Abstract
Few data exist evaluating the epidemiology of Kawasaki disease (KD) resistant to intravenous immunoglobulin (IVIG) in the United States on a national level, and characterization of the epidemiology of IVIG resistance may improve patient care. We aim to characterize the incidence of KD resistant to IVIG therapy and risk factors for resistance in children’s hospitals in the United States. A large, administrative database was used to identify pediatric patients admitted with an ICD-9 code for mucocutaneous lymph node syndrome (446.1) and a charge for at least one dose of IVIG. Patients were identified as resistant to IVIG therapy if there were ≥2 calendar days between an initial IVIG dose and a subsequent dose of IVIG, methylprednisolone, rituximab, or infliximab. Patient demographic and hospital information were collected, as well as the charges for imaging, laboratory, and medications. Resistance occurred in 16.3 % (hospital range 8.0–26.8 %) of the population and was not associated with time or number of patients admitted with KD. Patients admitted to hospitals in the highest quartile of resistance were more likely to be African-American (26.5 vs 20.1 %, p < 0.01), less likely to have an echocardiogram performed (93.6 vs 97.1 %, p < 0.01), were more likely to have a C-reactive protein drawn (93 vs 79.9 %, p < 0.01), and were less likely to have an erythrocyte sedimentation rate drawn (87.9 vs 91.6 %, p < 0.01). The incidence of KD resistant to IVIG is highly variable among pediatric hospitals and treatment patterns vary between hospitals with high- and low-resistance patterns. Further evaluation of diagnostic and treatment patterns at pediatric hospitals is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The mainstay of treatment for Kawasaki disease (KD) for many years has been intravenous immunoglobulin (IVIG) [8]. The efficacy of IVIG therapy was been well established in preventing coronary artery aneurysms. However, a significant number of patients (10–20 %) with KD experience ‘resistance’ to IVIG therapy, defined as a persistent fever ≥36 h after an initial IVIG dose [1, 8]. Multiple doses of IVIG are recommended in this scenario, and recent literature has also advocated the use of monoclonal antibody preparations, such as infliximab or rituximab, or methylprednisolone, in resistant patients [8, 13].
Locally focused studies, primarily in Japan, have been performed to develop scoring systems to predict patient’s IVIG resistance, but have not evaluated the epidemiology of IVIG resistance on a large scale [3, 5, 7, 10, 11]. In the United States, increased incidences of IVIG-resistant KD have been noted in specific regions of the country [14]. We hypothesized that IVIG resistance is different in various geographic regions of the United States. These differences may be due to the potentially variable content of IVIG preparations, variability in patient care practices or diagnostic techniques at pediatric hospitals, and differing racial and ethnic distributions in the United States. Data generated from investigating IVIG resistance in this manner may elucidate patterns useful for prediction of resistance or serve as a baseline for future investigations. Therefore, our aim was to characterize the epidemiology of KD resistant to IVIG therapy in pediatric hospitals in the United States and identify risk factors which may be associated with IVIG resistance.
Methods
A retrospective, descriptive study was designed, and Institutional Review Board exemption was obtained. Data for this study were obtained from the Pediatric Health Information System (PHIS), an administrative database that contains inpatient, emergency department, ambulatory surgery, and observation data from 43 not-for-profit, tertiary care pediatric hospitals in the United States. These hospitals are affiliated with the Child Health Corporation of America (Shawnee Mission, KS), a business alliance of children’s hospitals. Data quality and reliability are assured through a joint effort between the Child Health Corporation of America and participating hospitals. The data warehouse function for the PHIS database is managed by Thomson Reuters (Ann Arbor, MI). For the purposes of external benchmarking, participating hospitals provide discharge/encounter data including demographics, diagnoses, and procedures. Forty two of these hospitals also submit resource utilization data (e.g., pharmaceuticals, imaging, and laboratory) into PHIS. Data are de-identified at the time of data submission, and data are subjected to a number of reliability and validity checks before being included in the database.
Data were queried for patients discharged from January 1, 2004 to June 30th, 2012 which are the most complete data available in the PHIS database. Patients were included if they had an International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code for acute febrile mucocutaneous lymph node syndrome (446.1), received IVIG therapy, and were <19 years of age. Hospitals were excluded if they did not submit data each year of entire study period or had missing or incomplete data. If patients were admitted multiple times, the first admission was used.
Patients were considered to have IVIG-resistant KD if they received an initial dose of IVIG and a subsequent dose of IVIG, methylprednisolone, rituximab, or infliximab ≥2 days after the initial IVIG dose [12]. Additionally, patients were considered to be resistant to IVIG if they were readmitted within 7 days and received a dose of IVIG, methylprednisolone, rituximab, or infliximab on the readmission.
Data collection included patient demographics, hospital, primary attending physician and consult service, length of stay, medications, laboratory utilization, readmission, echocardiography, and mortality. Patterns of resistance at individual hospitals were described. The hospitals were divided into quartiles and hospitals in the quartile with the lowest incidence of resistance (low resistance) were compared to hospitals in the quartile with the highest incidence of resistance (high resistant). Trends in IVIG resistance were evaluated over time using a statistical process control (SPC) chart to determine variations in resistance patterns. Resistance was also evaluated over seasons. Mean and standard deviation were used for normally distributed data and median and interquartile range (IQR) was used for non-parametric data. Student’s t test, Mann–Whitney U test, and Fisher’s exact test were used to determine differences in patient characteristics between high-resistance and low-resistance hospitals. Analysis was performed with Chart Runner (PQ systems, Dayton, Ohio) and Stata IC v.12 (StataCorp, College Station, Texas). A p value of <0.05 was determined a priori as significant.
Results
A total of 9,721 patients met study criteria from 33 hospitals. Median patient age was 2.7 years (IQR 1.4–4.7 years), 60.7 % were male, and most patients were Caucasian (51.6 %). Patient length of stay was a median of 3 days (IQR 2–4 days), 6.9 % were admitted to an intensive care unit, and mortality was <0.1 %. A procedure code for echocardiography was present in 93.6 % of patients. Aspirin was used in 89.9 %, and corticosteroids (5.5 %), infliximab (1.1 %), warfarin (0.7 %), clopidogrel (0.4 %), pentoxifylline (0.3 %), abciximab (0.05 %), and rituximab (0.01 %) were also used. Incidence of readmission within 7 days for retreatment was 3.2 %.
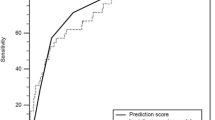
The overall incidence of IVIG resistance was 16.3 %. No increasing trends in resistance to IVIG over time were identified in a statistical process control chart using process stability rules. (Fig. 1) Resistance patterns varied significantly among hospitals from 8.0 to 26.8 % (p < 0.05) (Fig. 2). There was no association with hospitals with a high number of patients admitted with KD and percentage of patients resistant to IVIG (Fig. 3).
Eight hospitals with the lowest incidence of resistance (lowest quartile) were compared to eight hospitals with the highest incidence of resistance (highest quartile) to assess for differences in patient or hospital characteristics. Low-resistance hospitals had a mean incidence of resistance of 10.8 ± 0.3 % compared to high-resistance hospitals, 22.1 ± 0.4 % (p < 0.01). No differences were noted in age or gender between high and low-resistance hospitals, but African-American patients were more prevalent at high-resistance hospitals (Table 1). Patients admitted to hospitals in the highest quartile for IVIG resistance were more likely to have been readmitted for therapy (3.7 vs 5.7 %, p < 0.01). There was not a significant difference in intensive care unit admission (5.3 vs 5.3 %, p = 0.96).
Aspirin was less frequently used at low-resistance hospitals as compared to high-resistance hospitals (89.3 vs 90.2 %, p < 0.01). Patients at a high-resistance hospital were more likely to receive corticosteroid, and were more likely to have salicylate level monitoring (2.0 vs 7.3 %, p < 0.01), but were less likely to have received infliximab (Table 1).
Although the difference is small, echocardiograms were performed more often in patients at low-resistance hospitals as compared to high-resistance hospitals (97.1 vs 93.6 %, p < 0.01). At low-resistance hospitals, fewer patients had a C-reactive protein drawn (79.9 vs 93.0 %, p < 0.01) but more had an erythrocyte sedimentation rate drawn (91.6 vs 87.9 %, p < 0.01).
Discussion
This is largest evaluation regarding the epidemiology of IVIG-resistant KD. Resistance to IVIG has been well documented, and the overall incidence data presented here reflect previous reports from national and local databases [2, 8, 12]. African-American patients were more prevalent at high-resistance hospitals, which differs from previous publications [9].
Overall, our findings demonstrate that IVIG resistance is not uniform throughout pediatric hospitals in the United States. Due to the similarities in the patient data extracted, and the lack of a significant trend of resistance over time, we postulate that these differences may occur due to variation in evaluation and treatment of KD, and, subsequently the diagnosis and treatment of IVIG-resistant KD, at pediatric hospitals.
The diagnosis of KD can be difficult, and increased diagnosis of incomplete KD after guideline publication has been noted [4]. Similarly, guidelines for the diagnosis and treatment of KD may be followed in varying degrees and may be highly dependent on institutional practices [6]. Additionally, patients diagnosed with KD could have atypical KD, and would have a different disease progression and, presumably, differing resistance rates. If the threshold for diagnosing patients with KD is low, many patients who do not have KD could be inappropriately administered IVIG, thus inflating the denominator of patients diagnosed with KD who may not truly have it in our study, and reducing the percentage of patients identified as IVIG resistant.
Other common modalities for evaluation of KD in low- versus high-resistance hospitals demonstrated some significant differences. An echocardiogram was more likely to be performed in a low-resistance hospital. The discrepancy in C-reactive protein and erythrocyte sedimentation rate utilization is important to note, as current guidelines recommend the utilization of both modalities when diagnosing KD [8]. The difference in laboratory testing lends support to the theory that evaluation and thus diagnosis of KD is highly variable at pediatric hospitals.
Other sources of variation may be present that represent institutional biases in the treatment of KD, but are unable to be evaluated using this data source. Medication dose or brand of IVIG is not present in the database, nor are important variables such as presence of fever, length of febrile illness prior to treatment, physical signs and symptoms, or pertinent laboratory values. These are limitations associated with a retrospective review of administrative data. Based on the data presented, we propose that variability in KD diagnosis and overtreatment with IVIG may be the etiology of resistance patterns demonstrated in this report. Due to the lack of granularity associated with a large database study, we are unable to evaluate the etiology of the resistance, and are only able to postulate a question for future investigation. Clinicians are urged to evaluate practices regarding the diagnosis of KD and IVIG therapy at their institution.
Conclusion
Kawasaki disease resistant to intravenous immunoglobulin therapy occurs frequently and the incidence of resistance varies significantly between pediatric hospitals.
Abbreviations
- KD:
-
Kawasaki disease
- IVIG:
-
Intravenous immunoglobulin
- IQR:
-
Interquartile range
References
Burns JC, Capparelli EV, Brown JA, Newburger JW, Glode MP (1998) Intravenous gamma-globulin treatment and retreatment in Kawasaki disease. US/Canadian Kawasaki Syndrome Study Group. Pediatr Infect Dis J 17(12):1144–1148
Chang RK (2002) Epidemiologic characteristics of children hospitalized for Kawasaki disease in California. Pediatr Infect Dis J 21(12):1150–1155
Fukunishi M, Kikkawa M, Hamana K et al (2000) Prediction of non-responsiveness to intravenous high-dose gamma-globulin therapy in patients with Kawasaki disease at onset. J Pediatr 137(2):172–176
Ghelani SJ, Sable C, Wiedermann BL, Spurney CF (2012) Increased incidence of incomplete Kawasaki disease at a pediatric hospital after publication of the 2004 American Heart Association guidelines. Pediatr Cardiol 33(7):1097–1103
Hwang JY, Lee KY, Rhim JW et al (2011) Assessment of intravenous immunoglobulin non-responders in Kawasaki disease. Arch Dis Child 96(11):1088–1090
Kahwaji IY, Connuck DM, Tafari N, Dahdah NS (2002) A national survey on the pediatric cardiologist’s clinical approach for patients with Kawasaki disease. Pediatr Cardiol 23(6):639–646
Kobayashi T, Inoue Y, Takeuchi K et al (2006) Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation 113(22):2606–2612
Newburger JW, Takahashi M, Gerber MA et al (2004) Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 114(6):1708–1733
Porcalla AR, Sable CA, Patel KM, Martin GR, Singh N (2005) The epidemiology of Kawasaki disease in an urban hospital: does African American race protect against coronary artery aneurysms? Pediatr Cardiol 26(6):775–781
Seki M, Kobayashi T, Kobayashi T et al (2011) External validation of a risk score to predict intravenous immunoglobulin resistance in patients with kawasaki disease. Pediatr Infect Dis J 30(2):145–147
Sittiwangkul R, Pongprot Y, Silvilairat S, Phornphutkul C (2006) Management and outcome of intravenous gammaglobulin-resistant Kawasaki disease. Singap Med J 47(9):780–784
Son MB, Gauvreau K, Ma L et al (2009) Treatment of Kawasaki disease: analysis of 27 US pediatric hospitals from 2001 to 2006. Pediatrics 124(1):1–8
Son MB, Gauvreau K, Burns JC et al (2011) Infliximab for intravenous immunoglobulin resistance in Kawasaki disease: a retrospective study. J Pediatr 158(4):644–649
Tremoulet AH, Best BM, Song S et al (2008) Resistance to intravenous immunoglobulin in children with Kawasaki disease. J Pediatr 153(1):117–121
Disclosure
The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moffett, B.S., Syblik, D., Denfield, S. et al. Epidemiology of Immunoglobulin Resistant Kawasaki Disease: Results from a Large, National Database. Pediatr Cardiol 36, 374–378 (2015). https://doi.org/10.1007/s00246-014-1016-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-014-1016-1