Abstract
Developing a standardized protocol for pediatric exercise laboratories is challenging. Our objective was to report normal pediatric values for a continuous non-steady state cycle ergometer ramp protocol to achieve 8–10 min of exercise based on sex and weight. One hundred seventeen patients (117) [mean age 13 ± 2.8 years, range 7–18 years (51% male)] referred for chest pain with normal cardiac evaluation underwent cardiopulmonary testing on a cycle ergometer. Patients entered one of the four continuous ramp protocols (10, 15, 20, and 25 W/min ramp) to achieve an expected peak workload of 3 W/kg at an increase of 0.3 to 0.35 W/kg/min. Exercise test outcomes measured included duration, peak heart rate, work, respiratory exchange ratio, peak oxygen consumption, peak blood pressure, and ventilatory anaerobic threshold. An exercise duration of 8–10 min was achieved in a majority of the study population; however, interactions with age (older, longer duration) and sex (males, longer duration) were present. Using our algorithm (0.3–0.35 W/kg × weight), we demonstrated four non-steady state ramp bike ergometer protocols (10, 15, 20, and 25 W/min) that can be applied to males and females of different ages and weights to achieve an exercise duration of 8–10 min.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiopulmonary exercise tests (CPETs) allow for the study of cardiovascular and ventilatory systems responses to a known amount of exercise stress [1]. Achieving peak-level measurements of gas exchange, heart rate (HR), rhythm, and blood pressure (BP) allows for simultaneous evaluation of multiple organ systems [1]. CPETs should be reproducible with regard to maximal oxygen consumption (\({V_{{{\text{O}}_2}}}\)) and exercise parameters, and conducted within an appropriate time frame (10 ± 2 min) [2, 3]. Exercise tests less than 8 min are too intense, intimidating deconditioned patients and posing risks in those with cardiovascular disease. An exercise test longer than 12 min leads to boredom, lack of concentration, and motivation with failure to reach maximal effort [3].
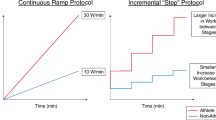
Most pediatric exercise testing protocols are adaptations of protocols used in adult populations; however, children cannot be considered “little adults” [4]. The Bruce treadmill protocol may limit young children because the work increments in between sequential stages may be too large to achieve [2, 3]. The James cycle protocol has limitations when applied to small children, or children with exercise intolerance, as they may not reach appropriate duration [2]. Multiple variations of these protocols have thus been developed to modify stage duration, increments in work rates, and pedaling cadence allowing for more fruitful stress testing of children and young adults [3]. This inter-programmatic variation in exercise protocols has led to difficulties in comparing exercise testing results across laboratories [5].
Continuous ramp cycle ergometer protocols allow for quality data collection in testing children and adolescents [2, 6,7,8,9]. Tanner et al. in 1991 report using a continuous ramp cycle protocol, creating a standard method for variation in workload, thus allowing for weight- and sex-based testing to be completed within an appropriate time frame [8]. Reference values for pediatric cycle ergometer protocols are lacking [5]. The work of Cooper et al. in 1984 provides current reference values for the bike ergometer using a ramp workload based on age [6]. Ten Harkel et al. reported normal values in 2010 using a step-wise increase in wattage (15 W/min or 20 W/min) on the bike ergometer based on height of the patient [9].
The purpose of our study was to implement and then report normal reference values for maximal CPET data performed on a continuous (not step wise) ramp cycle ergometer protocol using a weight- and sex-based protocol. Such “continuous ramp” normative data have not been reported, thus our data will provide useful comparative norms for all pediatric cardiopulmonary exercise labs adopting a similar exercise protocol that adapts and fits to children of all sizes and both sexes.
Methods
Approval by the Institutional Review Board of our institution was obtained; this research complied with the 1964 Declaration of Helsinki and its later amendments. Patients with the main complaint of chest pain and no other cardiac diagnosis based on normal office visit, electrocardiogram (ECG), and echocardiogram were selected for data review. The purpose of recruitment was to have an even distribution across the age range of the study and to reflect the body mass index (BMI) distribution in the US population. The goal was to have a sufficient sample size across the pediatric age spectrum. Testing occurred between 2004 and 2015. No patient had arrhythmia, ECG changes, or pulmonary disease. The study population consisted of 117 children, 60 of whom were male (51%) and 57, female. Ethnicity included 74 Caucasian, 28 African American, 1 American Indian, and 14 classified as other. The range of ages was from 7 to 18 years (mean age 13 ± 2.8 years), and the 117 patients were divided into 2 age groups [10]. The females were divided based on age 11 years or younger (N = 19) and age older than 11 years (N = 38). The males were divided based on age 13 years or younger (N = 33) and age older than 13 years (N = 27). No written consent was obtained for the study. Our Institutional Review Board approved this retrospective study using exercise data as long as the identifying data information was not revealed.
Exercise Tests
Baseline and post exercise pulmonary function testing (spirometry) generated a flow volume loop following the American Thoracic Society protocol and standards to rule out possible pulmonary origin of the chest pain [11]. Patients were attached to a stress ECG machine (GE Case System, GE Marquette Medical Systems, Milwaukee, WI) with a Mason–Likar placement of electrodes. Resting ECGs (supine, seated, standing, hyperventilating) were performed prior to the study. Studies were performed on a routinely calibrated, electronically braked cycle ergometer (Sensormedics, VIAsprint 150P, Yorba Linda, CA). Vigorous encouragement to maintain a pedaling rate between 75 and 85 revolutions/min continued throughout the duration of each study. Patients were entered into one of the four continuous ramp protocols (10, 15, 20, or 25 W/min) based on sex and weight. Work was increased 0.3 watts per kg body weight per minute (W/kg/min) for females and 0.35 W/kg/min for males. For example, a 66-kg female would be put into a 20-W/min ramp protocol and a 70-kg male would be placed into a 25-W/min ramp protocol.
Previous studies chose a work rate of 0.25 W/kg/min based on distributing a maximum workload of 3 W/kg over 12 min (or 3 W/kg divided by 12 min) yielding 0.25 W/kg/min as the work rate for their study population [8]. Our 0.3 W/kg/min work rate was based on estimating a max workload of 3 W/kg in children [12]. Since we targeted a 10-min study (instead of 12 min) across all groups, we divided 3 W/kg by 10 min to get 0.3 W/kg/min for females. Because, on average, males can achieve a larger workload than females, we divided 3.5 W/kg by 10 min to get 0.35 W/kg/min for males [13]. Initial workload started at zero and increased according to the selected protocol. Where the algorithm was indeterminate, the technician decided an appropriate level of work for cases. Metabolic measurements during exercise were obtained by breath-by-breath analysis throughout the study (Vmax 229C Encore, Cardinal Health, Yorba Linda, CA). Using 10-s averaging, ventilatory anaerobic threshold (VAT) was measured by the V-slope method and confirmed by using the ventilator-equivalent method [14]. BP measurements (Tango Stress Blood Pressure Monitor, SunTech Medical, Morrisville, NC) were collected at rest, after the first 2 min of exercise (at the beginning of the third minute of exercise), and then every 3 min until the termination of the study, with intermittent measurements as needed. BP was recorded at 1, 3, and 5 min during recovery by the attending physician. The first and fourth Korotkoff sounds were used for systolic and diastolic BP. Twelve-lead ECG rhythm strips were obtained every 3 min for the duration of the study and every minute of recovery.
All patients were able to coordinate their pedaling on the bike to meet end of test criteria. All patients were verbally encouraged to continue the test until exhaustion. End of test criteria were met when patients were unable to maintain a pedaling cadence above 70 revolutions/min and respiratory exchange ratio (RER) above 1.01.
Information extracted from the exercise study included protocol performed, duration of study (min), peak HR (beats/min), maximum work in watts (Wmax), maximum work/kg of weight (Wmax/kg), RER at maximal \({V_{{{\text{O}}_2}}}\) (RERmax), maximum (cc/min/kg) and absolute (l/min) \({V_{{{\text{O}}_2}}}\) (\({V_{{{\text{O}}_2}\;\hbox{max} }}\)), maximum systolic and diastolic BP measurements (mmHg), and VAT (V02 at VAT) in ml/kg/min and ratio of VAT (V02 at VAT) divided by \({V_{{{\text{O}}_2}\;\hbox{max} }}\) as a percentage.
Data Analysis
Descriptive statistics were calculated for resting and exercise metabolic measurements for age- and sex-specific groups. Two-sample unpaired t test was used to compare these groups in the current study sample and with the same age- and sex-specific groups across studies. This statistical analysis was performed using R Statistical Software, version 3.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
Patient data collected prior to the study included age, weight (kg), height (cm), race, sex, and BMI. Children were grouped into four BMI categories based on the Centers for Disease Control and Prevention’s BMI-for-age growth chart for sexes. The four categories are underweight (less than 5th percentile), healthy (5th to less than 85th percentile), overweight (85th to less than 95th percentile), and obese (equal to or greater than the 95th percentile) with prevalence shown in Fig. 1 [15, 16].
Number of patients by weight status based on body mass index (BMI). Breakdown of weight status categories based on BMI for 57 females (light shading) and 60 males (dark shading). Underweight (BMI < 5th percentile) and healthy weight status (BMI 5th ≤ 85th percentile) are depicted in the first two pairs of bars. Overweight (BMI 85th < 95th percentile) and obese status (BMI ≥ 95th percentile) patients are depicted in the last two pairs of bars. Of the females in our study, 26% were overweight or obese (11 overweight and 4 obese or 15/57 or 26%). Of the males in our study, 30% were overweight or obese (5 overweight and 13 obese or 18/60 or 30%) [15]
We reported the data in four groups—two male groups and two female groups. Since sex and puberty are important confounders in exercise testing, we divided the patient data into male and female groups.
We also compared our data with a previously published pediatric study by Cooper et al. [6] who studied 109 (58 boys and 51 girls ranging from 6 to 17 years old) patients on a bike ergometer. They used a ramp ergometer protocol with increasing work rate at 10, 15, 20, or 40 W/min based on the age of the patient with defined exercise duration goals of 5 to 12 min. The mean time was 9 min for their study. The Cooper et al. study was published in 1984 and based the workload solely on age rather than both weight and sex. We also compared peak V02 (same as V02 max) and VAT data from our four study groups directly with the Cooper et al. data groups [6].
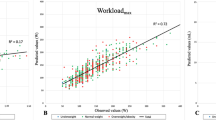
We tested whether each of the key variables (exercise duration, HR work, RER, peak oxygen consumption, or \({V_{{{\text{O}}_2}}},\) peak BP) varied by age and sex of the subjects by comparison of nested models using analysis of variance. To test whether a parameter varied by age, we compared a model with age and sex as a predictor to a reduced model that did not include age; testing for parameter variability by sex was done similarly. When the results of this analysis showed age and sex as significant predictors of test time, we reanalyzed the data in a subset of those who had a peak V02 > 25 cc/kg/min as a minimum standard for fitness to determine the typical time range for the test.
Results
Figure 1 shows our BMI results: 30% of our male population (5 + 13/60) and 26% of our female population (11 + 4/57) were categorized as ≥ 85th percentile of BMI for age and thus were either in the category of overweight or obese [15]. Table 1 shows the anthropometric data of the four groups of patients. Table 2 shows exercise test outcomes in the four groups of patients.
Exercise Test Work and Duration
Using the algorithm of 0.3 to 0.35 W/kg/min × weight, a workload of 3.1 to 3.4 W/kg in males was achieved. This translated to an average exercise duration of 8.5 to 9.93 min. In females, the mean peak workload achieved was 2.6 to 2.7 W/kg. The average duration of the study for females was 8 to 8.26 min.
Complications
No patient suffered significant complications. Our most common complication after exercise testing was dizziness due to hypotension from hypovolemia. There were no major morbidities such as ventricular tachycardia or syncope.
Gender-Specific Thresholds (See Table 3 )
Based on the age, sex, and peak V02 interactions found with test duration as described previously, we developed sex-specific age thresholds (≤ 11 years old for females and ≤ 13 years old for males described above). Table 3 shows the range in minutes for each of the four age and sex subgroups with normal fitness (V02 > 25 cc/kg/min). In general, there was time for adequate measurement of exercise parameters and most achieved an exercise time of 8 to 10 min.
Discussion
This study demonstrated the feasibility of using a continuous bicycle ramp ergometer protocol, adapted to age, sex, and body weight, to provide 8 to 10 min of exercise stress across childhood and adolescence. Our results showed that a ramp protocol based on sex and age involving a large number of children and adolescents can provide generally similar, maximal CPET results compared with previously published literature such as those provided by Cooper et al. [6]. Ogden et al. showed that the percentage of overweight and obese males and females in the US in 2007 and 2008 using the National Health and Nutrition Exam data (when most of our patients were exercised) was 34–35% [17]. This compares with our BMI distribution of 26–30% of children who were overweight and obese (Fig. 1). Thus our study population represents the general population of the same age because the BMI distribution of this cohort is similar to the reported US distribution [17, 18].
Duration
Older males exercised for a longer duration than the other groups. Older males comprised the only group to reach the exercise target of 10 ± 2 min. We were able to get the younger males and females to exercise 8 to 8.5 min so that data could be obtained during this time (which is more than the James protocol average of 6.2 min [8]).
Data Quality of Our Normal Values (See Table 4)
The quality of data is important because the change in habitual activity of children in 2004 to 2015 (more sedentary) compared with the activity of children in the 1980s (more active) has been raised as an issue when comparing fitness of children in the 1980s with children today [5]. When our data were compared with Cooper et al.’s 1984 data, peak V02 did not differ significantly in both of our female groups and our younger male group (13 years or younger) [6]. This suggests no significant change in fitness of children in the Cooper et al. patient population in 1984 compared with our patient population after 2000. The only group in which V02/kg was significantly different compared with the Cooper et al. groups was the older males (> 13 years) group versus our older males (> 13 years) (Cooper et al. 50 ± 8 vs. current study 45 ± 7, p = 0.037) [6]. The older males from the Cooper et al. study in southern California who participated in the study were more fit than the older males from the mid-Atlantic region.
The VAT was not different when comparing our data of younger and older males of all ages versus Cooper’s younger and older males. The VAT did differ among females 11 years of age and younger between our data and Cooper et al.’s data (p = 0.005), and between females older than 11 years in our data and Cooper et al.’s data (p = 0.007). The higher VAT in both of our female groups compared with Cooper et al.’s data suggests that our female groups were better conditioned, although peak V02 was not different when compared with Cooper et al.’s data.
Explanation for Dividing into Males/Females with Age Cutoffs
Establishing normal CPET values in children can be difficult due to child development. Sex and puberty are known confounders. We reported the data in four groups—two male groups and two female groups. The female pubertal growth spurt occurs between 10 and 13 years of age so we chose 11 years of age or younger as the dividing age between pre- and post-puberty in females [10]. The male pubertal growth spurt occurs between 12 and 15 years of age so we chose 13 years or younger as the dividing age between pre- and post-puberty in males [10]. Females mature faster at younger ages, and they may be bigger and better skilled than males in childhood [13]. After puberty, males have greater muscle mass, which provides more strength and power [13]. As shown in Oded Bar-Or’s Pediatric Sports Medicine for the Practitioner in 1983, when \({V_{{{\text{O}}_2}\;\hbox{max} }}\) is expressed as an absolute value (l/min), the rate of increase is similar between boys and girls up to age 12 years [19]. Godfrey et al. found that the highest workload completed depended significantly on height and sex of the child; males achieved higher workloads than females of similar height [7]. Since growth in height and body mass is commonly associated with puberty, it is important to differentiate individuals into pre- and post-pubescent groups to allow for appropriate reference comparisons.
Limitations
The present algorithm of 0.3 W/kg/min for females was an overestimate of the estimated maximum workload for non-conditioned females, as the mean workload for females was 2.6 to 2.7 W/kg (rather than 3 W/kg). However, we were able to get females to exercise 8 to 8.26 min so that data could be obtained during this time. Thus, the ramp work rate of 0.3 W/kg/min is suitable for this protocol. We divided the male and female groups based on expected time of puberty; however, we did not confirm pubertal status by measuring Tanner stages to confirm presence or absence of puberty [10]. Future studies should use Tanner stage testing to validate stages of puberty. This study population by nature of referral bias may not reflect fitness distribution of the general population. Future studies would need to record the exercise routine for study patients prior to exercise testing. Also, we had insufficient statistical power that did not allow separation by race. As reported previously, there are differences in racial groups for BP response and maximal workload [20]. Future studies should include more patients so that different racial groups can be studied accurately.
Conclusion
We report normal data for a non-steady state ramp from the lab for children 7 to 18 years of age without cardiac disease using a bicycle ergometer. Based on sex and weight, we increased the workload from 0.3 to 0.35 W/kg/min and put patients in either a 10-, 15-, 20-, or 25-W/min bicycle ergometer ramp protocol. We were able to achieve an optimal testing duration of 8 to 10 min, which falls within our goal of 8 to 12 min. This study showed safe and adaptable data for a continuous ramp protocol for males and females of different age groups. We present this standardized exercise cycle ergometer protocol for pediatric exercise labs so that results may be more easily compared between labs.
References
Wasserman K, Hansen JE, Sue DY, Casabur R, Whipp B (1999) Principles of exercise testing and interpretation: including pathophysiology and clinical applications, 3rd edn. Lippincott Williams and Wilkins, Philadelphia
Paridon S, Alpert BS, Boas SR, Cabrera ME, Caldarera LL, Daniels SR, Kimball TR, Knilans TK, Nixon PA, Rhodes J, Yetman AT, American Heart Association Council on Cardiovascular Disease in the Young, Committee on Atherosclerosis, Hypertension, and Obesity in Youth (2006) Clinical stress testing in the pediatric age group: a statement from the American Heart Association Council on Cardiovascular Disease in the Young, Committee on Atherosclerosis, Hypertension, and Obesity in youth. Circulation 113:1905–1920
Rowland TW (1993) Aerobic exercise testing protocols. In: Rowland TW (ed) Pediatric laboratory exercise testing: clinical guidelines. Human Kinetics, Champaign, pp 19–41
Tomassoni TL (1993) Conducting the pediatric exercise test. In: Rowland TW (ed) Pediatric laboratory exercise testing: clinical guidelines. Human Kinetics, Champaign, pp 1–17
Blais S, Berbari J, Counil FP, Dallaire F (2015) A systematic review of reference values in pediatric cardiopulmonary exercise testing. Pediatr Cardiol 36:1553–1564
Cooper DM, Weiler-Ravell D, Whipp BJ, Wasserman K (1984) Aerobic parameters of exercise as a function of body size during growth in children. J Appl Physiol Respir Environ Exerc Physiol 56:628–634
Godfrey S, Davies CT, Wozniak E, Barnes CA (1971) Cardio-respiratory response to exercise in normal children. Clin Sci 40(5):419–431
Tanner CS, Heise CT, Barber G (1991) Correlation of the physiologic parameters of a continuous ramp versus an incremental James exercise protocol in normal children. Am J Cardiol 67:309–312
Ten Harkel ADJ, Takken T, Van Osch-Gevers M, Helbing WA (2011) Normal values for cardiopulmonary exercise testing in children. Eur J Cardiovasc Prev Rehabil 18:48–54
Marshall WQ (1978) Puberty. In: Falkner F, Tanner JM (eds) Human growth, vol 2. Plenum, New York, pp 141–178
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J, ATS/ERS Task Force (2005) Standardisation of spirometry. Eur Respir J 26:319–338
Petzl DH, Haber P, Schuster E, Popow C, Haschke F (1988) Reliability of estimation of maximum performance capacity on the basis of submaximum ergometric stress tests in children 10–14 years old. Eur J Pediatr 147:174–178
Brooks GA, Fahey TD, Baldwin KM (1984) Sex difference in physical performance. In: Brooks GA, Fahey TD (eds) Exercise physiology: human bioenergetics and its applications, 1st edn. Wiley, New York, pp 637–659
Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60:2020–2027
Center for Disease Control and Prevention (n.d.) Body mass index: considerations for practitioners. https://www.cdc.gov/obesity/downloads/BMIforPactitioners.pdf. Accessed 2 April 2017
Center for Disease Control and Prevention (2017) Clinical growth charts. National Center for Health Statistics. http://www.cdc.gov/growthcharts/clinical_charts.htm. Accessed 14 Sep 2017
Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM (2010) Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA 303:242–249
Centers for Disease Control and Prevention (2017) National Health and Nutrition Examination (NHANES). http://www.cdc.gov/nchs/nhanes/index.htm. Accessed 20 Sep 2016
Freedson PS, Goodman TL (1993) Measurement of oxygen consumption. In: Rowland TW (ed) Pediatric laboratory exercise testing: clinical guidelines. Human Kinetics, Champaign, p 107
Alpert BS, Flood NL, Strong WB, Dover EV, DuRant RH, Martin AM, Booker DL (1982) Responses to ergometer exercise in a healthy biracial population of children. J Pediatr 101:538–545
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Work completed at Nemours/Alfred I. duPont Hospital for Children, Wilmington, DE.
Rights and permissions
About this article
Cite this article
Octavio, J.M., Folk, A.L., Falini, L. et al. Standardization of a Continuous Ramp Ergometer Protocol for Clinical Exercise Testing in Children. Pediatr Cardiol 40, 834–840 (2019). https://doi.org/10.1007/s00246-019-02079-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02079-2