Abstract
The outcome for children with pulmonary vein atresia has been historically poor. This report describes clinical outcomes after surgical treatment of primary and secondary pulmonary vein atresia. All patients undergoing surgery for pulmonary vein atresia at Children’s Hospital Boston from 1 January 2005 to 1 January 2009 were identified. The data available for analysis included demographic characteristics, findings based on cardiac catheterization and other imaging, clinical information, operative surgical intervention, and pulmonary vein histology. The study-specific information included the calculated number of atretic pulmonary veins as well as surgical interventions performed during the study period. The study end points included successful relief of pulmonary vein atresia, recurrence of pulmonary atresia or stenosis, overall pulmonary vein disease progression, and patient survival. A total of 16 patients with one or more pulmonary vein atresias were identified in the cardiac surgery registry database. Of these 16 patients, 5 had primary pulmonary atresia, and 11 had secondary atresia after repair of anomalous pulmonary venous drainage. Surgical recanalization of atretic pulmonary veins was achieved for more than 80% of the patients. At the most recent follow-up assessment, 7 (44%) of the 16 patients had recurrence of atresia. Five of the patients had development of new atresia in other previously healthy pulmonary veins. The median follow-up period was 4 months for primary and 17 months for secondary pulmonary vein atresia. The three main predictors of pulmonary vein disease progression after surgery were the presence of underlying lung disease (P = 0.036), prematurity (P = 0.035), and a history of recurrent pulmonary vein atresia. The overall mortality rate for the patients with primary or secondary pulmonary vein atresia was 56% at the most recent follow-up assessment (100% for the patients with primary vein atresia and 36% for the patients with secondary vein atresia). Conclusions: Surgical recanalization of pulmonary vein atresia is possible, but prognosis remains poor. Recurrence of atresia can take place as early as a few months in the presence of underlying lung disease, prematurity, or history of recurrent pulmonary vein atresia. Further research is needed to identify mechanisms for attaining and sustaining pulmonary vein patency after surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary vein atresia (PVA) with or without an anomalous venous connection is rare and generally leads to progressive pulmonary hypertension and cardiac failure in infancy [1, 2]. Traditionally, this has been associated with a high case fatality rate due to a malignant obliterative disease biology refractory to available therapeutic methods [3, 4]. The existing therapeutic methods for pulmonary vein stenosis (PVS) include catheter intervention with or without cutting balloon angioplasty and stent deployment. This study aimed to determine the results of surgical intervention outcomes for PVA at Children’s Hospital Boston.
Methods
Patients
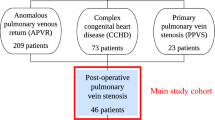
All patients undergoing pulmonary vein surgery for at least one atretic pulmonary vein at Children’s Hospital Boston from 1 January 2005 to 1 January 2009 were identified. All patients undergoing initial surgery for PVA had mild, moderate, or severe pulmonary vein disease in one or more of their other pulmonary veins in addition to at least one atretic pulmonary vein.
Patient data gathered for the study included demographic characteristics, radiologic information, catheter findings, clinical information, and operative surgical intervention. Surgical outcome involved survival and vein patency at the most recent follow-up assessment. Study-specific information included the number of atretic pulmonary veins and the interventions performed during the study period.
We divided the patients into two categories based on the type of pulmonary vein disease: PVA and no significant underlying congenital heart disease [primary pulmonary vein atresia (PPVA)] or PVA after anomalous pulmonary venous drainage repair [secondary pulmonary vein atresia (SPVA)]. The PPVA group contained patients who had either isolated vein atresia with no underlying heart or lung disease or vein atresia with underlying lung disease (e.g., bronchopulmonary dysplasia).
We defined PVA as complete obliteration of the luminal contour extending more than 5 mm within at least one vessel segment on computed tomographic (CT) angiography or catheterization or as no demonstrable flow signal on echocardiography. Nuclear lung perfusion scan was performed for 69% of the patients (8 of 11 SPVA patients and 3 of 5 PPVA patients) pre- and postoperatively as an adjunct assessment procedure (Fig. 1a).
a Preoperative pulmonary vein disease and its respective nuclear medicine lung perfusion scan. Black areas represent the site and schematic extent of the stenosis. Pulmonary vein atresia is depicted by complete obliteration (black color) shown for the right upper, right lower, and left lingual pulmonary veins. The number above each lung zone shows the percentage of perfusion to each lung. The pulmonary vein disease is present bilaterally. The perfusion to the right lung is 15%, reflecting low perfusion in the right lung compared with the left lung. b Postoperative scheme of pulmonary vein disease with its respective lung perfusion scan. Postoperative relief for atresia of the right upper and lower pulmonary veins is seen, with improvement of the lung perfusion scan to 40% on the right side. However, recurrent atresia of the left lingular pulmonary vein is depicted by complete blockage of this vein and the development of collateral circulation to maintain lung perfusion on the left side
Patients were classified as having recurrence when atresia developed in a previously atretic pulmonary vein that had been successfully recalanalized. We classified PVA that developed after cardiac repair as “secondary pulmonary vein atresia.” “Bilateral disease” was characterized by atresia of at least one pulmonary vein draining from both the left and right lungs. We defined “disease progression” as worsening stenosis for at least two of the pulmonary veins ranging from mild stenosis (<35% narrowing of the luminal contour) or moderate stenosis (35 to <70% narrowing) to either severe stenosis (70% narrowing) or near/complete atresia (100% obliteration of the luminal contour) measured at the last follow-up assessment.
Surgical Technique
All procedures were performed via a median sternotomy with cardiopulmonary bypass through cannulas in the ascending aorta, one vena cava, or both vena cavae. Deep hypothermic circulatory arrest or low-flow hypothermic bypass was used to maximize exposure of the retrocardiac anatomy incorporating the veno-left atrial junction. We also adopted a variety of techniques that were used as needed. These techniques encompassed end arterectomy of the thickened endothelial layer of pulmonary vein or left atrium, resection of the localized stenotic area, unroofing of the pulmonary vein, and intraoperative pulmonary vein dilatation with graduated expandable balloons by the surgeon.
Often with atretic veins, the original lumen is difficult to find. Thus, surgical debridement cannot be undertaken without serious risk of full-thickness injury. Finding the correct pathway leading to the native pulmonary vein lumen often was facilitated by initial gentle passage of a guidewire followed by serial dilation with graduated intraoperative balloon angioplasty. The latter split the diseased layers, rendering further debridement easier and safer. If access to the retrocardiac pulmonary vein was cumbersome, exposure was further facilitated by transection of the inferior vena cava.
Each of the aforementioned techniques was tailored to each individual patient’s pulmonary vein anatomy. For most patients, the sutureless technique of choice was the pericardial flap procedure for the right-sided veins and left atrial appendage flap technique for the left-sided veins. With the pericardial flap technique, the mobilized portion of the pericardium serves as the hemostatic roof for the incised veins. The pericardial edge is anastomosed just distal to the incised veins, hence the term “sutureless.” The left atrial flap approach is similar to the original pericardial flap procedure but advances a flap of the left atrium and the left atrial appendage over the incised pulmonary veins to achieve hemostasis. Biopsies were taken from each vein and labeled appropriately for frozen section and staining.
Baseline and Follow-up Studies
Patients presenting with a diagnosis of PVS underwent baseline echocardiography and a nuclear lung perfusion scan. We used CT angiography primarily to determine the extent of disease progression in the distal vessels and the lungs. This was performed with the assistance of the cardiac anesthesia service for sedation or general anesthesia, with intubation depending on the age and clinical status of the patient. The clinical decision was based on a multidisciplinary team meeting, and a choice for relief of PVA or PVS was made. Surgical therapy was considered when catheter-based intervention was deemed either unsuccessful or of limited value.
After relief of PVA or PVS, repeat catheterization was performed approximately 2 to 3 months later to determine disease progression. At 6 months, all patients had sedated echocardiography, nuclear lung perfusion scan, and CT angiography.
Intraoperatively PVA or PVS biopsies were labeled anatomically. Each specimen was submitted for a standard staining panel including hematoxylin and eosin (H&E; Masson Trichrome, Alcian Blue, pH 2.5; Miller’s Elastic). When indicated, tissues were examined with immunohistochemical markers for platelet-derived growth factor receptor beta (PDGFR-β), phosphorylated PDGFR-β, and vascular endothelial growth factor receptor 2 (VEGFR-2).
Further management in the form of chemotherapy was based on multidisciplinary meetings. Each case was discussed, and patients with multivessel pulmonary vein disease (involvement of at least two pulmonary veins) and tissue biopsy consistent with the presence of myofibroblast proliferation were offered medical management using chemotherapeutic agents as an adjunct to anatomic palliation with surgery, catheter-based interventions, or both.
The choice of the physician or parents, the innovative and experimental nature of the treatment, and the lack of insurance coverage were some of the limiting factors for enrollment in this treatment strategy. If the parents decided to enroll (for vinblastine and methotrexate using the previous protocol or Avastin and/or Gleevec with innovative use or a new protocol), they gave their consent, and treatment was initiated.
Before initiation of treatment, laboratory tests to ensure normal organ function were performed. During treatment, patients had regular oncology follow-up evaluations with laboratory tests to assess drug safety, monthly cardiology follow-up evaluations with sedated echocardiography and lung perfusion scan, and 6-month CT angiography to evaluate the status of pulmonary veins. If at any time during the follow-up evaluations patients showed clinical or radiologic signs of disease recurrence, they were discussed further in our multidisciplinary meetings. The multidisciplinary team assessed patients 12 months after treatment, and the decision was made with the parents either to hold or to continue the treatment based on efficacy and safety of the treatment.
Statistical Analysis
Patient characteristics were summarized using number (%) for categorical variables and median (range) for continuous variables. Summaries were performed for the entire group of patients and also separately for those with PPVA versus SPVA. Comparisons of characteristics between patients who did and did not experience disease progression were performed using Fisher’s exact test.
Results
Patient Cohort
A total of 16 patients with one or more atretic pulmonary veins who underwent surgical treatment were identified. In this group, 11 patients had PVA secondary to underlying congenital heart disease, and 5 patients had PPVA with or without lung disease (Table 1). The PVS treatment interventions at the time of surgery to relieve pulmonary vein disease are summarized in Table 2.
PPVA
Four of five patients with one or more PPVAs underwent surgical treatment and achieved early patency of their atretic veins. All four of these patients had systemic or suprasystemic right ventricle pressure (RVp) preoperatively. None of the patients showed vein patency at their most recent follow-up assessments. Interestingly, two patients experienced PVA in previously healthy patent veins. Immediate RVp after pulmonary vein surgery was slightly lowered in all four patients (>50 to 80% systemic). All the patients except one received chemotherapy for positive myofibroblasts in the pulmonary vein biopsy specimens. The one patient eligible for treatment did not receive chemotherapy per the parent’s decision.
SPVA
Of the 16 patients, 11 presented with SPVA after cardiac surgery. The total number of atretic pulmonary veins was 22. During a median follow-up period of 17 months (range, 1–41 months), nine of the patients (85%) maintained patency (without atresia recurrence) of previously atretic pulmonary veins after surgical therapy. Three of the patients acquired new PVA after surgery. Of the 11 patients, 2 could not achieve surgical patency of their atretic veins and had no benefit from surgery, whereas 7 had biopsy results positive for myofibroblasts, 5 of whom were treated with chemotherapy. One of two patients with positive histology results was enrolled in the chemotherapy protocol but died before initiation of chemotherapy. The remaining patient did not start treatment per the parent’s choice.
Four patients had near systemic preoperative RVp. Postoperatively, they achieved RVp of half systemic pressure or less. One patient had some improvement in RVp to two-thirds systemic pressure, whereas others remained either systemic or suprasystemic, as shown at the last follow-up visit. At this writing, seven patients (64%) in this subgroup are still alive, and four of them have achieved a decrease in RVp to half systemic pressure. Chemotherapy was used for three of these seven survivors. Among the four deceased patients who had RVp higher than two-thirds systemic pressure, two patients had received chemotherapy and lived for 8 and 13 months.
Autopsy and Histologic Results
Autopsies were available for 4 of the 9 patients who died among the total of 16 patients. Three patients had findings confirming prior imaging of PVA and severe pulmonary artery hypertensive changes. One patient had abnormal lung parenchyma formation, microcystic changes, and scattered pulmonary infarcts. One patient had diffuse alveolar injury with widespread bronchopulmonary pneumonia together with multifocal lung infarcts. In one patient who underwent lung transplantation, the explanted lungs demonstrated pulmonary venous hypertensive changes proximal to the stenosis, most marked in the lower lobes. Pulmonary arterial histopathology consisted of significant medial layer hypertrophy associated with scarring, intimal fibromyxoid proliferation, and luminal narrowing. The cause of death for the bilateral lung transplant recipient was severe primary graft failure.
Of the 16 patients, 12 (all with PPVA and 7 with SPVA) had evidence of myofibroblast proliferation shown by surgical biopsy or autopsy. Two of the myofibroblast-negative patients had definitive signs of mild intimal proliferation with fibrous and elastic tissue on surgical biopsy specimens, but the other two, despite intimal proliferation, had evidence of fibromyxoid change. The final two patients had recurrent PVS, and none of the myofibroblast-negative patients received chemotherapy.
Disease Progression
Of the 16 patients, 6 experienced disease progression of their previously atretic veins during the follow-up period. The patient pathophysiologic and operative variables associated with disease progression were single- versus multiple-vein disease, pulmonary artery pressure after pulmonary vein surgery (greater than or less than systemic pressure), presence or absence of myofibroblasts, use of different surgical techniques (sutureless repair, intraoperative balloon), pre- and postoperative catheter-based interventions, proof of immediate postoperative vein patency, bilateral versus unilateral pulmonary vein disease, use of chemotherapy, presence of associated congenital heart defects, and recurrence of PVA among surgically treated patients. The statistically significant factors found to be associated with worsening pulmonary vein disease were presence of underlying lung disease, prematurity, and recurrence of PVA after initial surgical relief (Table 3).
Discussion
Although rare, PVS and PVA are relentless [1]. When the disease becomes progressive, leading to complete obstruction of more than one vessel, the prognosis is very poor [1]. Historically, surgical mortality associated with relief of individual PVA has approached 100%. Usually, PVA is refractory to all forms of surgical or catheter-based intervention. The condition can occur as a complicating feature of complex congenital heart disease, but it also can occur as a primary disease in isolation in infants with otherwise normal hearts. The case fatality and recurrence rates for the PPVA type are higher than for SPVA [3, 4].
In a recent study using the Pediatric Cardiac Care Consortium database, 31 patients had PVS, and approximately 50% underwent intervention to relieve PVS. The study end points were lung death or transplantation. The authors found that when PVS was diagnosed at the age of 18 months with an initial mean pulmonary arterial pressure greater than 33 mmHg or with bilateral vessel involvement, the risk of death rose to more than 75% [4].
Several hypotheses have been postulated to explain the processes behind PVS and PVA. These include but are not limited to alteration in size, structure, and function of the vein; abnormal shear stress on the vein endothelium due to differential flow or pressure perturbances; inherent reduction in the caliber of the vein with changes in the structure; and cellular expression of the vessel wall [5–7]. Among these hypotheses, the latter has attracted the most interest with respect to clinical patient management.
Unusual myofibroblastic cells have been found in primary PVS. These cells have phenotypic features of both fibroblasts and smooth muscle cells [8]. They are capable of differentiating into either fibroblasts or smooth muscle cells, but the main trigger for such has not been isolated. Receptor tyrosine kinases such as PDGFR and VEGFR found recently on myofibroblast membranes are considered as possibly playing a role in the pathogenesis of the disease.
Ample literature describes the natural history of PVS after repair of total anomalous pulmonary vein connection, but case reports and subgroup analysis of PVA are scarce. A study by Yun et al. [9] from the University of Toronto found that among 60 patients who underwent operative intervention for PVS, only 5 patients had PVA. Three of these patients died 2 to 4 months after surgery, and at the end of the follow-up period, only one patient (20%) had achieved long term patency. Because PVA patients have such a dismal long-term prognosis, we elected to focus on these patients as part of a comprehensive review examining surgical management of PVS at our institution.
Our current goal for most of these patients was to relieve any PVA in a multidisciplinary fashion incorporating surgical, catheter-based interventions, and chemotherapy. The latter specifically targets the myofibroblast. Since 2005, we have used nuclear medicine lung scan, CT angiography, and cardiac catheterization to better characterize patients with PVA. These imaging methods provide further information beyond two-dimensional echocardiography in delineating both the extent and the severity of PVA.
For proximal atresia (obliteration of the pulmonary vein lumen near the left atrial junction), we recommend surgery after an initial catheter-based intervention has failed to achieve vein patency. Distal vessel disease beyond second-order pulmonary vein tributaries or outer lung parenchyma is mostly not amenable to anatomic palliation with either surgery or catheter intervention. Lung or heart–lung transplantation may be the only means for managing this rapidly progressive disease. Medical management with experimental chemotherapeutic agents may be beneficial, especially for the distal vessel disease.
We also have adopted a variety of surgical techniques including endarterectomy, incision into an atretic vein, patch augmentation of the atrium, pericardial vein patching, and resection of discrete narrowed vein orifice. Each of these techniques were tailored to individual pulmonary vein disease at the discretion of the surgeon. However, the sutureless repair has been the mainstay surgical procedure of choice when feasible. Biopsies were labeled appropriately and sent from each pulmonary vein to histopathology at the time of surgery.
Furthermore, extrapolating from percutaneous vein angioplasty, we used intraoperative balloon angioplasty. Under direct vision, inflation of the balloon with a predetermined size to the appropriate vein diameter achieves necessary equal distribution of radial forces and stress throughout the vein to show where the true lumen is and hopefully sustain patency. This is particularly useful for long-segment atresia or stenosis, in which the true lumen is difficult to determine. Before leaving the operating room, we measured RVp after surgical repair, directly with needle puncture of the right ventricle or indirectly with echocardiography.
Although a significant reduction in pulmonary artery pressure was associated with relief of PVA, the number of our patients was too small to determine correlation and assign an absolute RVp as a predictor of disease progression after surgical relief.
Patients are followed carefully and reimaged with a nuclear medicine scan before discharge and 4 to 6 weeks postoperatively. Under the discretion of the primary cardiology team, patients with multivessel PVS and biopsy results positive for myofibroblasts are offered the option of chemotherapy. Treatment is started after informed consent is obtained from the family (as detailed in the Methods section). Should there be any level of recurrence or progressive narrowing, our first step is to apply balloon dilation or cutting balloon therapy [1]. We strongly believe that repeat interventions may slow the progression of restenosis. Stent deployment is used if balloon dilation fails to achieve satisfactory patency and surgery is unlikely to be of any further benefit.
In our study, immediate surgical relief of PVA was achieved for more than 80% of the patients. Disease progression, defined as stenosis or atresia of the pulmonary vein after surgery, was observed in one-third of the patients, and a slightly more than half of the patients were deceased at follow-up evaluation. The presence of underlying lung disease, prematurity, and history of recurring pulmonary vein atresia after surgical relief were associated with disease progression. Although others have found prematurity and low birth weight to be associated with PVS [2], we did not observe this. However, our population sample was small, and large sample studies need to be conducted. The mechanisms underlying this disease remain obscure and were not the focus of this study.
Although the overall survival rates found at the most recent follow-up assessment are low compared with those for other congenital heart defects, this is not unexpected. The cause of death for most patients is respiratory failure due to relentless pulmonary hypertension complicated by pneumonia or hemoptysis.
Without treatment, patients with PVA have an extremely poor prognosis, and lung transplantation is the only and last surgical option. Only one patient in our study received bilateral lung transplantation and survived for 1 month. This patient’s cause of death was acute rejection and primary graft dysfunction. Given the known limitations of lung transplantation including donor availability, variable recipient waiting time, and the known complications of immunosupression, any treatment that could improve survival by alleviating pulmonary vein disease is highly sought after. We adopted a multidisciplinary approach that involves contemporary surgical vein repair, catheter-based intervention, and more recently, chemotherapy. With better understanding of the basic science and pathophysiology of the pulmonary vein wall, we will be able to target better both known and unknown culprits involved in this highly morbid and mortal disease.
References
Driscoll DJ, Hesslein PS, Mullins CE (1982) Congenital stenosis of individual pulmonary veins: clinical spectrum and unsuccessful treatment by transvenous balloon dilation. Am J Cardiol 49:1767–1772
Drossner DM, Kim DW, Maher KO, Mahle WT (2008) Pulmonary vein stenosis: prematurity and associated conditions. Pediatrics 122:e656–e661
Fong LV, Anderson RH, Park SC, Zuberbuhler JR (1988) Morphologic features of stenosis of the pulmonary veins. Am J Cardiol 62:1136–1138
Holt DB, Moller JH, Larson S, Johnson MC (2007) Primary pulmonary vein stenosis. Am J Cardiol 99:568–572
Jenkins KJ, Sanders SP, Orav EJ, Coleman EA, Mayer JE Jr, Colan SD (1993) Individual pulmonary vein size and survival in infants with totally anomalous pulmonary venous connection. J Am Coll Cardiol 22:207
Riedlinger WF, Juraszek AL, Jenkins KJ, Nugent AW, Balasubramanian S, Calicchio ML, Kieran MW, Collins T (2006) Pulmonary vein stenosis: expression of receptor tyrosine kinases by lesional cells. Cardiovasc Pathol 15:91–99
Sun CC, Doyle T, Ringel RE (1995) Pulmonary vein stenosis. Hum Pathol 26:880–886
Latson LA, Prieto LR (2007) Congenital and acquired pulmonary vein stenosis. Circulation 115:103–108
Yun TJ, Coles JG, Konstantinov IE, Al-Radi OO, Wald RM, Guerra V, de Oliveira NC, Van Arsdell GS, Williams WG, Smallhorn J, Caldarone CA (2005) Conventional and sutureless techniques for management of the pulmonary veins: evolution of indications from postrepair pulmonary vein stenosis to primary pulmonary vein anomalies. J Thorac Cardiovasc Surg 129:167–174
Acknowledgment
We thank Dr. Gauvreau for her help and guidance with univariate analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shuhaiber, J., Rehman, M., Jenkins, K. et al. The Role of Surgical Therapy for Pulmonary Vein Atresia in Childhood. Pediatr Cardiol 32, 639–645 (2011). https://doi.org/10.1007/s00246-011-9942-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-011-9942-7