Abstract
Accurate assessment of ventricular function is particularly important in children with hypoplastic left heart syndrome (HLHS) after completion of the total cavopulmonary connection (TCPC). For this purpose, two-dimensional speckle tracking (2DST) is a promising technique as it does not depend on the angle of insonation or the geometry of the ventricle. The objective of this study was to assess changes in systolic and diastolic right ventricular (RV) function within a 5-year follow-up period of HLHS patients after TCPC using conventional and 2DST echocardiography. RV fractional area change (RVFAC), tricuspid annular plane systolic excursion (TAPSE), E/A, E/e′ and 2DST parameters [global longitudinal peak systolic strain (GS) and strain rate (GSRs), global strain rate in early (GSRe) and late (GSRa) diastole] of 40 HLHS patients were compared at 1.6 and at 5.1 years after TCPC. RVFAC, E/A, E/e′ and GS did not change, whereas TAPSE (13.7 ± 3.2 vs. 10.5 ± 2.4 mm/m2, p < 0.001), GSRs (−1.56 ± 0.28 vs. −1.35 ± 0.31 1/s, p < 0.001), GSRe (2.22 ± 0.49 vs. 1.96 ± 0.44 1/s, p = 0.004) and GSRa (1.19 ± 0.39 vs. 0.92 ± 0.39 1/s, p < 0.001) decreased significantly. Systolic and diastolic RV function parameters of HLHS patients decreased from 1.6 to 5.1 years after TCPC in our patients. Changes in global strain rate parameters may be signaling early RV dysfunction that is not detectable by traditional echocardiography. Further study is needed to verify this and to determine whether these changes are clinically relevant.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Serial echocardiographic assessment of right ventricular (RV) function is essential in children with hypoplastic left heart syndrome (HLHS) following surgical palliation with the total cavopulmonary connection (TCPC). Due to the complex geometry of the single RV, echocardiographic assessment remains challenging [1]. Cardiac catheterization and magnetic resonance imaging serve as gold standards for hemodynamic assessment of the RV in biventricular and univentricular circulations [2, 3]. Standardized echocardiographic RV examination protocols only exist for the biventricular heart [4], in clinical practice RV function is mostly analyzed qualitatively. Two-dimensional speckle tracking (2DST) is a promising echocardiography technique for quantifying RV function [5]. Limitations related to geometry or angle of insonation are lacking [6]. RV function in the HLHS cohort has been studied using this technique throughout all stages of Fontan palliation [7–9]. Recently, the 2DST parameter global longitudinal strain rate (GSR) has been suggested as possible preload independent parameter of systemic RV contractility in HLHS after TCPC [10, 11]. Moreover, 2DST can also be applied to accurately assess diastolic function [12, 13]. This is especially important for the evaluation of the single RV, where studies have shown diastolic ventricular dysfunction to precede systolic ventricular dysfunction during midterm and long-term follow-up [3, 14]. The aim of our study was to assess serial changes in systolic and diastolic ventricular function parameters at short-term follow-up and 5 years after TCPC of HLHS patients following TCPC using the 2DST technology. We hypothesized that 2DST parameters can be helpful in detecting early subclinical changes of ventricular function parameters in these patients.
Methods
Patients
We searched our database for children with HLHS who had undergone three-stage palliation at our institution. All patients were operated at all three stages by the same surgeon. By institutional preference, all patients had a Norwood operation with modified Blalock–Taussig shunt as stage one, a Hemi Fontan operation as stage two and stage three consisted of TCPC with lateral, intra-atrial tunnel with a 4 mm fenestration. Fenestrations were routinely closed 1 year after TCPC until 2007; afterward, indications for closure were individualized and included, for example, significant cyanosis and embolic complications. Patients that had their TCPC between January 2004 and December 2009 were analyzed.
Echocardiography
Patients needed to have at least 2 follow-up echocardiograms in our clinic. The first examination was performed at a median time of 1.6 years (T1) and the second examination at a median time of 5.1 years (T2) after TCPC (see Table 1). The timing was chosen, so that for T1 patients were beyond the immediate postoperative period and T2 represents the longest available follow-up. Both exams had to be performed using a standardized echocardiography protocol, including a gray scale apical four chamber view (A4CV) with a frame rate maintained at >60 fps, and patients had to be under stable conditions as outpatients. All recordings were conducted using a Vivid 7 scanner (GE, Healthcare, Wauwatosa, WI) and analyzed using an off-line workplace by one single investigator (M.M.) (Echo PAC PC 2008, GE Healthcare).
Ventricular function (VF), tricuspid regurgitation and neo-aortic valve insufficiency (Neo-AI) were graded subjectively (VF: 1 = good, 2 = moderately decreased, 3 = severely decreased; Valves: 1 = absent, 2 = trivial, 3 = mild, 4 = moderate, 5 = severe). Tricuspid annular plane systolic excursion (TAPSE) was measured by M-mode at the hinge point of the lateral tricuspid valve leaflet with the RV free wall and indexed to body surface area [15]. Right ventricular fractional area change (RVFAC) was calculated as end-diastolic minus end-systolic area/end-diastolic area from the A4CV. E- and A-wave velocities were taken from pulsed wave Doppler inflow of the tricuspid valve, and E/A was calculated. If E- and A-wave were fused, only E-wave was measured. Color tissue Doppler imaging was obtained from the RV free wall keeping the angle of insonation at <30° relative to the direction of the movement of the myocardium. Mean color Doppler myocardial velocities were obtained from a 5 × 5 mm region of interest in the myocardium adjacent to the lateral tricuspid valve annulus. The peak early diastolic velocity (E′) was measured and averaged for analysis from 3 consecutive heartbeats. The presence of patent fenestration was assessed by color Doppler imaging of the lateral intra-atrial Fontan baffle.
For 2DST, the endocardial border of the single RV was traced manually from the A4CV. A region of interest consisting of six segments dividing the RV was automatically proposed by the software and manually corrected if necessary. Borders were accepted if both the visual inspection and the software indicated adequate tracking for all segments. Global longitudinal systolic strain (GS), global longitudinal systolic strain rate (GSRs), global longitudinal early diastolic strain rate (GSRe) and global longitudinal late diastolic strain rate (GSRa) were obtained by postprocessing evaluation using average values of the six segments. Segments were excluded if the myocardium was not visualized well enough to allow 2DST.
Statistics
Data are expressed as median and interquartile range, or mean and standard deviation as appropriate. Testing for normality was performed using the Kolmogorov–Smirnov test. For the comparison of the two examinations within the follow-up period, paired Wilcoxon signed rank test, paired samples Student’s t test, marginal homogeneity test and McNemar test were used as appropriate. For the comparison of patients with and without ACE inhibitors, Student’s t test for independent samples was used. Correlation of parameters was assessed with the nonparametric Spearman’s rho test, or with the parametric Pearson test as appropriate. p Values ≤0.05 were considered significant. All analyses were conducted using the statistical software package SPSS 20.0 (SPSS Inc., Chicago, IL, USA) and MedCalc version 14.12 (MedCalc Software, Mariakerke, Belgium). Interobserver variability of 2DST parameters was assessed by having two different observers (M.M. and J.L.) making the same measurements on the same 2D echo loop at separate times on 20 randomly selected patients, and the coefficient of variation was calculated.
Graphics
Graphics were created using MetaPost, a free interpreter software by John D. Hobby, version 1.211, distributed within the TEX framework via the public domain Comprehensive TEX Archive Network.
Ethical Standards
The study was approved by the institutional review board, and all patients gave their consent for anonymized data collection and analysis.
Results
Study Population
40 patients were included in the study for analysis (26 male patients). HLHS sub-type was as follows: 10 mitral stenosis/aortic stenosis, 9 mitral stenosis/aortic atresia, 17 mitral atresia/aortic atresia and 4 mitral atresia/aortic stenosis. Patient characteristics are displayed in Table 1. The patients underwent TCPC at a median age of 2.5 (2.3–2.9) years.
Conventional Echocardiography Parameters
Conventional echocardiography parameters are displayed in Table 2. Mean frame rate was 78 (±16) fps at the first and 85 (±8) fps at the second examination. RVFAC remained unchanged, while TAPSE decreased significantly. Diastolic Doppler parameters E/A and E/E′ did not change.
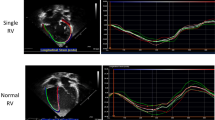
Two-Dimensional Speckle Tracking
Results of 2DST echocardiography are shown in Fig. 1. GS did not change between the first and the second observation, whereas GSRs decreased significantly. The diastolic parameters GSRe and GSRa also decreased significantly.
Correlation of 2DST with Conventional Echocardiography Parameters
RVFAC did not correlate with systolic 2DST parameters, while TAPSE showed a statistically significant but weak correlation with both GS and GSRs. E/A and E/E′ did not correlate with the diastolic 2DST parameters GSRe or GSRa (Table 3).
Influence of ACE Inhibitors
In a sub-analysis, we compared patients who were on ACE inhibitors with patients who were not. Groups did not show significant differences for any of the traditional or 2DST diastolic and systolic function parameters at the first or second examination.
Interobserver Variability
Interobserver variability was in a similar range for the systolic parameters GS and GSRs (GS, −10.5 %; GSRs, −9.9 %) and a little bit higher for the diastolic parameters GSRe and GSRa (GSRe, −14.0 %; GSRa, −15.8 %).
Discussion
To our knowledge, this is the first study reporting on longitudinal changes of RV systolic and diastolic function in HLHS following TCPC using traditional and 2DST echocardiography. We were able to show that from a median of 1.6–5.1 years after TCPC, the traditional parameters RVFAC, E/A and E/E′ did not change while TAPSE decreased. The main finding of our study was that both systolic and diastolic RV GSR parameters decreased significantly, while GS did not change during our observed follow-up period.
Systolic Changes
Among the traditional echocardiographic parameters, TAPSE decreased significantly. In biventricular hearts, Koestenberger [15] showed that TAPSE increases with age. The same author noticed a positive correlation of TAPSE with BSA, hence we chose to index TAPSE to BSA in order to be able to compare patients with different body sizes and to minimize the impact of growth on TAPSE [16]. Thus, we think the decrease in indexed TAPSE in our patients reflects a true decline in longitudinal excursion of the basal RV free wall. When interpreting TAPSE values, one should consider the preload dependency of this parameter [17, 18]. Since preload cannot be assessed adequately by echocardiographic techniques, it could not be measured in this study. In the Fontan circulation, a change in preload occurs, for example, when patients develop significant tricuspid or neo-aortic regurgitation or Fontan, conduit fenestrations are closed [17, 18]. In our study group, the degree of valve regurgitation did not change between examinations but significantly more patients had closed fenestration at the time of the second examination. Due to study design, we were unable to assess whether this may have had an impact on the TAPSE results but consider it unlikely. In our patients, RVFAC did not change during follow-up. RVFAC is a parameter of global systolic function that has been described as a surrogate for the ejection fraction (EF) for the morphologic RV, and it has been shown to correlate well with cardiac magnetic resonance-derived EF [19, 20]. In Fontan patients, the EF was found to be stable over 15 years of follow-up [3]. Therefore, as a global parameter of ventricular function similar to the EF, RVFAC might not be an ideal parameter for the assessment of subclinical changes in RV function. In our opinion, it is not contradictory to have found decreasing TAPSE but unchanged RVFAC in our patients. The regional function near the base may well have decreased, while the global function was still preserved.
It was recently shown in a study by our group in HLHS patients after Fontan that GSRs correlated with conductance catheter-derived indices of myocardial contractility and was not affected by acute preload changes [11]. Therefore, we think that, if applied correctly, 2D strain rate imaging might be a valuable new asset for echocardiographic follow-up of this patient population. In the current study, within a follow-up period of 5 years after Fontan, GSRs decreased significantly, while GS did not change. Since strain describes the deformation in percent and strain rate the velocity of deformation, this result could mean that the velocity of deformation declined first, while overall deformation was still preserved in our patients.
Previous studies have indicated a potentially higher sensitivity of GSRs compared to GS to detect subtle changes in systolic function. A study in healthy subjects with biventricular hearts reported on right atrial and ventricular adaptation to training [21]. Only GSRs, but not GS was able to reveal these adaptations. In another study, Kaneko et al. [22] compared patients with single right and left ventricles and found longitudinal GSRs values to be lower in patients with RV than with LV morphology before bidirectional cavopulmonary connection while GS was not different. These studies can be viewed as support for the notion that GSRs may be more sensitive to detect subtle changes in global deformation, possibly because a decline in the velocity of deformation precedes noticeable changes in deformation itself.
Diastolic Changes
The evaluation of diastolic function in patients with a single right ventricle remains problematic because it is neither standardized nor do normal values exist. In our study, we utilized conventional Doppler imaging as well as speckle tracking techniques in an attempt to investigate changes of diastolic function over time. One commonly used method for diastolic function assessment in the systemic left ventricle is the mitral inflow Doppler derived E/A ratio which, in the absence of atrioventricular valve disease, can yield information about relaxation and filling properties of the ventricle during diastole. Because no normal values exist in our patient population, the absolute values are of questionable value, but it is important to note, that there was no change over time in this parameter. The same was true for the other commonly utilized parameter we chose, E/E′, which is a ratio that combines inflow Doppler and tissue Doppler to estimate filling pressures. Elevated values found in the systemic left ventricle correlate to elevated left ventricular filling pressures in adults [23]. This ratio in our patients also did not change.
In contrast to these conventional parameters of diastolic function, the speckle tracking parameters GSRe and GSRa decreased significantly within the follow-up period. There is evidence from multiple studies using different technologies that the diastolic function can be or become impaired in single ventricle patients after TCPC. The Pediatric Heart Network on contemporary outcomes after the Fontan procedure described abnormal diastolic function using conventional echocardiographic techniques in 72 % of children who had undergone a Fontan operation [14]. That study confirmed findings by Penny et al. [24] who found abnormalities in diastolic function of single LV Fontan patients using traditional echocardiography methods more than 20 years ago. In a tissue Doppler study of single LV patients 7.4 years after Fontan operation, reduced diastolic function compared to biventricular controls was reported [25].
Using speckle tracking echocardiography, Ho et al. [26] examined single LVs long-term after TCPC and found significantly reduced longitudinal GSRe compared to controls. In another study, Kaneko et al. [22] did not find a decrease in GSRe when they compared values before stage 2 palliation and after TCPC. However, because the mean age of the patient population after TCPC was only 3.4 years, these results do not contradict our results, since patients in our study had a median age of 7.7 years at the second examination. The decrease in diastolic strain rate may be exactly during this time frame which they did not focus on. These studies show that diastolic strain rate imaging can be successfully applied in this patient population which is in line with our own experiences. In fact, strain rate imaging may be better suited than conventional Doppler and tissue Doppler methods because there is some data that it is less dependent on preload conditions [11].
End-diastolic pressure (EDP) has been shown to gradually rise with Fontan follow-up indicating worsening diastolic properties [3]. In the single RV, EDP correlated strongly with GSRe and was found to correlate better than any other diastolic echocardiographic measurement [10]. Husain et al. therefore suggested GSRe as a possible non-invasive parameter to estimate EDP. Unfortunately, we were unable to investigate a relationship between GSRe and filling pressures because we had no invasive data available at the time of most echocardiograms.
In this study, we found a concomitant decrease in GSRa, representing the velocity of fiber lengthening during late diastolic filling. In single ventricle hearts, Khoo et al. [27] measured atrial strain and strain rate and found reduced atrial reservoir and conduit function, and an increased reliance on atrial active function for ventricular filling. The single ventricle atrial mechanics deviated significantly from normal early childhood maturational changes, and the authors compared their findings to those of an atrium that is facing early ventricular diastolic dysfunction.
Diastolic function parameters can potentially be affected by heart rate. The heart rate of our patients at the second echocardiography was significantly lower than at the early echocardiography, following the natural trend of the heart rate to decrease between ages 4 and 8 years. Considering this and the fact that the heart rates were not high enough to impair ventricular filling, we consider it unlikely that the heart rate difference contributed significantly to the differences in diastolic strain rate parameters we found.
Similarly, differences in medication use could potentially have an effect on diastolic function. While ACE inhibitors are standard of care for systolic heart failure, their influence on diastolic function is less clear. Therefore, we compared patients with and without ACE inhibitor therapy at both follow-up times and found no differences in systolic or diastolic function parameters between groups. Based on these results in our patients, one can assume that ACE inhibitor therapy did not influence our results significantly.
In HLHS Fontan patients, ventricular function can be influenced by many factors. Differences in regional diastolic function or diastolic dyssynchrony may influence global diastolic function. Our study focused on global rather than on regional deformation. Differences in regional systolic deformation values have been shown [28], and possibly influence global deformation parameters [29]. A different size of the remnant LV in the anatomic subgroups might impact regional function, but global longitudinal systolic deformation has been shown to be independent from the HLHS sub-type [30]. Increased diastolic dyssynchrony is also noted in this patient population, albeit the association with reduced global diastolic function is still lacking [31]. Elevated arterial elastance of the reconstructed aorta after the Norwood operation correlates with diastolic stiffness of the systemic RV which further influences diastolic function [32]. Uncoordinated ventricular relaxation and myocardial fibrosis have also been associated with decreased diastolic function in the univentricular heart [24]. To which extent changes in preload during three-step palliation influence diastolic function has not been studied. Investigation of these complex pathophysiological changes involved in diastolic dysfunction was beyond the scope of this study.
Limitations
The main limitations are related to the retrospective design of the study, and hence the fact that not all echocardiography examinations were optimized for the purpose of 2DST. Due to imaging quality, not all segments could be examined in every patient. Circumferential and radial deformation parameters were not obtained since we find it difficult to standardize short axis views in the single RV in clinical practice. We were unable to include invasive hemodynamic parameters as echocardiographic studies were performed during outpatient visits. Inherent to methodology, our “global deformation parameters” do not reflect longitudinal deformation of the whole RV but only that of the visualized slice from the apical 4-chamber view. Finally, it should be noted that the interobserver variability for the 2DST parameters of about 10–15 % has to be considered when interpreting results, but it was in a similar range as in other studies examining the single RV using the same technology [28, 30]. Due to study methodology and sample size, the influence of Fontan fenestration patency on our findings could not be determined accurately.
Conclusion
This is the first study reporting on longitudinal changes in ventricular systolic and diastolic function parameters in HLHS patients following Fontan repair using 2DST echocardiography. Systolic and diastolic GSR decreased between measurement times at 1.5 and 5 years after TCPC. These early global changes were not detected by traditional echocardiography techniques. It is unclear whether the changes we found in systolic and diastolic strain rate will become clinically relevant in terms of overt RV dysfunction. Future research may show whether this change possibly signals early, subclinical changes of intrinsic function or is a reflection of RV adaptation to abnormal loading conditions in the Fontan circulation.
References
Mahle WT, Coon PD, Wernovsky G, Rychik J (2001) Quantitative echocardiographic assessment of the performance of the functionally single right ventricle after the Fontan operation. Cardiol Young 11:399–406
Goetschalckx K, Rademakers F, Bogaert J (2010) Right ventricular function by MRI. Curr Opin Cardiol 25:451–455
Nakamura Y, Yagihara T, Kagisaki K, Hagino I, Kobayashi J (2011) Ventricular performance in long-term survivors after Fontan operation. Ann Thorac Surg 91:172–180
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713 (quiz 786–688)
Abraham TP, Dimaano VL, Liang HY (2007) Role of tissue Doppler and strain echocardiography in current clinical practice. Circulation 116:2597–2609
Bijnens BH, Cikes M, Claus P, Sutherland GR (2009) Velocity and deformation imaging for the assessment of myocardial dysfunction. Eur J Echocardiogr 10:216–226
Petko C, Hoffmann U, Möller P, Scheewe J, Kramer HH, Uebing A (2010) Assessment of ventricular function and dyssynchrony before and after stage 2 palliation of hypoplastic left heart syndrome using two-dimensional speckle tracking. Pediatr Cardiol 31:1037–1042
Petko C, Uebing A, Furck A, Rickers C, Scheewe J, Kramer HH (2011) Changes of right ventricular function and longitudinal deformation in children with hypoplastic left heart syndrome before and after the Norwood operation. J Am Soc Echocardiogr 24:1226–1232
Hill GD, Frommelt PC, Stelter J, Campbell MJ, Cohen MS, Kharouf R, Lai WW, Levine JC, Lu JC, Menon SC, Slesnick TC, Wong PC, Saudek DE (2015) Impact of initial Norwood shunt type on right ventricular deformation: the single ventricle reconstruction trial. J Am Soc Echocardiogr 28:517–521
Husain N, Gokhale J, Nicholson L, Cheatham JP, Holzer RJ, Cua CL (2013) Noninvasive estimation of ventricular filling pressures in patients with single right ventricles. J Am Soc Echocardiogr 26:1330–1336
Schlangen J, Petko C, Hansen JH, Michel M, Hart C, Uebing A, Fischer G, Becker K, Kramer HH (2014) Two-dimensional global longitudinal strain rate is a preload independent index of systemic right ventricular contractility in hypoplastic left heart syndrome patients after Fontan operation. Circ Cardiovasc Imaging 7:880–886
Perry R, De Pasquale CG, Chew DP, Joseph MX (2008) Assessment of early diastolic left ventricular function by two-dimensional echocardiographic speckle tracking. Eur J Echocardiogr 9:791–795
Herod JW, Ambardekar AV (2014) Right ventricular systolic and diastolic function as assessed by speckle-tracking echocardiography improve with prolonged isolated left ventricular assist device support. J Card Fail 20:498–505
Anderson PA, Sleeper LA, Mahony L, Colan SD, Atz AM, Breitbart RE, Gersony WM, Gallagher D, Geva T, Margossian R, McCrindle BW, Paridon S, Schwartz M, Stylianou M, Williams RV, Clark BJ 3rd (2008) Contemporary outcomes after the Fontan procedure: a Pediatric Heart Network multicenter study. J Am Coll Cardiol 52:85–98
Koestenberger M (2012) Transthoracic echocardiography in children and young adults with congenital heart disease. ISRN Pediatr 2012:753481
Koestenberger M, Ravekes W, Everett AD, Stueger HP, Heinzl B, Gamillscheg A, Cvirn G, Boysen A, Fandl A, Nagel B (2009) Right ventricular function in infants, children and adolescents: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 640 healthy patients and calculation of z score values. J Am Soc Echocardiogr 22:715–719
Kasnar-Samprec J, Kuhn A, Horer J, Vogt M, Cleuziou J, Lange R, Schreiber C (2012) Unloading of right ventricle by bidirectional superior cavopulmonary anastomosis in hypoplastic left heart syndrome patients promotes remodeling of systemic right ventricle but does not improve tricuspid regurgitation. J Thorac Cardiovasc Surg 144:1102–1108
Koestenberger M, Ravekes W (2013) Value of the tricuspid annular plane systolic excursion as a follow-up parameter in patients with hypoplastic left heart syndrome. J Thorac Cardiovasc Surg 145:1682–1683
Mertens LL, Friedberg MK (2010) Imaging the right ventricle—current state of the art. Nat Rev Cardiol 7:551–563
Anavekar NS, Gerson D, Skali H, Kwong RY, Yucel EK, Solomon SD (2007) Two-dimensional assessment of right ventricular function: an echocardiographic-MRI correlative study. Echocardiography 24:452–456
Pagourelias ED, Kouidi E, Efthimiadis GK, Deligiannis A, Geleris P, Vassilikos V (2013) Right atrial and ventricular adaptations to training in male Caucasian athletes: an echocardiographic study. J Am Soc Echocardiogr 26:1344–1352
Kaneko S, Khoo NS, Smallhorn JF, Tham EB (2012) Single right ventricles have impaired systolic and diastolic function compared to those of left ventricular morphology. J Am Soc Echocardiogr 25:1222–1230
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA (1997) Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30:1527–1533
Penny DJ, Rigby ML, Redington AN (1991) Abnormal patterns of intraventricular flow and diastolic filling after the Fontan operation: evidence for incoordinate ventricular wall motion. Br Heart J 66:375–378
Vitarelli A, Conde Y, Cimino E, D’Angeli I, D’Orazio S, Ventriglia F, Bosco G, Colloridi V (2005) Quantitative assessment of systolic and diastolic ventricular function with tissue Doppler imaging after Fontan type of operation. Int J Cardiol 102:61–69
Ho PK, Lai CT, Wong SJ, Cheung YF (2012) Three-dimensional mechanical dyssynchrony and myocardial deformation of the left ventricle in patients with tricuspid atresia after Fontan procedure. J Am Soc Echocardiogr 25:393–400
Khoo NS, Smallhorn JF, Kaneko S, Kutty S, Altamirano L, Tham EB (2013) The assessment of atrial function in single ventricle hearts from birth to Fontan: a speckle-tracking study by using strain and strain rate. J Am Soc Echocardiogr 26:756–764
Petko C, Hansen JH, Scheewe J, Rickers C, Kramer HH (2012) Comparison of longitudinal myocardial deformation and dyssynchrony in children with left and right ventricular morphology after the Fontan operation using two-dimensional speckle tracking. Congenit Heart Dis 7:16–23
Gokhale J, Husain N, Nicholson L, Texter KM, Zaidi AN, Cua CL (2013) QRS duration and mechanical dyssynchrony correlations with right ventricular function after Fontan procedure. J Am Soc Echocardiogr 26:154–159
Petko C, Voges I, Schlangen J, Scheewe J, Kramer HH, Uebing AS (2011) Comparison of right ventricular deformation and dyssynchrony in patients with different subtypes of hypoplastic left heart syndrome after Fontan surgery using two-dimensional speckle tracking. Cardiol Young 21:677–683
Stiver C, Nadorlik H, Nicholson L, Janevski I, Belfrage K, Wheller J, Cua CL (2015) Diastolic dyssynchrony differences in patients with single right ventricles vs control patients. Congenit Heart Dis 10:326–332
Schlangen J, Fischer G, Petko C, Hansen JH, Voges I, Rickers C, Kramer HH, Uebing A (2013) Arterial elastance and its impact on intrinsic right ventricular function in palliated hypoplastic left heart syndrome. Int J Cardiol 168:5385–5389
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Drs. Miriam Michel and Jana Logoteta contributed equally to this work and share the first authorship.
Drs. Colin Petko and Hans-Heiner Kramer share the last authorship.
Rights and permissions
About this article
Cite this article
Michel, M., Logoteta, J., Entenmann, A. et al. Decline of Systolic and Diastolic 2D Strain Rate During Follow-Up of HLHS Patients After Fontan Palliation. Pediatr Cardiol 37, 1250–1257 (2016). https://doi.org/10.1007/s00246-016-1424-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1424-5