-TGAIVS oxygen saturation in the ascending aorta and, consequently, in the cerebral circulation is lower than in the pulmonary artery and ductus arteriosus. That’s the reason why it’s common to find mild microcephaly in these newborns. Therefore, the restoration of an acceptable saturation immediately after birth is one of the goals to be achieved, in the aim to reach the catch-up brain growth early in the post-operative period. We assessed the atrial septum reliably by two providers with good reproducibility. Our study found that the aspects of the atrial septum cannot be used to predict patients who will need UBAS and there is no correlation between the fetal and the immediately post-natal evaluation.
In our experience, 87.1% of patients with D-TGAIVS underwent BAS (15/31 Urgent BAS, 12/31 non-urgent BAS). This percentage is higher compared to other studies and there are significant practice variations between institutions [7, 9,10,11,12]. Our institution pays particular attention to avoid hypoxic brain damage. We attempt to avoid any delay in creating adequate mixing between the pulmonary and systemic circulations, to increase oxygen delivery and maintain adequate systemic perfusion [19]. That’s the reason why our systemic oxygen saturation threshold to define a critical condition for severe hypoxia and, consequently, an indication for UBAS is less than 70%. Our definition of UBAS is in agreement with the study carried out by Tuo et al. [11] as we give a time limit of 60 min from birth to UBAS. Other groups, on the other hand, have considered a different definition for UBAS up to 24 h after birth [9, 10, 12]; while Jouannic et al. set the limit of 30 min for defining an UBAS [7]. However, in our experience it should be noted that the group composed of newborns who underwent UBAS had an average saturation of 56.7% and a median of 60%, both values in line with other studies [9, 11].
Since the early 2000’s, multiple studies have been paid careful attention to the anatomy of the foramen ovale during fetal echocardiographic studies in fetuses with congenital heart malformations generally speaking [20, 21]. These studies described various echocardiographic patterns of the septum primum features such as an altered angle, excessive or reduced motility and/or an aneurysmatic conformation. They considered these features linked to the altered hemodynamic conditions in those patients. Afterward, Punn and Silverman paid careful attention to the aspect of the foramen ovale in fetuses with D-TGAIVS. They described an association of the septum primum hypermobility during the fetal life with the restriction of the FO at birth [9]. Furthermore, Tuo et al. confirmed that this morphology of the septum primum can be associated with an increased risk of UBAS at birth; but, they suggested that the risk increases in the presence of a hypermobile septum primum with an aneurysmal septum primum [11].
Nevertheless, in our experience we have not found any statistically significant association between these FO echocardiographic features to the need for BAS after birth. The only echocardiographic aspect that was always associated with an UBAS was the presence of a flat, thickened, almost muscular septum primum. We have found this parameter only in 2 out of 31 patients, therefore, because of the very small sample, without reaching a statistical value. Interestingly no fetuses in the control group had a flat septum.
Moreover, we highlighted that the hypermobile septum primum is significantly more frequent in patients with D-TGAIVS than in healthy controls. This finding could be explained by the fact that at the end of pregnancy in patients with D-TGAIVS there could be a decrease in pulmonary vascular resistance, due to the relatively high oxygen saturation in pulmonary arteries and ductus arteriosus, with an increase in pulmonary blood flow. The combination of these conditions can cause the restriction of ductus arteriosus and an increase in left atrial pressure. This would therefore result in a herniation of the septum primum in the right atrium, giving an aspect of a network that flaps from one atrium to the other. Another statistically significant difference that we found between D-TGAIVS and controls patients is in the PFO/TSL ratio (p < 0.001). According to our data, this ratio is lower in patients with TGA compared to the controls, indicating a smaller interatrial communication in patients with D-TGAIVS. This also could be explained by the increase in left atrial pressure in TGA due to increased pulmonary blood flow.
We also evaluated the aneurysmal septum primum, which in the literature is often considered a normal variation present in the third trimester of pregnancy rather than a pathological marker. Conversely, Jouannic et al. reported this aspect in association with inadequate mixing of the pulmonary and systemic circulation, but normal fetuses were not examined for comparison and our study showed no difference [7]. We have observed that the color Doppler outlines the anatomical profile of this redundancy of the septum primum, without, spreading inside the left atrium. Therefore, in this condition the evaluation of the amount of interatrial shunt is intriguing. This is the reason why we decided to measure the width of the effective interatrial communication not at the level of the FO (anatomical measurement), but at the level of the color Doppler passing through the redundant septum primum (functional measurement) (Fig. 3).
The evaluation of the interatrial communication just before the cesarean section did not predict the size of the interatrial communication just immediately after delivery (Table 5), considering also the inadequate acoustic windows given by the position of the fetus and the reduced amniotic fluid, in so advanced gestational age.
Therefore, the atrial septum evaluation despite being reproducible and meticulously evaluated was not a good predictor of the need for UBAS.
We did not find important differences in pulmonary venous Doppler velocities. Slodki et al. described a significantly higher maximum pulmonary veins velocity in those patients who required UBAS than in those not requiring BAS. However, it is important to specify that their definition of UBAS included a timing threshold up to 24 h after birth [12]. Therefore, it’s very difficult to compare our findings to theirs as most of the patients who underwent non-urgent BAS were still within 24 h of birth.
Limitations
The relatively small sample size due to the rarity of the disease is a limitation for the accuracy of the statistical analysis. On the other hand, our short period of analysis (2 years and 11 months), compared to other studies, increases the power of our observation.
Conclusions
Assessment of atrial septum anatomy in fetuses with D-TGAIVS is challenging. The need for an urgent BAS is still unpredictable. The only reliable aspect for the need of an urgent BAS is the presence of a flat, thickened, almost muscular septum primum, but it is seen in only few cases. However, based on the high likelihood to need an urgent BAS and the inability to predict that using the aspects of the atrial septum, we suggest that all fetuses with D-TGAIVS should be delivered at a tertiary care center with the ability to perform an urgent BAS if needed.
References
Calderon J, Angeard N, Moutier S, Plumet M-H, Jambaqué I, Bonnet D (2012) Impact of prenatal diagnosis on neurocognitive outcomes in children with transposition of the great arteries. J Pediatr 161(1):94-98.e1
Blyth M, Howe D, Gnanapragasam J, Wellesley D (2008) The hidden mortality of transposition of the great arteries and survival advantage provided by prenatal diagnosis. BJOG Int J Obstet Gynaecol 115(9):1096–1100
Bonnet D, Coltri A, Butera G, Fermont L, Le Bidois J, Kachaner J et al (1999) Detection of transposition of the great arteries in fetuses reduces neonatal morbidity and mortality. Circulation 99(7):916–918
van Velzen CL, Haak MC, Reijnders G, Rijlaarsdam MEB, Bax CJ, Pajkrt E et al (2015) Prenatal detection of transposition of the great arteries reduces mortality and morbidity. Ultrasound Obstet Gynecol 45(3):320–325
Kumar RK, Newburger JW, Gauvreau K, Kamenir SA, Hornberger LK (1999) Comparison of outcome when hypoplastic left heart syndrome and transposition of the great arteries are diagnosed prenatally versus when diagnosis of these two conditions is made only postnatally. Am J Cardiol 83(12):1649–1653
Maeno YV, Kamenir SA, Sinclair B, van der Velde ME, Smallhorn JF, Hornberger LK (1999) Prenatal features of ductus arteriosus constriction and restrictive foramen ovale in d-transposition of the great arteries. Circulation 99(9):1209–1214
Jouannic J-M, Gavard L, Fermont L, Le Bidois J, Parat S, Vouhé PR et al (2004) Sensitivity and specificity of prenatal features of physiological shunts to predict neonatal clinical status in transposition of the great arteries. Circulation 110(13):1743–1746
Soongswang J, Adatia I, Newman C, Smallhorn JF, Williams WG, Freedom RM (1998) Mortality in potential arterial switch candidates with transposition of the great arteries. J Am Coll Cardiol settembre 32(3):753–757
Punn R, Silverman NH (2011) Fetal predictors of urgent balloon atrial septostomy in neonates with complete transposition. J Am Soc Echocardiogr 24(4):425–430
Vigneswaran TV, Zidere V, Miller OI, Simpson JM, Sharland GK (2017) Usefulness of the prenatal echocardiogram in fetuses with isolated transposition of the great arteries to predict the need for balloon atrial septostomy. Am J Cardiol 119(9):1463–1467
Tuo G, Paladini D, Montobbio G, Volpe P, Cheli M, Calevo MG et al (2017) Prenatal echocardiographic assessment of foramen ovale appearance in fetuses with D-transposition of the great arteries and impact on neonatal outcome. Fetal Diagn Ther 42(1):48–56
Słodki M, Axt-Fliedner R, Zych-Krekora K, Wolter A, Kawecki A, Enzensberger C et al (2018) New method to predict need for Rashkind procedure in fetuses with dextro-transposition of the great arteries. Ultrasound Obstet Gynecol 51(4):531–536
Wilson AD, Rao PS, Aeschlimann S (1990) Normal fetal foramen flap and transatrial Doppler velocity pattern. J Am Soc Echocardiogr 3(6):491–494
Brossard-Racine M, du Plessis A, Vezina G, Robertson R, Donofrio M, Tworetzky W et al (2016) Brain injury in neonates with complex congenital heart disease: what is the predictive value of mri in the fetal period? AJNR Am J Neuroradiol 37(7):1338–1346
Andropoulos DB, Hunter JV, Nelson DP, Stayer SA, Stark AR, McKenzie ED et al (2010) Brain immaturity is associated with brain injury before and after neonatal cardiac surgery with high-flow bypass and cerebral oxygenation monitoring. J Thorac Cardiovasc Surg 139(3):543–556
Beca J, Gunn JK, Coleman L, Hope A, Reed PW, Hunt RW et al (2013) New white matter brain injury after infant heart surgery is associated with diagnostic group and the use of circulatory arrest. Circulation 127(9):971–979
Block AJ, McQuillen PS, Chau V, Glass H, Poskitt KJ, Barkovich AJ et al (2010) Clinically silent preoperative brain injuries do not worsen with surgery in neonates with congenital heart disease. J Thorac Cardiovasc Surg 140(3):550–557
Dimitropoulos A, McQuillen PS, Sethi V, Moosa A, Chau V, Xu D et al (2013) Brain injury and development in newborns with critical congenital heart disease. Neurology 81(3):241–248
Mukherjee D, Lindsay M, Zhang Y, Lardaro T, Osen H, Chang DC et al (2010) Analysis of 8681 neonates with transposition of the great arteries: outcomes with and without Rashkind balloon atrial septostomy. Cardiol Young 20(4):373–380
Donofrio MT, Bremer YA, Moskowitz WB (2004) Diagnosis and management of restricted or closed foramen ovale in fetuses with congenital heart disease. Am J Cardiol 94(10):1348–1351
Rudolph AM (2007) Aortopulmonary transposition in the fetus: speculation on pathophysiology and therapy. Pediatr Res 61(3):375–380
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AT: study design, LP: coordinated study, MM, TA: major contributors in writing the manuscript; MM, TA, AT: analyzed and interpreted patient data. All authors read and approved the final manuscript. All authors contributed to the design, data analysis and critically read the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was approved by the Institution Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (AVI 80104 kb)
Supplementary file2 (AVI 28453 kb)
Supplementary file3 (AVI 33528 kb)
Supplementary file4 (AVI 89215 kb)
Rights and permissions
About this article
Cite this article
Masci, M., Pasquini, L., Alsaied, T. et al. Reliability of Fetal Echocardiography in Predicting Postnatal Critical Hypoxia in Patients with Transposition of Great Arteries and Intact Ventricular Septum. Pediatr Cardiol 42, 1575–1584 (2021). https://doi.org/10.1007/s00246-021-02642-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02642-w






